8 Apr 2019
Managing asthma in equids
Sarah Gough and David Rendle discuss the diagnosis and treatment of mild and marked forms of the disease, including environmental management.

Figure 1. Nostril flare in a horse with an acute exacerbation of equine asthma, despite excellent management, including the paper bedding seen in the background.
Equine asthma is a common cause of poor performance and respiratory distress in horses throughout the world. It encompasses a spectrum of disease ranging from a milder form – previously termed equine inflammatory airway disease (IAD) – to the more marked equine asthma, formerly recurrent airway obstruction (RAO), in which exercise intolerance may be more marked and respiratory distress may occur at rest.
Pasture-associated RAO is a further subset of equine asthma triggered by access to pasture and, presumably, pollens, rather than a stable environment; clinical signs tend to be severe. Regardless of the specific manifestation of equine asthma, tracheal and/or pulmonary inflammatory changes develop and leukocyte profiles change within tracheal wash fluid (TWF) and/or bronchoalveolar lavage fluid (BALF).
Managing the environment is the most critical component of management, with additional therapeutics required in many cases to control the inflammatory changes, bronchoconstriction, mucous production and clinical signs.
A spectrum of diseases
Equine asthma is a syndrome that encompasses a spectrum of disease of varying severity and, thus, varying treatment requirements. Mild asthma primarily affects younger horses (two to four years old) although it can occur in horses of any age1, 2. Affected horses may exhibit mild exercise intolerance and cough during exercise; however, respiratory rate and effort are normal at rest and a cough is variably present1-3.
Marked equine asthma typically affects older horses (more than seven years old), and while environmental management and therapeutic interventions can control the clinical signs, the disease is allergic and cannot be cured4-6.
Marked equine asthma reflects a more severe form of disease with chronic cough, exercise intolerance and increased respiratory effort (with the potential for respiratory distress) at rest4, 7, 8.
Cytologically, a spectrum exists of neutrophilic inflammation in the TWF and/or BALF of horses with equine asthma, with increases in eosinophils and mast cells also being identified in some cases1-4. Increased tracheal mucous is a consistent finding regardless of the severity of asthma2, 4, 7, 6. In most mild cases the inflammatory changes are reversible and the potential for complete recovery exists if horses are managed appropriately4, 6. As asthma becomes more marked, irreversible airway remodelling and fibrosis may occur. Evidence exists of an underlying genetic basis for marked equine asthma3, 7, which should be considered in animals that might be used for breeding.
Recognising clinical signs
Clinical signs will vary depending on the severity of asthma. Mild disease can be subclinical and result in reduced performance, with diagnosis being based on cytological examination of BALF and/or evidence of tracheal mucous endoscopically.
Chronic cough (which may be more prominent, either during exercise or at rest) and bilateral nasal discharge are common features of equine asthma. Although some cases of mild equine asthma show increased respiratory effort during exercise and prolonged exercise recovery periods, horses with mild asthma do not have increased respiratory rate, effort or distress at rest2, 3, 7, 9.
While mild equine asthma is seen in all breeds and ages, it is most often associated with young sporthorses and racehorses, with racehorses often reported to “fade in the last quarter” during racing2, 7.
Horses with marked equine asthma will exhibit signs at rest (Figure 1) during exacerbations of disease and may show more consistent exercise intolerance3, 7. Typical clinical signs during exacerbations of disease include flared nostrils and evidence of contribution from the abdominal musculature to respiratory effort, resulting in biphasic expiration and, in chronic cases, a heave line7. The increased respiratory effort is typically more pronounced on expiration due to bronchiolar collapse with airway remodelling, although in more severe cases, increased inspiratory effort may also be noted7.

Diagnostic tests
Cytological assessment of BALF is considered the most sensitive and specific diagnostic test for equine asthma1-3, 10. Examination of TWF may also reveal increased mucous production and an altered leukocyte profile; however, the results of tracheal wash analysis are less reliable in identifying lower airway pathology. Cytological examination of BALF is, therefore, preferred and is recommended when any form of equine asthma is suspected (Figure 2)4.

Regrettably, a general reluctance exists among UK vets to perform bronchoalveolar lavage for diagnosis of lower airway disease, which is a shame as it is a straightforward and very useful diagnostic test (Panel 1).
A bronchoalveolar lavage (BAL) can be performed via an endoscope or by using a cuffed nasobronchial tube. In the UK the use of a nasobronchial tube is preferred and is the method described here.
- Sedate the horse appropriately. Butorphanol has an antitussive effect and its use is recommended. The application of a twitch may also be helpful.
