1 May 2017
Laura Quiney and Sue Dyson look at a variety of recent research undertaken on both the aetiology and detection of horses presenting as lame.
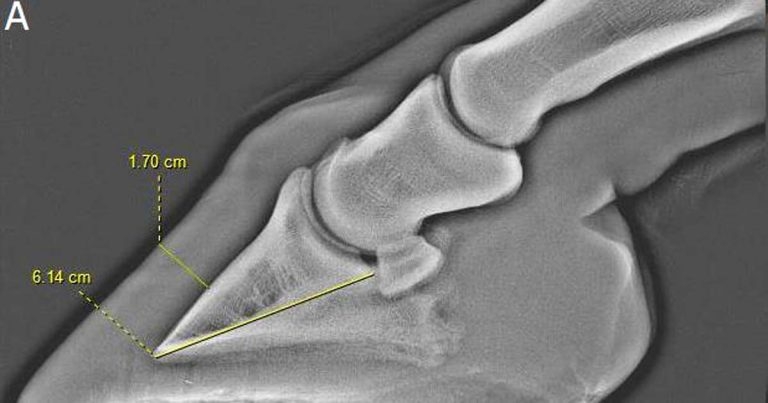
Figure 1. Lateromedial radiographs of the front feet of an 11-year-old Connemara-cross gelding. The horse was overweight and short stepping in front when ridden. Bilateral perineural analgesia of the palmar nerves (at the base of the proximal sesamoid bones) resulted in marked improvement in the forelimb step length. 1a. The left front foot. The hoof distal phalanx distance to palmar length of the distal phalanx ratio was 27.7 per cent. 1b. The right front foot. The hoof distal phalanx distance to palmar length of the distal phalanx ratio was 27.4 per cent. Mild modelling at the toe of the distal phalanx is apparent. In both feet, loss of the normal radiolucent halo around the distal phalanx in the toe region and mild distal rotation of the distal phalanx occurred. The radiographic findings are suggestive of laminar pathology and it was concluded this horse had atypical laminitis – most likely as a result of abnormal bodyweight and insulin resistance.
This article aims to review some of the recent literature that has advanced our knowledge and understanding of the causes of lameness or its diagnosis.
Laminitis is a debilitating disease and, over the past decade, an increasing amount of research has improved our understanding of potential risk factors.

Menzies-Gow et al (2017) performed a prospective cohort study in which risk factors for the development of laminitis were assessed in a group of 446 horses without a history of previous laminitis. Physical observations and biochemical values were acquired at the start of the study, and the horses were followed over three years.
Obesity was common (72.2%); however, in the final multivariable model, this was surprisingly not a risk factor for the development of laminitis. Risk factors included low plasma adiponectin, high basal insulin and high post-dexamethasone insulin levels. Further prospective studies would be necessary to determine the fluctuation and inter-relationship of these biochemical markers prior to a laminitis episode.
A perceived risk of iatrogenic laminitis exists following glucocorticoid administration. Previous reports of the development of laminitis following corticosteroid administration (including prednisolone, dexamethasone and triamcinolone) either lacked a control group or were limited to case reports. Jordan et al (2016) conducted a retrospective case-control study to determine the incidence of laminitis in a group of 416 horses treated with oral prednisolone, compared with time-matched controls (two controls per case).
No significant difference (p=0.8) occurred between the incidence rates of laminitis in the two groups (treated group = 2.6, control group = 3.46). Of the horses subjected to euthanasia as a result of laminitis, no association existed between mortality and prednisolone administration. Increasing age, underlying endocrinopathy and a previous history of laminitis were identified as potential risk factors on univariable analysis. Equine metabolic syndrome and increasing age were the risk factors identified on multivariable analysis. Prednisolone administration was not identified as a risk factor in this study.
In an abstract, the findings of a prospective cohort study involving 889 horses administered corticosteroids over 13 months were described (Potter et al, 2016). The prevalence of laminitis was 0.6% (5 out of 889 horses).
Development of laminitis was not associated with either the type of corticosteroid or the route of administration. A significant association (p<0.001) was apparent between breed, previous laminitis and underlying endocrinopathy with the development of laminitis during the study period.
Both of these studies indicate, contrary to the widely held belief, administration of corticosteroids does not appear to increase the risk of developing laminitis. However, this may also be a reflection of the low frequency of occurrence of corticosteroid-associated laminitis, the doses administered and the presence of other concurrent risk factors.
Radiographic assessment of the dorsal hoof wall in relation to the distal phalanx is important in the evaluation of laminitis. Subclinical laminitis may be under-diagnosed compared with the conventional acute formof disease.
Subclinical laminitis can contribute to poor performance, resulting in loss of extravagance of forelimb movement or a bilaterally shortened forelimb step length. It may be insidious in onset, with radiographic changes associated with the distal phalanx or hoof wall (Figure 1; Mansmann and Castelijns, 2017).
