11 Jan 2022
Equine pedal osteitis
Edele Grey discusses this condition in horses, looking at presentation, clinical signs and treatment.
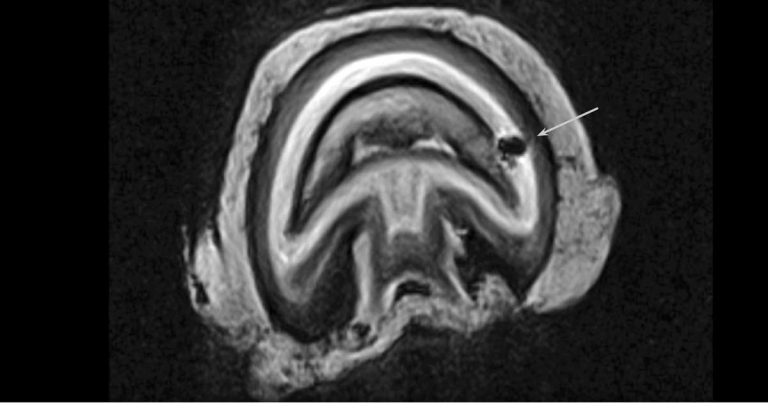
Image: University of Liverpool
Pedal osteitis is a poorly defined condition that some authors have argued is frequently misdiagnosed. The term covers a range of radiological abnormalities involving the third phalanx; however, knowledge is lacking as to the aetiology of some of these changes.
The term “pedal osteitis complex” has been postulated to describe a range of these radiological changes (Butler et al, 2000).
Osteitis implies an active inflammatory process within a bone; in this case, involving the distal phalanx (Dyson, 2011a). As the distal phalanx lacks a medullary cavity, inflammation or infection should really be termed osteitis and not osteomyelitis.
Broadly, two types of pedal osteitis exist: septic, from bacterial infection; and non-septic, due to trauma or repetitive concussive forces; although the latter has not been conclusively proven (Dyson, 2011a).
Arguably, the most common of these conditions is septic, due to either a puncture wound or as a complication of persistent subsolar abscesses (O’Brien and Hunt, 2014). Non-septic osteitis may be due to chronic bruising of the sole and is more often seen in athletic horses working on hard ground. It can be a sequelae to chronic pain from persistent corns, laminitis or a shoe creating an abnormal pressure point on the sole of the hoof.
Anatomy
The distal phalanx is a unique bone as it has no medullary cavity with exceptional vascularisation – it is suspended within the hoof capsule by epidermal laminae, which is integrated within the laminar corium.
The palmar processes project caudally on both medial and lateral aspects of each phalanx, with the solar and abaxial surfaces being relatively smooth. Cartilage attaches to the proximal border of each process; initially hyaline in the juvenile, which then progresses to fibrocartilage in adults (Dyson, 2011a).
The size and shape of these cartilages is extremely variable within and between horses. The suspensory apparatus of the distal phalanx, coupled with the digital cushion, serves to dissipate energy with foot strike, forcing evacuation of blood from the vessels within the foot (Pollitt, 2010).
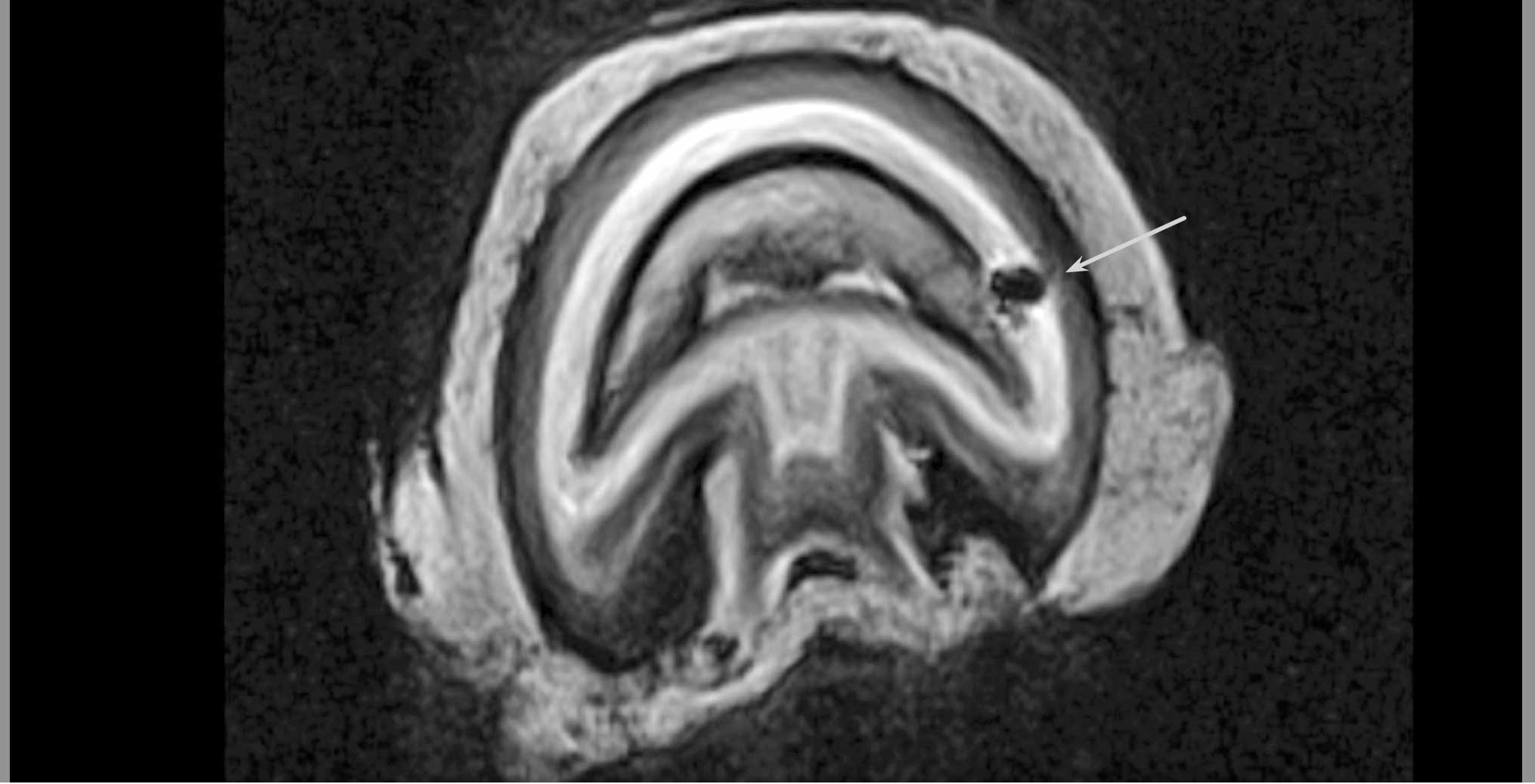
