24 Jun 2025
Mélanie Perrier MRCVS looks at some of the developments in wound treatments for horses.

Image: chelle129 / Adobe Stock
Wounds are a common occurrence in horses and can be classified based on their extent, location, stage of healing and degree of contamination.
They can present as a therapeutic challenge for the equine practitioner – especially when presented as second intention healing with its associated complications, particularly hypergranulation tissue formation.
Anatomical knowledge is important, as one of the first questions the equine practitioner will have to answer is whether the wound communicates with a synovial structure (joint, bursa, tendon sheath) or cavity (abdominal, thoracic and sinus), which will influence the treatment options chosen.
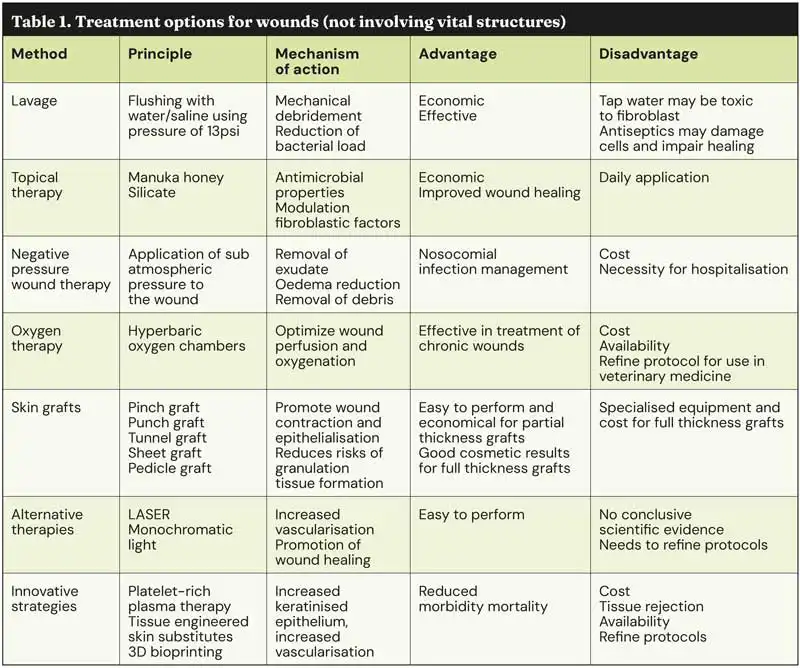
This article will give an overview of what is available in terms of treatment for wounds that do not involve any vital structure, trying to focus on the scientific evidence of the past five years or so (Table 1).
One of the most important steps when considering wound treatment is wound lavage and debridement. When assessing a wound, the area should be clipped and cleaned as best as possible prior to assessing its extent and configuration. When considering which solution is most effective for flushing wounds, no relevant studies on the effectiveness of antiseptic solutions for cleaning equine wounds are available, and no reported difference exists in infection and healing rates after flushing wounds with either tap water or normal saline solution1,2, besides one study stating tap water is toxic to fibroblasts3.
The solution should be delivered to the wound with an appropriate pressure of around 13 per square inch (psi). This can be achieved by using an automated lavage solution kit or a 12ml syringe attached to a 22G needle. Antiseptic use for wounds has also been discussed extensively over the years. Overall, antiseptics are better recommended to be used diluted around the wound and not directly over it, as they may have negative effects on the cells needed for adequate wound healing. When using antiseptics, they should always be diluted appropriately, and some evidence suggests that povidone iodine may be effective in lavaging contaminated wounds1.
Topical treatments are often used to influence the healing process. Common topical treatment used for wound management include corticosteroid application for the management of exuberant granulation tissue and honey for its antibacterial effect and improvement of autolytic debridement.
A wide variety of topical wound care medication is available to the equine practitioner and general public, with inconclusive results and varying degrees of reported success4. One publication investigated the use of peptide-modified collagen chitosan hydrogel for wound healing. The hydrogel has been proposed to promote keratinocyte attachment, survival and migration, but also to promote rapid re-epithelialisation with improved physiological features. This experimental study looking at delayed wound healing suggested a single topical application of the product was safe and helped incidence of wound closure and modulation of the biomechanical function of healing tissues5.
Another publication investigated the use of a maltodextrin and ascorbic acid gel in the treatment of distal limbs wounds. Some studies have demonstrated maltodextrin and ascorbic gel may improve chronic wound healing by increasing the protein expression of TGFB1, increased collagen turnover, and may have the potential to deliver nutrients to the wound by delivering glucose for cell metabolism.