- Warn the owner the horse will cough while a BAL is being performed and not all fluid will be retrieved. The volume of fluid instilled is negligible compared to the volume of the horse’s lungs and any remaining fluid is absorbed rapidly into the circulation. Warn a second attempt may be required if insufficient fluid is retrieved from the first attempt.
- Prepare a solution of 15ml local anaesthetic (LA) with 15ml saline in a 30ml syringe and the solution to be instilled to collect the sample. The volume to be instilled varies between 200ml and 500ml 0.9% saline or phosphate buffered saline depending on personal preference. The authors routinely use 300ml (5 × 60ml syringes).
- Check the BAL cuff tube is not leaking.
- Pass the BAL tube via the ventral nasal meatus and, with the head and neck extended to ease passage into the trachea, pass it into the trachea.
- Once in the proximal trachea, approximately 10ml of LA and saline is instilled before the tube is further advanced to the approximate level of the thoracic inlet, at which point the remaining LA and saline is instilled and followed with air to clear the tube. At this stage coughing is expected. If endoscopy is performed prior to BAL, LA can be instilled via the endoscope instead.
- The BAL tube is then further advanced until it will not pass any more as it becomes wedged in a bronchus – at which point the cuff is inflated with around 5ml of air.
- Instil the saline. Withdraw as much fluid as possible (with minimal withdrawal force to reduce airway collapse). More than 50% return of infused fluid is expected. If the distal airways have been lavaged effectively the sample will be foamy due to the presence of surfactant (Figure 3).
- Pool the sample and submit an aliquot for cytological evaluation.
- If the sample is being posted to a laboratory it should be fixed at the time of collection with cytospin, ethylenediamine tetra-acetic acid or formalin. Contact your laboratory to find out which fixative it prefers1.

Managing equine asthma
Some cases of equine asthma are reversible – other horses with true allergic disease will remain predisposed for life. Progressive airway remodelling can occur in cases of severe equine asthma, resulting in permanent reductions in lung compliance and irreversible fibrosis4. Timely and effective treatment is, therefore, important not only to reduce morbidity short term, but also to improve prognosis long term.
Environmental management
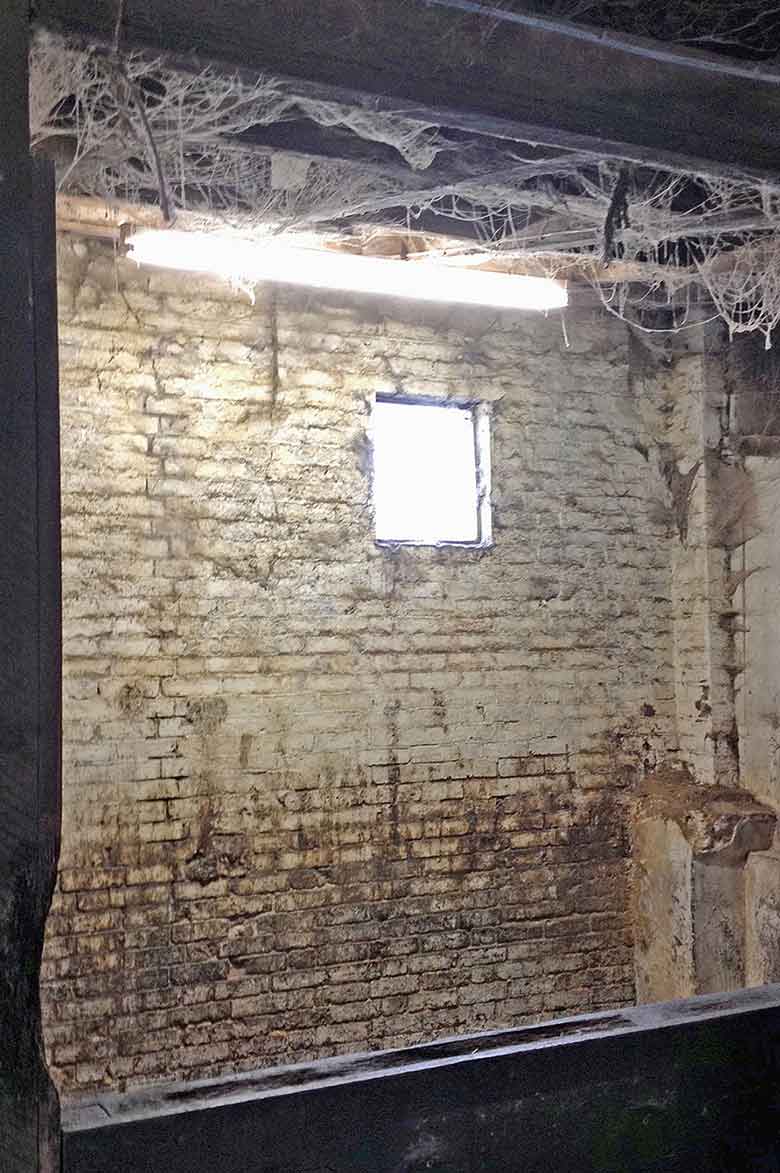
The stable environment contains numerous substances noxious to the lower airways, including bacterial endotoxin, inorganic dust, moulds, plant debris, mite debris, volatile gases and ammonia2, 11, 12 (Figure 4).