Figures 1a and 1b show the anatomy of the pedal bone and its suspension within the hoof.


Radiographically, the distal phalanx has a wide spectrum of relatively common variations that may be associated with clinical signs.
Horizontal orientation of the pedal bone’s solar surface in relation to the ground, or horses with palmar processes lower than the toe, has been linked with more proximal sites of pain (Dyson, 2011a).
A wide range of degrees of ossification of the lateral cartilages exists between horses, with heavier breeds having increased ossification when compared with lighter breeds and ponies.
Radiographs have poor sensitivity for active inflammation as it can take two weeks to reveal changes and these persist for extended periods after the inflammation has subsided (Mizobe et al, 2017; Dyson, 2011a).
Slight bony irregularity associated with the parietal sulci may be clinically insignificant new bone formation or may be mineralisation of the dermal laminae, which can cause clinical signs of lameness, although the aetiology is ill‑defined (Butler et al, 2000).
Presentation and clinical signs
Onset and duration of clinical signs vary depending on the inciting cause. However, classically a horse will present with a chronic lameness of insidious onset, which may be bilateral in non-septic cases (Dyson, 2011a); or in septic cases, a lameness that resolves with a course of antimicrobials only to recur when they are withdrawn (Lugo and Gaughan, 2006).
In chronic laminitis, recurrent abscessation at the same site may indicate a septic process within the distal phalanx.
Horses of any age, sex or breed can be affected by pedal osteitis; however, it has been postulated that certain foot conformations may predispose to some clinical manifestations of non-septic pedal osteitis (Ross and Dyson, 2011). Long toes, low or collapsed heels and horses with flat soles may be predisposed, and osteitis is almost exclusively seen in these horses’ forelimbs.
Diagnosis
Traditionally, a diagnosis was made on clinical response to hoof testers, with perineural analgesia and radiographic evidence of bony changes to the distal phalanx.
During a clinical lameness examination, the affected hoof may have increased temperature on palpation in comparison with the other feet and bounding digital pulses may be palpable, particularly on the side of the lesion. This, however, is not pathognomonic for pedal osteitis.
