17 Apr 2023
Equine parasitology: an update on diagnostics and treatment options
Jacqueline Matthews discusses how to test for – and treat – common parasitic infections in horses.

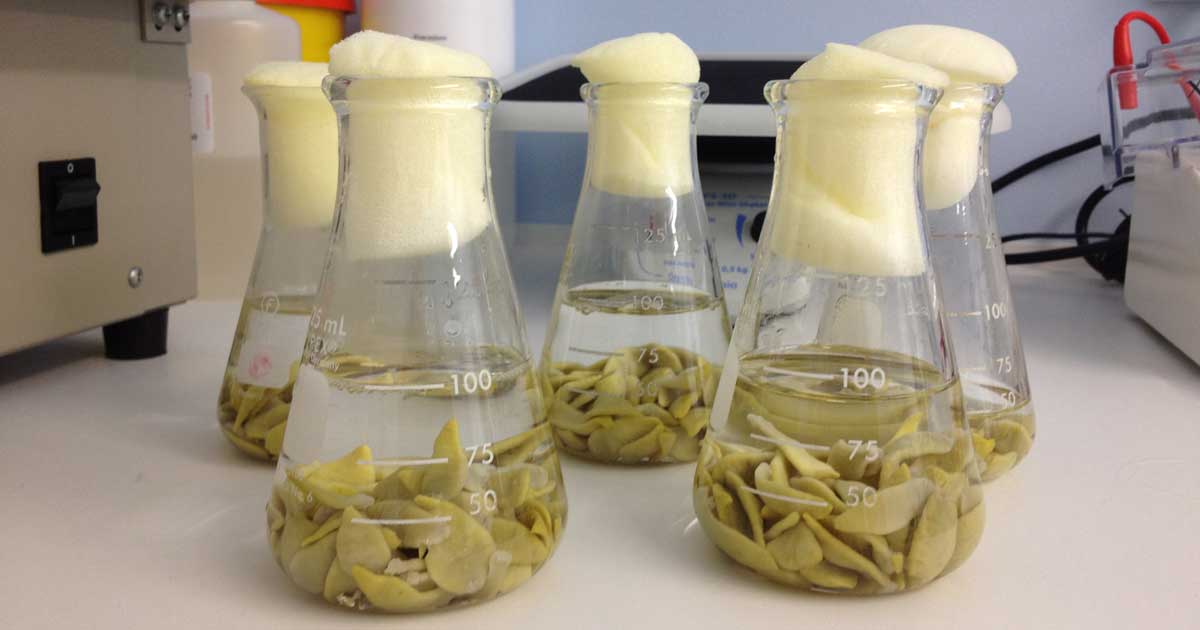
Tapeworms in flasks. Image: Austin Davis Biologics
Nearly all grazing horses are exposed to gastrointestinal helminths. Most show no ill effect of infection, but a small proportion accumulate high burdens and develop disease.
The most common helminths are the cyathostomins (small redworms, small strongyles) and the tapeworm, Anoplocephala perfoliata. Other species found in the UK include the roundworm – Parascaris species, an important parasite of foals – and the pinworm, Oxyuris equi, which can be a persistent problem in some herds.
Historically, the large strongyle, Strongylus vulgaris, was a serious threat due to its potential to cause non-strangulating intestinal infarction; this is found rarely in the UK due to long-term, regular macrocyclic lactone use. This parasite should, however, be considered as a possible emergent threat in herds that have not received this class of anthelmintic for extended periods.
Parasite-associated disease
A small number of horses with high cyathostomin or tapeworm burdens can develop disease.
In the former, horses present with acute larval cyathostominosis, which, in some reports, has a case fatality rate of up to 50%. These have a range of symptoms, most commonly weight loss, diarrhoea and colic (Murphy and Love, 1997).
The syndrome is associated with emergence of substantial numbers of encysted larvae from the large intestinal wall. In temperate regions of the northern hemisphere, larvae usually emerge in large numbers in autumn or winter following a build-up of parasites in horses that have grazed heavily contaminated pasture and have not received effective anthelmintics.
