15 Nov 2019
Karin Kruger discusses the pathophysiology of a variety of upper and lower tract conditions that can cause distress in horses, and the need for calm assessment to ensure favourable outcomes.

Image © LUM3N / Pixabay

Horses have a massive respiratory reserve, but true respiratory emergencies can arise for a variety of reasons, requiring rapid and decisive action.
When presented with a horse in respiratory distress, the author first tries to establish whether the primary problem is in the upper respiratory tract, lower respiratory tract or both. Wounds, swellings, nasal discharge, patient history and a brief examination will provide helpful clues.
Unless the horse is hypotensive, a small amount of acepromazine helps to take the edge off the horse’s distress. If the horse is not a danger to itself or others, further sedation should be avoided.
In cases with an upper respiratory condition and severe respiratory distress, a quick tracheostomy will bypass the problem and allow the horse to resume normal respiration until the underlying problem can be resolved.
Upper airway endoscopy is the diagnostic test of choice to resolve various aetiologies, and radiography and ultrasound frequently adds valuable information.
In horses with severe lower respiratory disease, thoracic auscultation may be sufficient to make a preliminary diagnosis, which is supported by ultrasound and radiography. Careful auscultation of the entire lung field may reveal musical wheezes (bronchospasm), crackles (fluid or exudate in the airway), the absence of breath sounds ventrally (pleural effusion or lung consolidation), or the absence of breath sounds dorsally (pneumothorax or lung consolidation).
Upper airway obstruction is often associated with an abnormal respiratory noise and can result from obstruction of any part of the upper respiratory tract.
Conditions that result in nasal obstruction include trauma, bilateral jugular thrombosis, bee sting, adverse reaction to intranasal vaccination and snake bites.
If the nostrils are not yet occluded at the time of examination, but severe swelling is anticipated, a small tube placed in the nasal passage may be sutured to a nostril – or a nasotracheal tube placed – to prevent obstruction of the airway. Although not all horses will tolerate this, the author has been surprised at how well some standing horses have tolerated a nasotracheal tube.
Applying ice packs, or spraying epinephrine or phenylephrine into the nostrils, may also decrease swelling.
It is important to keep the horse’s head level or elevated to prevent dependent oedema.
Alpha-2 adrenergic agonists – particularly xylazine or detomidine – should be avoided because they lower the head, causing increased swelling and airway resistance.
In bee sting emergencies, dexamethasone and epinephrine may be indicated. Antibiotics, flunixin meglumine and tetanus toxoid can be considered if the skin is broken.
If adder bite cases are seen within eight hours, antivenin may be considered.
Epistaxis is caused by guttural pouch mycosis, ethmoid haematoma, trauma, neoplasia, exercise-induced pulmonary haemorrhage or a severe thrombocytopenia/coagulopathy.
Due to the potential of guttural pouch mycoses to cause rapid exsanguination, the author considers all nosebleeds (especially recurrent ones) to be emergencies.
Cases with epistaxis should have an endoscopic examination to determine the origin of the haemorrhage. If the haemorrhage originates from a guttural pouch, the horse should be referred for immediate arterial coil embolisation.
Laryngeal or pharyngeal obstruction can occur as a result of laryngeal oedema secondary to anaphylaxis, epiglottic or arytenoid disease, laryngeal paresis or paralysis, guttural pouch tympany, retropharyngeal lymph node enlargement (strangles or lymphosarcoma), proximal oesophageal obstruction (choke), pharyngeal trauma, hyperkalaemic periodic paralysis and neoplasia.
Anaphylaxis in horses is, thankfully, rare, but has been reported in association with antibiotic administration and after iatrogenic IV milk infusion in a foal (Alcott and Wong, 2010; Basile et al, 2015). Clinical signs include urticaria, dyspnoea, tachycardia, eyelid oedema and hypotension, which is sometimes followed by colonic tympany (colic) and laminitis.
As in other species, anaphylaxis is treated with epinephrine (3ml to 7ml IV/IM/SC of 1:1,000 for 450kg horse) and dexamethasone (0.1mg/kg to 0.2mg/kg IV bolus).
If the airway has not yet occluded, but swelling is progressive, a nasotracheal tube may be passed to prevent complete occlusion, or a tracheostomy can be performed.
Pulmonary oedema may develop secondary to upper respiratory obstruction; oxygen therapy is often needed in these cases.
IV colloids and crystalloids, as well positive inotropes and vasopressin, may be indicated in cases with systemic hypotension.
Severe lower respiratory disease results in respiratory distress with or without respiratory noise and cough.
Pneumothorax and pleural effusion decrease the lung’s ability to expand, which causes rapid shallow breathing. In either case, fluid or air should be drained or suctioned from the pleural space using a chest drain (Figure 1) to allow re-expansion of lungs. The author uses ultrasound guidance to optimise drain positioning.