While many organic materials can exacerbate equine asthma, straw and hay are considered the worst offenders2. Minimising the time spent in a stable environment is the most important component of managing equine asthma2, 3, 5, 13. In summer pasture-associated disease, pollens are thought to be responsible for inciting lower airway inflammation.
In horses where 24/7 outdoor management/turnout is not feasible, steps to minimise exposure to respirable dust in the stable are required; for example, provision of pelleted feed rather than chaff or hay and use of dust-extracted wood chip bedding2 (Figure 5).

If hay or chaff is to be provided it should be dampened down or steamed and fed from the ground to remove or reduce respirable particles (Figure 6); even transient exposure to hay may induce or exacerbate equine asthma.

Affected horses (if not all horses) should be removed from the building during stable cleaning, removal or provision of hay or any other activities that may increase exposure to dust and particulate matter2. These environmental factors are more important in managing equine asthma than provision of therapeutics, and without effective environmental management, therapeutic management is unlikely to be successful3, 5, 6, 13.
Therapeutics
Therapeutic management of equine asthma involves the provision of glucocorticoids to reduce the airway inflammation, with or without addition of bronchodilators, alongside environmental management to reduce the ongoing inflammatory stimulus. While corticosteroids, in conjunction with environmental management, remain the mainstay of treatment for equine asthma2, during acute exacerbation, immediate relief of bronchospasm and airway hyper-responsiveness requires additional treatment with rescue medications.
Rescue therapy for severe equine asthma
During acute exacerbation of severe equine asthma, bronchodilation is the initial aim. Parasympatholytic drugs, such as N-butylscopolamine or atropine, are indicated with effects typically seen within approximately five minutes of administration2, 5 if bronchospasm occurs. Unfortunately, the clinical effects are short-lived, with bronchospasm being relieved for 30 minutes with N-butylscopolamine in one study and 1 hour with atropine14.
Clenbuterol IV is less effective than atropine or N-butylscopolamine and comes with a risk of exacerbating ventilation/perfusion mismatch, and, thus, clinical signs. Given the short-lived empiric effects of these bronchodilators, it is important other therapy is instigated at the outset, as outlined for the acute case.
Treatment of the acute case
In cases of moderate to severe equine asthma, an initial course of systemic glucocorticoids is required to control the lower airway inflammation and subsequent bronchoconstriction. Both oral prednisolone and oral or parenteral dexamethasone are used for short-term control, with dexamethasone proven to reduce airway inflammation15.
Prednisolone is licensed for the treatment of RAO in the UK; however, most clinicians consider dexamethasone to be more effective in reducing lower airway inflammation and improving clinical signs.
Studies comparing prednisolone and dexamethasone are limited. In one study, responses were comparable when good environmental management took place. In another, dexamethasone appeared superior, even with prednisolone used at 2mg/kg – twice the licensed dose. Dexamethasone was used at a conservative 0.05mg/kg16, 17. Anecdotally, it is reported some horses that do not improve with prednisolone will show clinical improvement with dexamethasone. Further investigations are required.
Dexamethasone is typically used by IV injection in an emergency situation and then daily or every other day by IV or IM injection until signs improve. If owners do not want to perform injections, or more chronic treatment is required, the injectable formulation can be administered orally, or an extemporaneous paste designed for use in horses can be used. The use of oral dexamethasone is off-licence and should be administered with informed consent and consideration of the cascade. When using dexamethasone orally the dose should be increased 20% (if administered by mouth) to 50% (if added to feed) relative to the injectable dose as not all of it will be absorbed.
Bronchodilators may be of benefit in acute disease in some cases; however, it is important to remember bronchodilators only provide empiric therapy and so do not address the underlying inflammatory response. They should not be used for long-term management of equine asthma; if clinical signs are persistent, insufficient control of the underlying inflammatory response occurs and more glucocorticoids are required.