Susceptible horses can amass considerable burdens (tens to several hundred thousand larvae). A perfoliata has been associated with intestinal blockage and colic (Proudman and Trees, 1999). Pathological effects of infection correlate with burden intensity; lesions are generally more severe in horses with more than 20 tapeworms (Proudman and Trees, 1999), but most have low burdens and do not develop disease.
Sustainable helminth control programmes
The aim of sustainable control is to reduce the risk of horses accumulating burdens that result in disease, while addressing the need to mitigate anthelmintic resistance selection (Matthews, 2014).
Overuse of anthelmintics, combined with underdosing, has resulted in widespread resistance (Nielsen, 2022). Because no new anthelmintics are coming to market in the foreseeable future, it is imperative to preserve currently effective drugs by practising evidence-based control.
When designing a programme, it is essential to understand which parasites are present, levels of exposure/infection in a herd, how infection is distributed among individuals and anthelmintic sensitivity. Horses vary in susceptibility; once animals are mature, most regulate burdens well and have low levels of infection. As a result, relatively small numbers of individuals (less than 20%) contribute the bulk of contamination on to grazing (negative binomial distribution).
Diagnostics are key to identifying which parasites are present and which horses harbour higher levels of worms, or are higher worm egg shedders. These animals can then be targeted with specific anthelmintic treatments.
Diagnostics
Faecal egg count analysis
While horses are grazing, treatments should be administered to reduce pasture contamination with nematode (strongyle) eggs. Because of the negative binomial pattern in egg excretion, faecal egg counts (FECs) are invaluable in driving down treatment frequency.
Often, egg excretion patterns of an individual are consistent over time. FECs do not correlate with adult worm numbers, nor do they provide information on pre-patent larvae, so they should be used to direct treatments to reduce egg shedding through spring and summer grazing periods.
FECs can also be used in herds that have significant grazing time in winter, for assessing newcomers, in FEC reduction tests (FECRT) and for calculating strongyle egg reappearance periods (ERPs) after treatment (this is rarely performed in practice due to resource/cost implications).
FECs are useful in foals older than four months when trying to determine the parasite species present that need to be targeted with anthelmintics (such as Parascaris species or cyathostomins, or both species; Table 1). Note that FECs will not detect pinworm eggs, because these adhere to skin in egg packets; these are detectable using a tape test.
| Table 1. Treatment options for equine helminth infections in the UK, taking into account season and the results of diagnostic tests | ||||||||
|---|---|---|---|---|---|---|---|---|
| Time of year |
Action | Faecal egg count (FEC) |
Tapeworm test | Risk assessment: suitability for the small redworm blood test |
Small redworm blood test* | First treatment choice** | Second option | Third option |
| Autumn/winter | Apply treatment for encysted cyathostomins or test in horses in low transmission settings for cyathostomins. Test for tapeworm. |
N/A | Negative | High risk assessment including recent FEC >200 eggs per gram (EPG), poor pasture hygiene*** |
NA | Moxidectin | Five-day fenbendazole only if known sensitivity |
– |
| Low/moderate risk assessment including recent FEC <200 EPG, good pasture hygiene |
Above serum score cut-off for 1,000, 2,000 or 10,000 worms; threshold selected based on clinical assessment |
Moxidectin | Five-day fenbendazole only if known sensitivity |
– | ||||
| Below serum score cut-off for 1,000, 2,000 or 10,000 worms; threshold selected based on clinical assessment |
No anthelmintic required |
– | – | |||||
| Positive | High risk assessment including recent FEC >200 EPG, poor pasture hygiene |
N/A | Moxidectin and praziquantel**** |
– | – | |||
| Positive | Low/moderate risk assessment including recent FEC <200 EPG, good pasture hygiene |
Above serum score cut-off for 1,000, 2,000 or 10,000 worms; threshold selected based on clinical assessment |