Reaction to hoof testers is common, but rarely localised to a focal area, unlike a subsolar abscess.
The lameness usually improves with a palmar/plantar digital nerve block, but not with navicular bursal nor distal interphalangeal joint analgesia (Ross and Dyson, 2011).
Radiographic views should include at a minimum a lateromedial (LM), a dorsopalmar/plantar and a dorsoproximal palmar/plantarodistal oblique (DPrPDiO) view with other oblique views permitting further examination of the palmar processes (Dyson, 2011a).
It is important to remember a broad spectrum of radiographic divergence exists within clinically sound horses and that previous changes persist after the acute inflammation has subsided, possibly for life (Dyson, 2011a; Butler et al, 2000).
In chronic laminitis and horses with dropped soles, abnormal mineralisation may be present along the dorsal aspect of the pedal bone between the coronary band and solar margin distally near the toe, indicating a more chronic inflammatory process (Butler et al, 2000).
Radiographic changes may be absent in early stages of pedal osteitis, as up to 40% of the mineral content of the bone must be lost before osteolysis is radiographically visible (Cauvin and Munroe, 1998).
The evidence of osteolysis includes development of radiolucent areas and loss of trabecular detail with apparent widening of the vascular channels, indicating bone resorption along the solar margin of the distal phalanx (Dyson, 2011a; Mizobe et al, 2017).
In cases where radiographic changes are apparent, the contralateral limb should be screened as non-clinical changes are usually bilaterally symmetrical.
The palmar processes also show signs of osteitis, best seen on LM, DPrPDiO and palmar/plantaroproximal palmar/plantarodistal oblique views.
Discrete areas of radiolucency are most often seen along the axial surface of the palmar processes, with solar irregularity, elongation of these processes and abnormally thin soles in clinically affected horses (Butler et al, 2000).
Septic osteitis usually involves the parietal or solar borders of the third phalanx causing focal demineralisation, visible as a solar defect on a DPrPDiO view (Figure 2). This radiolucency is irregularly shaped without a sclerotic margin, although if a sequestrum is present a radiopaque area with a radiolucent border will be visible.

As the inflammation progresses, exaggeration of the vascularity may be present in the region of the infectious focus (Butler et al, 2000).
If an abscess has caused a pocket of inspissated purulent material within the pedal bone, an osseous cyst-like lesion may be apparent on the radiographs (well‑defined radiolucent area); however, if no connection to the distal interphalangeal joint exists, these can be ruled out (Butler et al, 2000).
Additional imaging modalities may be required to definitively diagnose active pedal osteitis. Nuclear scintigraphy, MRI and CT are becoming more readily available, and are being carried out more frequently.
Low-field MRI and gamma scintigraphy can both be performed under standing sedation, which can identify lesions not visible on radiographs.
The pedal bones generally have a relatively increased radiopharmaceutical uptake compared with other bones on a scintigraphy examination, but in cases of pedal osteitis this will be further increased and the bone will appear “hotter” than the other feet (Dyson, 2011a).
On MRI, septic pedal osteitis will appear as a focal area of hyperintensity on T2-weighted images, extending into the distal phalanx, while on T1-weighted images the area can appear hypointense within subchondral bone (Figure 3), which is consistent with bone sclerosis (Mizobe et al, 2017).
If the cause of the osteitis is a penetrating trauma, a signal void may appear to outline a tract to the distal phalanx. Increased signal intensity will also be visible in fat‑suppressed images, which may be coupled with irregularity of the cortical bone and disruption of adjacent laminae, which is evidence of an active osteitis (Dyson, 2011a).
In contrast to other advanced imaging modalities, CT requires a general anaesthetic, which increases the cost and risk of the procedure, and it has reduced ability to differentiate between fluid and soft tissue structures; therefore, it is not commonly performed for visualising the structures of the foot (Claerhoudt et al, 2014).
Treatment options and prognosis
Surgical debridement is the only recommended treatment for cases of septic pedal osteitis, with 73% of cases returning to – or reaching – expected levels of performance (O’Brien and Hunt, 2014).
Up to 25% of the distal phalanx can be surgically removed with the horse still having the potential to return to soundness (Rich Redding and O’Grady, 2012). The procedure can be carried out either standing or under general anaesthesia depending on a number of factors, including the patient’s temperament and the extent or location of the lesion.
Debridement with sedation and regional perineural analgesia, coupled with appropriate haemostasis, can usually expose sufficient tissue for the procedure. This will decrease the risks and costs associated with a general anaesthetic.