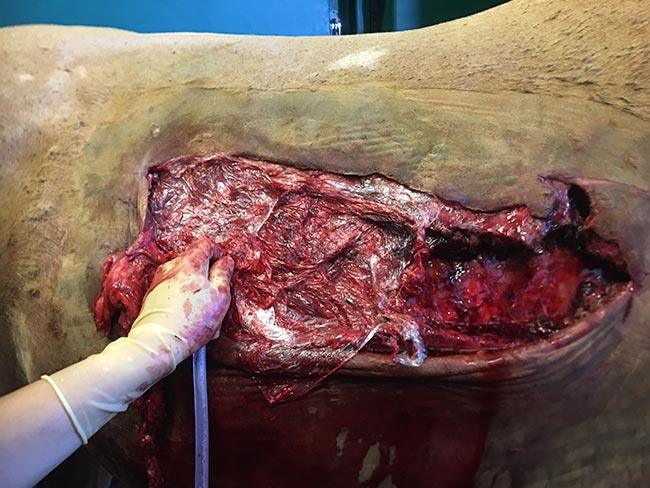
In cases of an open chest wound, cling film can be held over the defect while the horse is stabilised and the damage assessed (Figure 2).
Chest drains can be attached to active suction (in the case of pneumothorax) or a one-way valve (pleuropneumonia) for continuous drainage of air or fluid from the chest.
Pneumothorax in horses is seen following pleuropneumonia, open and closed thoracic trauma, and rarely after upper respiratory surgery or idiopathically. Clinical signs include increased respiratory rate, effort and distress, tachycardia, depression or anxiety, decreased lung sounds in the dorsal aspect of the thorax, an increased abdominal effort, nostril flare and an abnormal mucous membrane colour (Boy and Sweeney, 2000).
Comprehensive treatment of pleuropneumonia is beyond the scope of this article, but initial treatment may consist of fluid drainage, broad-spectrum antimicrobials, restoration of circulating volume and intranasal oxygen (Tomlinson et al, 2015a; 2015b; Arroyo et al, 2017).
Pulmonary oedema results from smoke inhalation, heart failure, trauma, upper airway obstruction, viral infections, head trauma or iatrogenic overzealous fluid administration. Hypoxaemia is common with pulmonary oedema.
Additionally to treating the underlying cause, the author treats most cases of pulmonary oedema with furosemide (1mg/kg IV), dexamethasone (0.1mg/kg) and intranasal oxygen (10ml/kg/min to 20ml/kg/min).
Endobronchial suction and bronchodilators can also be considered to improve ventilation (Senior, 2005).
The American-European Consensus Committee defined acute lung injury/acute respiratory distress syndrome (ALI/ARDS) in humans as a condition characterised by (Bernard et al, 1994):
In a case series of 15 foals with ALI/ARDS, an underlying bacterial, viral or fungal infection could be identified in 10 of 15 foals. Treatments varied, but all included aggressive intranasal oxygen, antimicrobials and anti-inflammatories (mostly corticosteroids). Additional treatments included nebulised furosemide, salmeterol, albuterol, fluticasone and gentamicin sulphate (Dunkel et al, 2005).
In adult horses, ALI/ARDS is seen in aspiration pneumonia (for example, being tubed in with mineral oil), viral infection, smoke inhalation, or secondary to severe viral or bacterial respiratory disease. In foals, sepsis, pneumonia, prematurity, meconium aspiration and fractured ribs have been implicated in the development of this condition.
Severe, acute bronchoconstriction – with varying degrees of inflammation and excessive mucous production – can occur in horses suffering from severe equine asthma (heaves).
In an acute emergency, the author uses IV corticosteroids and inhaled bronchodilators to reduce airway inflammation and relieve bronchospasm.
N-butylscopolammonium bromide (NBB) is a potent bronchodilator, reaching maximum effect 10 minutes after IV administration. This effect dissipates within one hour of drug administration (Couetil et al, 2012).
Atropine has traditionally been used to determine the reversibility of bronchospasm in severely asthmatic cases, but its use in horses is associated with undesirable side effects, such as gastrointestinal ileus.
One study indicated the bronchodilatory properties of NBB were not statistically different from those of atropine, but were of shorter duration. NBB was associated with fewer systemic side effects; therefore, it was preferred over atropine when assessing the reversibility of airway obstruction in horses (de Lagarde et al, 2014).
Severe respiratory distress in the horse has many diverse causes. Initial appropriate stabilisation of the patient will allow everyone to take a breath while the underlying cause, treatment plan and prognosis are determined.
Although the sight of a horse in respiratory distress can be quite traumatic for both owner and vet, a calm and logical assessment – and appropriate intervention – will provide the basis for a favourable outcome.