Moxidectin and praziquantel |
– | – | |||
| Below serum score cut-off for 1,000, 2,000 or 10,000 worms; threshold selected based on clinical assessment |
Praziquantel | 2× Pyrantel | – | |||||
| Rest of the year | FEC every 6 to 12 weeks, depending on risk of transmission (for example, stocking rate, age profile of horses, dung removal practices). Tapeworm test in spring depending on risk (for example, proportion of horses positive in previous tests, incidence of tapeworms associated disease). |
Negative | Negative | N/A | N/A | No anthelmintic required | – | – |
| Positive (strongyle eggs) |
Ivermectin | Pyrantel (if sensitivity known or treat and FEC reduction test (FECRT once a year) |
Moxidectin | |||||
| Positive (Parascaris eggs, more than four months) |
Fenbendazole (if sensitivity known, or treat and FECRT once a year) |
Pyrantel (if sensitivity known or treat and FECRT once a year) |
– | |||||
| Negative | Positive | Praziquantel | 2× pyrantel | – | ||||
| Positive (strongyle eggs) |
Ivermectin and praziquantel | 2× pyrantel (if cyathostomin sensitivity known or treat and FECRT once a year) |
Moxidectin and praziquantel |
|||||
| Positive (strongyle and Parascaris eggs) |
Pyrantel 2× (if cyathostomin sensitivity known or treat and FECRT once a year) |
Ivermectin and praziquantel (if Parascaris sensitivity known or resistance or treat and FECRT once a year) |
– | |||||
| NA – test not applicable for assessment for treatment options at this time of year or based on horse history. | ||||||||
| *Small redworm blood test only available through veterinary practice, and recommended for use in horses at low and moderate risk of infection with recent FEC <200 EPG grazing on paddocks with dung removal more than once a week when using to inform anthelmintic choice. Full guidelines are available at Austin Davis A4 8pp srw guidelines d8.0 0420.indd (website-editor.net) |
||||||||
| **Ensure the correct dose of anthelmintic is always used for the weight of the horse – weight as determined by a weighbridge is the most accurate. | ||||||||
| ***Good pasture hygiene means dung removed at least once week in grazing season. | ||||||||
| ****Praziquantel-only equine “specials” formulation available in the UK since August 2018. | ||||||||
Before undertaking FEC analysis, keep in mind the ERP for the anthelmintic used for the last treatment. A minimum wait of eight weeks is advised after benzimidazole, pyrantel embonate and ivermectin administration, and at least 12 weeks after moxidectin treatment.
Recommendations for FEC analysis are summarised in Panel 1. The widely used threshold eggs per gram (EPG) level for treatment is 200 EPG; this can be increased (for example, to 500 EPG) where transmission risk is lower (for example, in adult groups, grazed at low stocking density on paddocks where dung is removed at least once weekly).
- Collect samples as fresh as possible (those not fresh, but up to 12 hours old can be used, but should be refrigerated as soon as possible).
- Collect sub-samples from at least three faecal balls to ensure representative material is obtained and place into a zip-lock bag (or similar), removing as much air as possible to maximise anaerobic conditions to prevent egg hatching.
- If not processed immediately, samples should be refrigerated at the laboratory as soon as possible and analysis undertaken within five days of sample collection.
- Thoroughly mix samples before taking sub-samples for the FEC test.
- Use an FEC test method with as high a sensitivity as possible. If using the McMaster/modified McMaster method, counting all eggs in both chambers in a high-quality slide will enable a multiplication factor of ×15 (as opposed to ×50 or ×25) to calculate eggs per gram. This enables higher accuracy, which is useful in efficacy assessment.
- Regularly check the specific gravity of the flotation solution (1.2 for saturated NaCl solution).
- When counting, ensure microscope lenses are optimised for the distance required for parasitology slides. Use of the aperture condenser (contrast) helps delineate egg features.
- FECs are not accurate with frozen samples and should not be performed on diarrhoeic samples. However, the latter can be used for qualitative analysis or in larval cyathostominosis for detecting larvae.