The parasympatholytic drugs N-butylscopolamine or atropine cannot be used for more than a few doses for fear of ileus. Inhaled treatment is not appropriate in acute cases with reduced respiratory function, therefore oral clenbuterol is the bronchodilator of choice in acute cases of disease. Clenbuterol is only effective for short-term treatment as receptors downregulate. If treatment of the underlying inflammatory response is effective, treatment with bronchodilators beyond a couple of weeks should not be needed.
In cases of mild equine asthma, (those that would formerly be considered IAD rather than RAO), adequate control of airway inflammation can normally be achieved with the use of inhaled glucocorticoids (as discussed later), without the need for systemic treatment.
Long-term treatment and delivery options
The most critical component of long-term control of equine asthma is environmental management to reduce the exposure to respirable aeroallergens and dust particles. However, in many cases of chronic equine asthma, environmental management alone is not sufficient and long-term or intermittent glucocorticoid use is often required18. It is important horses are re-examined regularly, particularly after exacerbation of disease, to ensure they are being managed effectively and to enable changes in the treatment regimen to be made if necessary.
Inhaled therapy is preferred to systemic treatment as the drug is preferentially delivered to the respiratory tract15. According to a meta-analysis on the available literature, glucocorticoid treatment significantly improves equine asthma with no difference in efficacy between systemic and inhaled administration of the medication13. A difference in the rate of response will, however, occur, with systemic administration inducing a more rapid response than inhaled medications – further supporting the use of systemic corticosteroids in acute cases of severe equine asthma13. The same meta-analysis failed to identify a difference in efficacy between drug delivery via metered dose inhalers or nebuliser13.
Metered dose inhalers provide an easy-to-use treatment method that is generally well-tolerated. Spacer devices are required and have been designed for horses. Human paediatric spacers are, however, a cost-effective alternative.
Inhaled fluticasone has been shown to be as effective as systemic dexamethasone in controlling clinical signs in horses with mild equine asthma, and decreasing BALF neutrophilia in horses with severe equine asthma9, and is the most effective of the inhaled formulations of glucocorticoid with the longest duration of action. While other studies have found conflicting results on improvement of BALF neutrophilia with both fluticasone and dexamethasone, improved airway hyper-reactivity with treatment with both medications is a consistent finding2.
Bronchodilators can also be administered via inhalation to provide direct administration to the airways; however, in mild or chronic cases, they may offer little benefit over treatment with glucocorticoids alone. In the authors’ experience compliance with metered dose inhalers is often poor and results are less consistent than with use of a nebuliser.
Nebulisation has become a popular means of managing equine asthma (Figure 7). While considerable cost is associated with the purchase of a nebuliser, the ongoing treatment cost is markedly reduced, compared to either systemic or metered-dose inhaled treatment. Provided they are effectively disinfected, nebulisers can be used for multiple horses.

Human research has demonstrated similar efficacy of nebulised dexamethasone to oral prednisolone in managing asthma, and in horses little absorption occurs and the effect is minimal on the hypothalamic-pituitary-adrenal axis associated with treatment, thereby reducing the risk of adverse effects compared to systemic treatment15. The inhalation of injectable dexamethasone preparations is well tolerated and does not incite an inflammatory response14. Injectable dexamethasone is typically used at 20% of the systemic dose when nebulised and is diluted in an equal volume of saline.
Fluticasone may be more effective than dexamethasone, but is harder to obtain and more expensive than dexamethasone. All inhaled medications are used off-licence and should be used with appropriate consent in accordance with the cascade. Panel 2 provides an indication of doses for inhaled medications.
1. Emergency case in respiratory distress
A. Atropine 0.02mg/kg IV or N-butylscopolamine 0.3mg/kg IV
and
B. Dexamethasone 0.1mg/kg IV
2. Acute case with increased respiratory effort
A. Dexamethasone tapering from 0.1mg/kg IV/IM sid to 0.05mg/kg IV/IM every other day or prednisolone 1mg/kg to 2mg/kg PO sid
and
B. Clenbuterol 0.8ug/kg to 3ug/kg orally
q12h or (if respiratory function is adequate) salbutamol 10 actuations via metered dose inhaler (MDI) q12h to 24h for a 500kg horse.
3. Chronic case with little or no increase in respiratory effort
A. Dexamethasone 0.01mg/kg nebulised
sid with equal volume saline or fluticasone 10 actuations via MDI sid to bid for a
500kg horse (or equivalent via nebuliser)
and possibly
B. Salbutamol 10 actuations via MDI q12h to 24h for a 500kg horse.
*Other options are available. The doses are those used most frequently by the authors and are not licensed doses. Only prednisolone is licensed for treating equine asthma.