It also has antibacterial and bacteriostatic properties. Again, this study looked at chronic non-granulating wounds and concluded that topical application of the product resulted in increased wound contraction and quicker epithelialisation6.
Manuka honey, which has been used for centuries, is again becoming more and more popular with clients and equine practitioners. Honey is used for its antimicrobial properties and its ability to draw debris and necrotic tissues, and reduce oedema due to its hyperosmolar nature7,8,9 (Figure 1).

One publication looking at the use of manuka honey on second intention healing of distal limb wounds found faster healing times with honey-treated wounds compared to other wounds. Honey seems to be most useful during the inflammatory stage of healing and for its debridement properties, so is best recommended to be used during the first two to three weeks of wound healing10. Another publication looked at intralesional application of honey on surgically treated lacerations and found that its use prior to closure may help prevent infection and dehiscence11.
Finally, several silicate-based topical products are coming to the market for use in wound healing. Silicate is reported to act through the release of orthosilicic acid, which modulates the micro-environment and reduces chronic inflammation in the wound bed. It also allows improved healing by modulating fibroblastic factors and reducing inflammatory factors such as TGF-β1, IL-1β. In one study, its use in the treatment of equine distal limb wound healing may have reduced the development of exuberant granulation tissue and the need for surgical debridement12.
Negative pressure would therapy (NPWT) or vacuum-assisted closure (VAC) has been used extensively in humans to improve wound healing. This treatment modality refers to the application of sub-atmospheric pressure of about 125mmHg to the wound. This is achieved by using an evacuation tube seated in a foam dressing and secured to the area using a barrier drape, and several layers of waterproof cellophane to provide an airtight seal at the skin margins of the wound. The end of the tube is then connected to a drainage tube and pump providing a continuous or interrupted negative pressure of 125mmHg. The main indication for this therapy is the reduction in dead space and removal of exudates. This will result in oedema reduction, removal of debris and increased dermal perfusion. It will also release growth factors and reduce the number of bacteria within the wound.
In a scoping review for the use of this modality, the main indications and benefits for the therapy far outweigh the disadvantages, which were the cost of the equipment and the requirement for hospitalisation, which has to be weighed against the cost of regular bandages and wound care. The main advantages reported in this review were the monitoring and contention of septic exudate produced, control and removal of bacterial biofilm, improved healing by increasing blood flow, modulation of inflammatory response, facilitation of wound contraction and decreased healing time13.
In a case series of limb wounds in 42 horses, which can be particularly challenging in horses, this system was deemed to provide satisfactory healing in about 70% of cases. In that study, application of the system ranged from 2 to 36 days and was well tolerated except in one horse.
Careful preparation of the site is important to provide a good enough seal at the wound margin and allow optimal function of the device. Some of the reported complications include pressure necrosis, blockage of the tube by exudates and dislodging of the system. Other disadvantages include the costs associated with the device and necessary hospitalisation and care. Further studies may be needed to refine the advantages and optimal use of the system, but some promise regarding the limitation of nosocomial infection, as published in the human literature, may be of interest14.
Finally, one publication comparing the efficacy of NPWT to calcium alginate dressing in a contaminated equine distal wound model did not find any differences in wound healing between the two treatments. This was, however, a limb model where wounds were created over the dorsomedial metacarpus of a small amount of horses (10)15.
While some promise exists in the use of this therapy – especially in traumatic wounds and surgical sites infection – its cost, limited availability and still confounding scientific evidence in the equine literature limits its use in practice where active suction drains are still most commonly used (Figures 2 to 4). More scientific evidence may be needed to evaluate its main indications and benefits.

Oxygen therapy has been used to optimise wound perfusion and oxygenation and, therefore, prevent wound infection. The level of oxygen needed for wound healing varies on the stage of healing, as some hypoxia is needed initially to promote angiogenesis. One of the most common ways of delivering oxygen is through hyperbaric oxygen chambers, which allow exposure to 100% oxygen in a pressurised environment. Unfortunately, this modality while effective is not widely available in Europe16.
Topical oxygen therapy via an electrochemical oxygen concentration device has been studied experimentally, but no difference was seen in wound healing of the distal limbs in horses. Ozone therapy has also been described by delivering ozone, either through a sealed ozone-resistant bag, which is insufflated, or applying ozonated oil over the wound, but this has not been evaluated in equine patients. While oxygen therapy is likely to have benefits – especially for the treatment of chronic wounds – ideal application methods and protocol still need to be determined for use in equine veterinary medicine17,18.