Large strongyle and cyathostomin eggs cannot be distinguished in FECs; however, in managed herds, more than 99% of eggs counted will be cyathostomins. Identification of large strongyles requires culture and recovery of third stage larvae for morphological assessment. Tapeworm eggs are often missed or underestimated by standard faecal floatation methods, and modified techniques are required or antibody-based tests can be used.
FECs are invaluable in assessing effectiveness of anthelmintics in the field. This is achieved by performing a FECRT by collecting samples (as per Panel 1) prior to administering anthelmintic to provide a pre-treatment FEC. Samples are collected 10 to 14 days after treatment and the mean percentage reduction in FEC between pre-treatment counts to post-treatment counts is calculated for the group. At least six horses should be tested, ideally with a FEC of more than 200 EPG before treatment.
As the FEC can be variable, if lower numbers are assessed, the outcome is likely to be less accurate. The method used to count eggs should have a sensitivity of at least 25 EPG. Horses should not have received anthelmintic for the periods indicated already and been on-site for as long as possible. Thresholds used to make assumptions regarding susceptibility/resistance depend on the anthelmintic tested (Table 2).
| Table 2. Suggested cut-off values (mean percentage reduction in faecal egg count; FEC) for interpreting results of strongyle FEC reduction tests (FECRT; adapted from American Association of Equine Practitioners Guidelines, 2019). | ||||
|---|---|---|---|---|
| Anthelmintic | Observed results of FECRT (presented as mean percentage reduction between pre-treatment and post-treatment FEC tests) | |||
| Expected efficacy if no resistance | Susceptible (no evidence of resistance) | Suspected resistant | Resistant | |
| Fenbendazole | 99% | >95% | 90% to 95% | <90% |
| Pyrantel | 94% to 99% | >90% | 85% to 90% | <85% |
| Ivermectin/moxidectin | 99.9% | >98% | 95% to 98% | <95%* |
| *Resistance rarely reported by FECRT, so tests demonstrating below 95 per cent reduction after ivermectin/moxidectin should be repeated before confirming resistance. Note that emerging resistance to macrocyclic lactones in cyathostomins has been detected by reduced strongyle egg reappearance periods after treatment in different regions. | ||||
If the result is near the threshold, the test should be repeated before confirmation, and resistance should be evident in most/all horses tested. It is recommended that FECRT data can only be interpreted for the herd and not at individual level.
FECs are the cornerstone of diagnostics-led programmes, but these do not detect pre-patent nematodes, nor do the commonly used methods reliably detect tapeworm eggs. In Europe, antibody-based saliva, and serum tests to detect tapeworm infection, have been available for several years. In 2019, an antibody-based serum test was launched to support diagnosis of cyathostomin infections in horses.
Tapeworm antibody tests
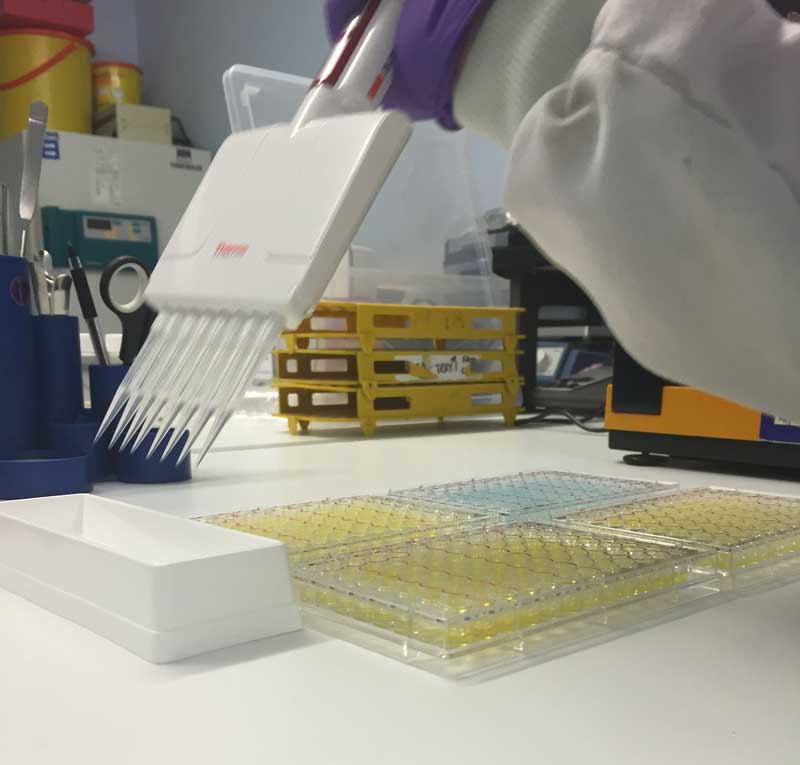
Measurement of parasite-specific IgG(T) by ELISA has become the most common way to identify equine tapeworm infections in the UK.