Alteration of the hoof wall in suspected subclinical laminitis has been described in Thoroughbred racehorses (Linford et al, 1993). However, a lack of data exists about subclinical laminitis in sports horses. Mullard et al (2016) retrospectively reviewed lateromedial foot radiographs of 279 horses (415 feet) without a history or clinical signs of typical laminitis. A wide range was apparent in the ratio between the hoof wall distal phalanx distance to the palmar length of the distal phalanx, mean 0.25 plus or minus 0.03 (median 0.25; interquartile range = 0.23 to 0.26; range = 0.19 to 0.36).
Breed, age and height:bodyweight ratio had a significant effect on the ratio, although did not adequately account for the variability in the ratio within this population, which may be associated with subclinical laminitis.
A higher frequency was apparent of modelling of the toe of the distal phalanx in horses in which the ratio was greater than 26%, compared with those where the ratio was less than or equal to 26%. No association existed between dorsal hoof wall thickness and the presence of divergent growth rings on the hoof wall, but no horse had divergence greater than 3mm.
It is generally accepted relatively poor inter-observer agreement for lameness evaluation exists – especially for low-grade or multi-limb lameness. Advances have occurred in the field of objective gait assessment. Pfau et al (2016) assessed 23 horses in hand and when lunged on both soft and hard surfaces. These horses were deemed to be sound by their owners. The results indicated horses that had symmetrical head movement when trotted in a straight line did not show any significant alteration in head movement symmetry when lunged on both reins on both surfaces.
The symmetry of head movements in horses that did have asymmetrical poll movements in a straight line (that is, forelimb lameness) was significantly affected by rein and surface. Rein and surface did not affect pelvic movement symmetry in horses that had either symmetrical or asymmetrical pelvic movement when assessed in a straight line. These results support the observation lameness may change under different circumstances (Dyson and Greve, 2016).
A need exists for more objective movement data on different types of sound horses to assess the influence of exercise under different circumstances on normal horses. Movement characteristics of a small group of 13 sound warmbloods in hand, on the lunge and ridden have been documented (Greve and Dyson, 2016). It is unclear whether objective gait analysis will be able to detect bilaterally symmetrical lameness, ataxia and to differentiate between multilimb lameness and referred lameness.
Horses with lameness may have reduced range of motion of the thoracolumbar region (Greve et al, 2016) and alteration in inclination of the trunk (Greve and Dyson, 2016), adaptations to pain that may make lameness more challenging to detect.
When ridden, there may be other manifestations of lameness, such as an uneven contact through the reins, lack of hindlimb impulsion and conflict behaviour (Dyson, 2016). These are clinical signs of pain causing lameness or poor performance, and commercially available objective gait analysis will not be able to detect these clinical signs. While objective gait analysis is proving to be an important research tool and may be a useful tool for objective assessment of interventions (for example, diagnostic analgesia), its value for lameness detection is questionable. Objective gait assessment in clinical practice should not displace a thorough conventional lameness evaluation.
Diagnostic analgesia is an important diagnostic procedure for horses with lameness or poor performance. The response of a horse to diagnostic analgesia directs diagnostic imaging and diagnosis, the results of which influence the ascribed prognosis. Accurate interpretation is dependent on a thorough knowledge of the potential effects of diagnostic analgesia.
The distribution and diffusion of local anaesthetic solutions depending on volume and injection technique have been questioned for several common sites of perineural or intrasynovial injection. Inconsistent reporting has occurred of the specificity of intrathecal analgesia of the digital flexor tendon sheath (DFTS).
Jordana et al (2016) showed the diffusion of mepivacaine does occur over time (measured 15 minutes and 60 minutes post-injection) from the DFTS into adjacent synovial structures (metacarpophalangeal or metatarsophalangeal joints, proximal interphalangeal joint or distal interphalangeal joint) in anaesthetised horses. The concentrations found were considered by the authors to be below that which would be clinically relevant. However, the minimum concentration of local anaesthetic solution required in a synovial space to produce analgesia is uncertain.
Significantly higher concentrations of local anaesthetic solution were found after 60 minutes, compared with after 15 minutes in the metacarpophalangeal or metatarsophalangeal joints ipsilateral to the injected DFTS. However, no significant difference was apparent in the concentration of local anaesthetic solution in the ipsilateral and contralateral metacarpophalangeal or metatarsophalangeal joints after 15 minutes. While this may indicate insufficient local diffusion for at least up to 15 minutes after injection to provide analgesia of the adjacent fetlock joint (and, therefore, confound interpretation), the effect of weight-bearing and walking is unknown.
There is an old-standing belief perineural analgesia of the palmar digital nerves only affects the sensory innervation of the palmar one-third of the foot. An abstract published by Paz et al (2016) indicated perineural anaesthesia of the palmar digital nerves significantly increased mechanical nociceptive thresholds of the dorsal laminae compared with baseline values (p less than 0.001), as well as the sole and heel bulbs.
Compared with baseline values, perineural anaesthesia of the dorsal branches of the palmar nerves only increased mechanical nociceptive thresholds around the coronary band. This study indicates the innervation of the dorsal laminae is primarily from the palmar digital nerves and the innervation of the coronary band is primarily from the dorsal branches of the palmar nerves.