Two approaches exist: solar, through any defect that exists with the limb held in flexion; or through the hoof wall via a surgically created window with the limb bearing weight.
Necrotic tissue must be removed in full, curetted to healthy bone that is hard and lighter coloured.
Devitalised bone has poor antibiotic penetration, so chronic drainage postoperatively indicates the persistence of a necrotic focus (O’Brien and Hunt, 2014).
Once sharp debridement of the defect has been carried out, maggot therapy may be used to ensure all necrotic material is removed (LePage et al, 2012; Rich Redding and O’Grady, 2012). Sterile packing with a bandage or hospital plate postoperatively – until a healthy bed of granulation tissue with cornification is evident for approximately six to eight weeks – is advised.
Patients are usually sound at a walk within two to four weeks postoperatively, with increasing comfort on tapering doses of NSAID medications (O’Brien and Hunt, 2014).
Prognosis for non-septic osteitis depends on early recognition of the disease and medical therapy to restore normal foot conformation using rest, corrective farriery, NSAIDs and removal of the inciting cause in cases of traumatic origin.
Chronic cases of pedal osteitis may have hoof capsule deformities that will carry a guarded prognosis (Dyson, 2011b).
Work on hard ground should be avoided while therapeutic trimming is carried out. Barefoot trimming and turnout may be beneficial if hoof quality is good.
Conclusion
Equidae are ungulate mammals – each limb stands on a single digit encased within a tough, keratinised hoof and lightweight limbs.
This evolutionary adaptation has contributed to the speed and athletic prowess of domestic horses; however, damage to these hooves can severely impair a horse’s mobility.
Pedal osteitis is a relatively common occurrence in horses, with a septic cause likely to be the diagnosis most frequently recognised in practice.
Septic pedal osteitis should be considered a differential in cases of chronic foot abscessation or recurrent lameness that resolves with antimicrobial therapy.
Non-septic osteitis should be considered in cases of chronic or intermittent lameness in horses working on hard ground that have a generalised response to hoof testers and improvement to diagnostic foot analgesia.
In patients with a history of a penetrating wound without synovial involvement or a subsolar abscess, a blunt radiopaque probe or contrast radiography may reveal a tract in contact with the distal phalanx.
If radiographs have no abnormalities, consider referral for advanced imaging to determine whether a soft tissue injury or pedal osteitis may be the cause of the lameness.
References
- Butler JA, Colles CM, Dyson SJ, Kold SE and Poulos PW (2000). Foot, pastern and fetlock, Clinical Radiology of the Horse (2nd edn), Blackwell Science, Hoboken: 27-130.
- Cauvin ERJ and Munroe GA (1998). Septic osteitis of the distal phalanx: findings and surgical treatment in 18 cases, Equine Vet J 30(6): 512-519.
- Claerhoudt S, Bergman EHJ and Saunders JH (2014). Computed tomographic anatomy of the equine foot, Anat Histol Embryol 43(5): 395-402.
- Dyson S (2011a) Nonseptic osteitis of the distal phalanx and its palmar processes, Equine Vet Educ 23(9): 472-485.
- LePage OM, Doumbia A, Perron-LePage MF and Gangl M (2012), The use of maggot debridement therapy in 41 equids, Equine Vet J 44(Suppl 43): 120-125.
- Lugo J and Gaughan EM (2006). Septic arthritis, tenosynovitis, and infection of hoof structures, Vet Clin North Am Equine Pract 22(2): 363-388.
- Mizobe F, Namura M, Kato T, Katayama Y, Kuwano A, Ueno T, Yamada K and Spriet M (2017). Signal changes in standing magnetic resonance imaging of septic pedal osteitis in a Thoroughbred racehorse, Jpn J Vet Res 65(2): 101-106.
- O’Brien T and Hunt RJ (2014). Recent advances in standing equine orthopaedic surgery, Vet Clin North Am Equine Pract 30(1): 221-237.
- Pollitt CC (2010) the anatomy and physiology of the suspensory apparatus of the distal phalanx, Vet Clin North Am Equine Pract 26(1): 29-49.
- Redding WR and O’Grady SE (2012). Septic diseases associated with the hoof complex: abscesses, puncture wounds, and infection of the lateral cartilages, Vet Clin North Am Equine Pract 28(2): 423-440.
- Ross MW and Dyson SJ (2011). The distal phalanx and distal interphalangeal joint. In Ross MW and Dyson SJ (eds), Diagnosis and Management of Lameness in the Horse (2nd edn), Elsevier Saunders, Philadelphia: 349-366.