A serum test, based on antigens described in Proudman and Trees (1996), detects specific antibodies shown to have strong positive correlation (Spearman’s correlation, 0.78) to infection intensity. The commercial test format includes a calibration curve to accurately generate a “serum score” for each horse and act as quality control for each test.
Serum scores are categorised as “low”, “borderline” or “moderate/high”, based on validation studies using serum from naturally infected horses with enumerated A perfoliata burdens (Lightbody et al, 2016). A saliva test version is also available; this has been validated by comparing antigen-specific antibody levels in 104 saliva samples with tapeworm burdens postmortem.
This test also differentiates “low” from “borderline” and “moderate/high” burdens, and accurately identifies all horses with a clinically relevant “high” burden (more than 20 tapeworms; Lightbody et al, 2016). When used to provide diagnosis for a treatment decision, application of this test has resulted in reductions in treatment frequency of approximately 70% (based on the results obtained in commercial use from 2015 onwards).

Frequency of testing should be based on an assessment of infection risk. Horses grazing pastures where antibody tests demonstrate high burdens, or where tapeworm-related disease has occurred, should be tested in spring and autumn (Table 1), and followed by treatment if results indicate a moderate/high burden.
Horses considered at low risk (that is, low antibody in previous tests within the herd/no previous history of tapeworm-related disease on site) can be tested in spring or autumn. Anthelmintics licensed for treatment of tapeworm infection have a short half-life, reaching negligible levels in around 24 hours, after which, horses can rapidly become reinfected. Therefore, it is important to ensure that reinfection risk is reduced by good pasture management.
Cyathostomin antibody test
The cyathostomin antibody test detects IgG(T) levels to a combination of three cyathostomin recombinant antigens (CT3).
Analysis of antigen-specific IgG(T) in a cohort of experimentally and naturally infected horses (n=83) demonstrated that an ELISA based on these antigens provided excellent diagnostic accuracy for burdens up to 5,000 worms (Receiver operating characteristic area under the curve; ROC-AUC; values more than 9.0; Tzelos et al, 2020).
The CT3 ELISA has been optimised for commercial application, including incorporation of calibration curves and validated using sera from 124 horses for which gold-standard cyathostomin burden data was available; this “small redworm blood test” provides excellent diagnostic accuracy (ROC-AUC more than 0.9) for burdens up to 10,000 cyathostomin worms.
The commercial format includes a calibration curve which generates a “serum score” for each horse and acts as the ELISA plate quality control.
At the selected serum score threshold (serum score 14.37/1,000 total worm burden threshold), the test provides a ROC-AUC value of 0.96, with 96% sensitivity and 81% specificity (Lightbody et al, in press).
Horses suitable for testing are those that have returned low (below 200 EPG) FECs in recent tests and graze pasture where regular (at least once a week) dung removal occurs (Table 1).
Results are reported as serum scores along with statistically derived probabilities (derived using logistic regression models) that an individual is infected with a burden greater than a given threshold; the test is capable of accurately predicting thresholds of 1,000, 5,000 and 10,000 worms. The results are interpreted by veterinary surgeons to inform decisions on cyathostomin larvicidal treatments in autumn/winter (Table 1).
Depending on transmission risks within a herd, observations in naturally infected populations indicate that use of the small redworm test can lead to reductions in larvicidal anthelmintic treatments by 20% (in high worm transmission settings) and up to 78% (in low worm transmission settings).