In summary, inhaled glucocorticoids should be considered the mainstay of long-term management of equine asthma with systemic glucocorticoids and possibly bronchodilators used intermittently as required during periods of exacerbation. The provision of omega-3 fatty acids may also have some benefit alongside environmental management in controlling mild airway inflammation3, 6, but probably offer poor value for money.
Conclusion
Equine asthma can be a serious and debilitating condition. While environmental management underpins the overall success of management, owner compliance and understanding of what is required to achieve appropriate environmental management is often poor. A tendency also exists for bronchodilators to be used at the expense of glucocorticoids – thereby reducing the efficacy of treatment. Inhaled glucocorticoids should be the mainstay of long-term therapeutic management of these cases with nebulised dexamethasone providing the most convenient and cost-effective option.
Early and accurate diagnosis is important, and to achieve this it is worth being proactive in performing bronchoalveolar lavage and not simply relying on tracheal wash cytology. Regular monitoring is important as many cases may suffer chronic mild clinical signs that may reduce their performance, compromise their welfare and result in the development of irreversible pulmonary damage.
References
- Cian F, Monti P and Durham A (2015). Cytology of the lower respiratory tract in horses: an updated review, Equine Vet Educ 27(10): 544-553.
- Mazan MR (2018). Lower airway disease in the athletic horse, Vet Clin North Am Equine Pract 34(2): 443-460.
- Richard EA and Robinson NE (2016). Inflammatory airway disease congress: one syndrome, multiple pathways: A Dorothy Russell Havemeyer Symposium, Equine Vet Educ 28(1): 9-12.
- Couëtil LL, Cardwell JM, Gerber V et al (2016). Inflammatory airway disease of horses – revised consensus statement, J Vet Intern Med 30(2): 503-515.
- Arroyo MG, Couëtil LL, Nogradi N et al (2016). Efficacy of inhaled levalbuterol compared to albuterol in horses with recurrent airway obstruction, J Vet Intern Med 30(4): 1,333-1,337.
- Nogradi N, Couëtil LL, Messick J et al (2015). Omega-3 fatty acid supplementation provides an additional benefit to a low-dust diet in the management of horses with chronic lower airway inflammatory disease, J Vet Intern Med 29(1): 299-306.
- Mazan MR (2015). Update on noninfectious inflammatory diseases of the lower airway, Vet Clin North Am Equine Pract 31(1): 159-185.
- Tanquerel L, Fillion-Bertrand G, Lavoie JP and Leclere M (2018). Effects of magnesium sulfate infusion on clinical signs and lung function of horses with severe asthma, Am J Vet Res 79(6): 664-673.
- Léguillette R, Tohver T, Bond SL et al (2017). Effect of dexamethasone and fluticasone on airway hyperresponsiveness in horses with inflammatory airway disease, J Vet Intern Med 31(4): 1,193-1,201.
- Hewson J and Arroyo LG (2015). Respiratory disease: diagnostic approaches in the horse, Vet Clin North Am Equine Pract 31(2): 307-336.
- Siegers EW, Anthonisse M, van Eerdenburg FJCM et al (2018). Effect of ionization, bedding, and feeding on air quality in a horse stable, J Vet Intern Med 32(3): 1,234-1,240.
- Bullone M, Murcia RY and Lavoie JP (2016). Environmental heat and airborne pollen concentration are associated with increased asthma severity in horses, Equine Vet J 48(4): 479-484.
- Calzetta L, Rogliani P, Page C et al (2018). Clinical effect of corticosteroids in asthma-affected horses: a quantitative synthesis, Equine Vet J 50(5): 594-601.
- de Lagarde M, Rodrigues N, Chevigny M et al (2014). N-butylscopolammonium bromide causes fewer side effects than atropine when assessing bronchoconstriction reversibility in horses with heaves, Equine Vet J 46(4): 474-478.
- Haspel AD, Giguère S, Hart KA et al (2018). Bioavailability and tolerability of nebulised dexamethasone sodium phosphate in adult horses, Equine Vet J 50(1): 85-90.
- Leclere M, Lefebvre-Lavoie J, Beauchamp G and, Lavoie JP (2010). Efficacy of oral prednisolone and dexamethasone in horses with recurrent airway obstruction in the presence of continuous antigen exposure, Equine Vet J 42(4): 316-321.
- Couroucé-Malblanc A, Fortier G, Pronost S, Siliart B and Brachet G (2008). Comparison of prednisolone and dexamethasone effects in the presence of environmental control in heaves-affected horses, Vet J 175(2): 227-233.
- Mainguy-Seers S, Picotte K and Lavoie JP (2018). Efficacy of tamoxifen for the treatment of severe equine asthma, J Vet Intern Med 32(5): 1,748-1,753.