Skin grafts are commonly used in large defects that would not heal functionally or to improve cosmetic outcomes. This technique of wound treatment relies on an appropriate preparation of the wound bed for graft reception and subsequent adequate immobilisation of the grafted area. To ensure optimum results, the recipient bed should be covered in healthy granulation tissue and free of infection. Skin grafts promote wound contraction and epithelialisation, while also reducing the risks of exuberant granulation tissue formation.
Different types of graft can be divided into full (dermis and epidermis) and partial (epidermis and part of the dermis) thickness skin graft. Full thickness skin graft generally results in better cosmetic results, but are associated with a higher risk of failure, longer healing time and limited donor site availability. Partial thickness skin grafts are, therefore, usually preferred if feasible, as they carry a higher success rate and are easier to harvest. They, however, result in slightly less desirable cosmetic outcomes. In equine practice, most grafts are autografts, even if allografts and xenografts have been described in the literature. Common donor site for grafts include regions that will not result in cosmetic blemishes, such as the ventral abdomen, pectoral region or under the mane.
Different techniques are available, with pinch grafting and punch grafting being commonly used, as they are relatively easy to perform and can be done on the standing sedated patient. Tunnel grafting, sheet grafting and pedicle grafting necessitate general anaesthesia and specialised equipment, hence why they are mainly performed in referral centres. They are also more costly, but usually result in improved cosmetic results and more rapid healing.
Pinch and punch grafting have had reported results of up to 75% and 95%, respectively, and remain a good treatment option for large wounds or wounds where cosmetics is a concern19.
A variety of alternative therapies have been proposed to enhance wound healing, such as extra corporal shockwave, therapeutic ultrasound and LASER therapy20. While promotion of wound healing was among the first observed benefits of photobiomodulation and while some well-understood mechanism of action exists, alongside growing evidence in human studies, no scientific evidence corroborates the benefits of photobiomodulation in wound healing in the horse21.
Similarly, one article looked at the use of infrared and monochromatic light on wounds, and the results of the study did not identify any clinically relevant positive effect of this modality on wound healing22.
Unfortunately, most of the publications regarding alternative therapies – especially light therapy – use a variety of settings with wide ranges of doses and wavelengths and different treatment protocol. While this may be an attractive treatment option – especially for owners – the need exists to develop optimal clinical protocol based on evidence-based medicine.
In the human literature, advancements in emerging technologies – especially in the area of 3D bioprinting, platelet-rich plasma therapy (PRP) and extra cellular-based (ECM) therapies have been reported. Biologic therapies’ use in wound healing has been studied in equine medicine.
Several publications regarding the use of stem cells, PRP and other biologicals can be found. In vivo studies have looked into the use of biological dressings and in particular the use of amnion or amnion-derived products, split thickness allogenic skin, allogenic peritoneum and xenogeneic porcine small intestinal mucosa. No advantages for the use of these dressing in small granulating wounds have yet been found23.
Most studies looking at the use of PRP in equine wounds are in vitro studies evaluating its use for surgical incisions/surgically induced wounds and distal limb wounds. No consensus exists on the usefulness of the treatment for wound.
One study concluded that PRP gel may be an alternative for acute wounds since PRP-treated wounds had better keratinised stratified epithelium than control wounds, higher blood vessels and better organised interconnecting collagen fibres.
Another study concluded that PRP gel may induce fibrosis, but had the ability to provide antibacterial support.
Finally, a study on distal limb wounds concluded that PRP treatment may be beneficial for wounds where massive tissue loss was present, or for chronic wounds. Again, more scientific evidence will be needed to prove the benefits and optimal use of biological in wound treatment24.
Tissue-engineered skin substitutes and 3D bioprinting consisting in the fabrication of biocompatible artificial skin, consisting of a deposition of living cells, biomaterials, biomolecules and growths factors layer by layer, have been described. The resulting fabricated skin closely resembles normal skin and should be able to transport nutrients and wounds exudates, while also depositing various skin cells at particular layers.
Skin substitutes have the advantages of providing mortality and morbidity reduction in chronic wounds, being safe and effective.
The main limitations include the risks of tissue rejection and a high cost, which may result in these products not being available on the veterinary market for a period of time, if at all.
While increasing scientific evidence exists about newer treatment options for wound management on the human and veterinary medicine side, the principles of wound management remain overall the same as they have been in the past few years. Early and appropriate treatment remain the key to a successful outcome.
Further scientific evidence will be needed to refine the use of other modalities/treatment options.