The test can be used in acute larval cyathostominosis outbreaks to support diagnosis; for example, in one outbreak, all six clinically affected horses tested returned high serum scores (serum score more than 50.0; Walshe et al, 2021).

Diagnostic-led treatments must be supported by excellent pasture management
It is essential that control programmes include measures to reduce the force of infection on pasture. This includes removal of dung, at least once a week, to break the transmission cycle of pre-parasitic stages.
Dung should be completely removed from paddocks, including adjacent areas, and heaps should be in a separate location to grazing. Spreading of fresh manure should be avoided on fields destined for grazing or hay making, as should harrowing, unless fields are rested from horses for extended periods, timing depending on climatic conditions.
Treatment options
Treatment should be informed by knowledge of helminth epidemiology, information on the parasites present, the distribution of parasites within the herd and knowledge of how the herd is managed (Table 1). Anthelmintic classes licensed for use in horses in the UK include:
- benzimidazoles (compound: fenbendazole) for nematode infections
- tetrahydropyrimidines (compound: pyrantel embonate) for nematode and tapeworm infection (at twice the dose used for nematodes)
- macrocyclic lactones: (compounds: ivermectin and moxidectin) for nematode infections
- isoquinoline-pyrozines (compound – praziquantel) for tapeworm infections.
Fenbendazole resistance in cyathostomins has been reported for several decades and is commonly described. Cyathostomin resistance to pyrantel has been reported in many countries, including the UK.
Resistance in these nematodes to ivermectin and moxidectin measured by failed FECRT has been reported in Brazil, but many reports exist of reduced ERP where eggs are detected after treatment at intervals much shorter than when the compounds were first marketed.
Because of cyathostomin resistance levels to benzimidazole and pyrantel, it is recommended that if/when these anthelmintics are used, annual FECRT be performed (Table 1).
Macrocyclic resistance is more common in Parascaris species and first choice for treatments is non-macrocyclic lactone products. If using the latter to treat Parascaris species, efficacy should be assessed. Anthelmintic resistance has yet to be officially reported in A perfoliata, but anecdotal reports exist of praziquantel resistance and studies are ongoing to assess this.
References
- American Association of Equine Practitioners (2019). Internal Parasite Control Guidelines.
- Austin Davis Biologics. Small Redworm Blood Test.
- Lester HE and Matthews JB (2014). Faecal worm egg count analysis for targeting anthelmintic treatment in horses: points to consider, Equine Vet J 46(2): 139-145.
- Lightbody, KL, Davis PJ and Austin CJ (2016). Validation of a novel saliva-based ELISA test for diagnosing tapeworm burden in horses, Vet Clin Pathol 45(2): 335-346.
- Matthews JB (2014). Anthelmintic resistance in equine nematodes, Int J Parasitol Drugs Drug Resist 4(3): 310-315.
- Murphy D and Love S (1997). The pathogenic effects of experimental cyathostome infections in ponies, Vet Parasitol 70(1-3): 99-110.
- Nielsen MK (2021). What makes a good fecal egg count technique? Vet Parasitol 296: 109509.
- Nielsen MK (2022). Anthelmintic resistance in equine nematodes: current status and emerging trends, Int J Parasitol Drugs Drug Resist 20: 76-88.
- Proudman CJ and Trees AJ (1996). Correlation of antigen specific IgG and IgG(T) responses with Anoplocephala perfoliata infection intensity in the horse, Parasite Immunol 18(10): 499-506.
- Proudman CJ and Trees AJ (1999). Tapeworms as a cause of intestinal disease in horses, Parasitol Today 15(4): 156-159.
- Tzelos T et al (2020). Characterisation of serum IgG(T) responses to potential diagnostic antigens for equine cyathostominosis, Int J Parasitol 50(4): 289-298.
- Walshe N et al (2021). Outbreak of acute larval cyathostominosis – a “perfect storm” of inflammation and dysbiosis, Equine Vet J 53(4): 727-739.