Malton and Nagy (2016) described the distribution of radiodense contrast medium and methylene blue following injection of a mid-pastern ring block. Greater diffusion was seen when 5ml were injected compared with 2ml. However, proximal diffusion into the proximal 20% of the proximal phalanx was seen when 2ml were injected. Therefore, a dorsal ring block using even a small volume of local anaesthetic solution may desensitise the proximal aspect of the proximal phalanx.
Dissection revealed the palmar digital nerve and dorsal branch were in close proximity in the mid-pastern region (1cm to 1.5cm). Proximal diffusion after perineural analgesia of the palmar digital nerves is influenced by the proximodistal site of injection and volume of injection (Nagy and Malton, 2015). Greater proximal diffusion of radiodense contract medium occurred after injection proximal to the ungular cartilages compared with further distally, and when 2.5ml was injected compared with 1.5ml. It is possible if more than 1.5ml is injected, or a site proximal to the ungular cartilages is used, inadvertent analgesia of the dorsal branches may also occur.
Several approaches to injection of the navicular bursa have been described, mostly from the palmar sagittal aspect, which requires penetration of the deep digital flexor tendon (DDFT). Lateral approaches that avoid the DDFT have been described, although avoidance of the DDFT had not previously been confirmed.
Daniel et al (2016) reported the frequency of DDFT, distal interphalangeal (DIP) joint and DFTS penetration from a radiographically guided lateral approach to the proximal recess of the navicular bursa.
The navicular bursa was successfully penetrated in all 40 cadaver limbs. The dorsal aspect of the DDFT was penetrated in 1 out of 40 limbs. A significant increase occurred in risk of penetration of the DIP joint, if the DIP joint was distended with fluid, and a trend for increased risk of DFTS penetration if distension of the DFTS was present, compared withnormal limbs.
A limitation of this study was MRI to assess needle placement (with the needle in situ) was only performed following correct needle placement as determined by radiography. Therefore, the results only reliably pertain to correct needle placement, and the penetration of structures from incorrect needle placement was not assessed because previous needle tracts could not be identified on MRI.
No reported adverse effects exist as a result of penetration of the DDFT by the commonly used palmar sagittal approach, so no known advantages of avoiding this structure exist either. This study demonstrated the lateral approach appears to be reasonably accurate and this technique could be useful in horses where skin disease or a wound in the heel region makes a palmar sagittal approach contraindicated.
However, penetration of the DIP joint and DFTS was relatively frequent, and this must be borne in mind if a suspicion of sepsis of these synovial structures exists.
Perrin et al (2016) described a novel lateral approach to the navicular bursa using ultrasound guidance.
A 68% success rate occurred (confirmed by the presence of the injected methylene blue solution within the navicular bursa on dissection) when performed by an operator experienced in foot ultrasonography, but who had never injected the navicular bursa under ultrasound guidance. Penetration of adjacent structures and synovial cavities was not assessed.
This technique appears to have moderate success; however, the effect of an operator (including ultrasonography and technique experience) is unknown.

Forelimb lameness only apparent in the ridden horse is sometimes attributed to rider or training error, or poorly fitting tack. However, Dyson and Rasotto (2016) have described an intermittent hopping-type lameness only seen in the ridden horse (Figure 2). It is seen as a shortened cranial phase to the step and marked elevation of the head during protraction of the lame limb at trot, as though the horse is about to break into canter.
This syndrome was first described, by Dyson (2003). In 2014, Dyson published a single case report in print of an event horse investigated for intermittent hopping-type forelimb lameness in which a jagged bone plate was identified between the biceps brachii and brachiocephalicus muscles.
In a study by Dyson and Rasotto (2016), the detailed clinical records of 46 horses identified with the syndrome over a 12-year period were reviewed. Use of different tack, a bitless bridle or a change in rider did not abolish the lameness in any horse in which these changes were made.
Diagnostic analgesia of the affected forelimb did not abolish the hopping-type lameness in any horse, although intra-articular analgesia of the articular process joints of the sixth and seventh cervical vertebrae improved the hopping-type lameness in two of four horses. Deterioration in the hopping-type lameness with progressive diagnostic analgesia was seen in 16 (34.8%) of horses.
Prolonged rest (greater than one year), NSAID administration, complementary therapies (physiotherapy, chiropractic manipulation and acupuncture), continued exercise despite lameness, and medication of the scapulohumeral joint (in two horses with scapulohumeral OA) did not produce long-term alteration in the hopping-type lameness. Of seven horses with OA of the articular process joints between the sixth and seventh cervical vertebrae, which were treated by intra-articular medication with a corticosteroid, three transiently improved.
Treatment with orally administered gabapentin improved the hopping-type lameness in two out of four horses. Postmortem examination revealed lymphocytic infiltration of the dorsal root ganglia of three horses, which may be associated with chronic pain. In one horse, satellite cell hyperplasia was apparent, which may contribute to neuropathic pain. The authors concluded this study adds to the mounting evidence that ridden examination is often essential for both lameness evaluation and pre-purchase examination. Further research to elucidate the cause(s) of this odd forelimb lameness is required.