20 Jan 2020
Louise Northway reinforces the scale of anaesthetic role veterinary nurses play, as well as possibilities for further training and advanced physiological parameters that can be monitored.

Monitoring anaesthesia is a key part of many of our working days. In the author’s opinion, it is one of the biggest – if not the biggest – responsibilities we have.
The RCVS Code of Professional Conduct for Veterinary Surgeons states the vet has ultimate responsibility in the maintenance and monitoring of anaesthesia; however, the author strongly feels this task is very much a joint responsibility.
RVNs should feel empowered to feel like more than “just” the person who acts as the hand of the vet to turn the vaporiser dial.
The code reads: “Maintaining anaesthesia is the responsibility of a veterinary surgeon, but a suitably trained person may assist by acting as the veterinary surgeon’s hands (to provide assistance which does not involve practising veterinary surgery), for example, by moving dials.”
However, RVNs do – and know – so much more than this. Tasks VNs may undertake include:
However, the aforementioned must be performed under the direction of the vet, in accordance with the RCVS Code of Professional Conduct for Veterinary Surgeons (Panel 1).
Veterinary nurses and student veterinary nurses may be directed to assist veterinary surgeons with the maintenance of anaesthesia and the monitoring of patients under anaesthesia. The following advice applies to these tasks:
a. Inducing anaesthesia by administration of a specific quantity of medicine directed by a veterinary surgeon may be carried out by a veterinary nurse or, with supervision, a student veterinary nurse, but not any other person.
b. Administering medicine incrementally or to effect, to induce and maintain anaesthesia may be carried out only by a veterinary surgeon.
c. Maintaining anaesthesia is the responsibility of a veterinary surgeon, but a suitably trained person mau assist by acting as the veterinary surgeon’s hands (to provide assistance which does not involve practising veterinary surgery), for example, by moving dials.
d. Monitoring a patient during anaesthesia and the recovery period is the responsibility of the veterinary surgeon, but may be carried out on his or her behalf by a suitably trained person.
e. The most suitable person to assist a veterinary surgeon to monitor and maintain anaesthesia is a veterinary nurse or, under supervision, a student veterinary nurse.
As an RVN, the author believes VNs should be encouraged to not only point out abnormalities, but also play an active part in the discussion of what may be causing the problem and what the best intervention may be.
Detecting abnormalities is crucial, but so is having the understanding to remedy them. Communication and collaboration of knowledge between you and your vet is imperative, for the benefit of the patient.
To do that, RVNs should feel empowered to undertake further anaesthesia training after qualifying, as the need to learn more still exists. This is a niche area you can use every day. Why? Because it helps support the vet in his or her role, improves patient management and care, and gives you satisfaction in being able to implement and use your niche area of knowledge.
You may be working in a practice that has limited or no additional electronic monitoring equipment. However, we should all be pushing to increase the level of care we provide to our patients, and the proper use of multiparameter monitoring equipment helps with this.
Advanced monitoring equipment can detect abnormalities and problems we simply could not know without, and gives us earlier warnings of developing problems.
You may think: “Well, I’ve never had a multiparameter monitor before, so why do I need one now?”
It’s only when you learn about just how much additional information it can provide, you realise the importance. When you start using such a monitor you will soon see patients often require a small amount of intervention during the anaesthetic period; for example, to correct a period of hypotension or hypoventilation. It would be almost impossible to detect these without an electronic monitor.
From a basic monitoring perspective, VNs monitor:
Meanwhile, with the use of advanced electrical monitoring equipment:
Let’s touch on two of the additional advanced physiological parameters we can monitor.

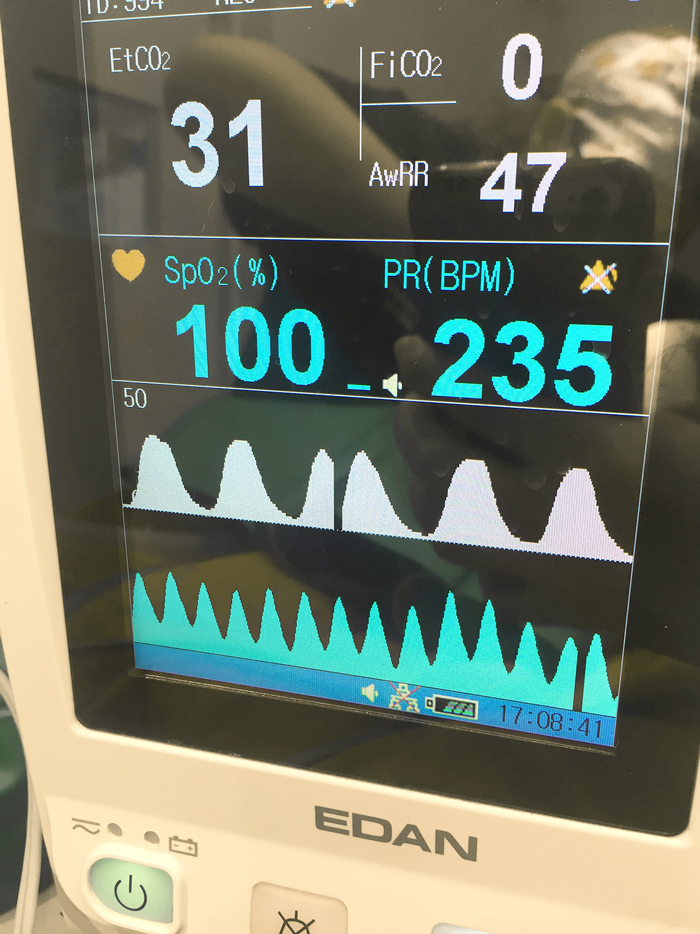
Capnography is the measurement and graphical display of the amount of CO2 in the respiratory gases. The capnograph is the author’s favourite piece of monitoring equipment. Capnography helps assess the adequacy of ventilation, as well as providing indirect information on cardiac output, circulation and cellular respiration.
Respiratory “rate” alone does not tell us if ventilation is adequate – but capnography can guide us. For example, a patient with 12 breaths per minute could be breathing at a normal rate, but taking very short and shallow breaths – and, therefore, effective gaseous exchange is not taking place.
The basic assumption we make with capnography is the ET value is the same as alveolar, which, in most cases, it is. But if the animal is taking shallow breaths, the ET value won’t be a true reflection of alveolar because it’ll be more like dead space gas. It’s only when we give the animal a nice deep breath that we can see what the true alveolar value is – the ETCO2 often increases in these situations.
Generally, hypoventilation results in hypercapnia (ETCO2 more than 45mmHg) due to a reduced ability to void CO2. Hyperventilation often results in hypocapnia as the patient will be voiding more CO2.
The amount of CO2 in the blood can also be affected by the patient’s body temperature and metabolic rate. Metabolic rate is affected by body temperature, so the lower the temperature, the slower the production of CO2; the warmer the temperature, the faster the production of CO2.
Capnography can also provide indirect information on cardiac output and circulation. If you remember the only way CO2 can return to the lungs is if it is pumped in the venous circulation by the heart then if you see a sudden decline in ETCO2, it may be the heart is pumping blood less effectively or less circulating volume is returning to the heart.
Another point to make is if a patient is being manually or mechanically ventilated and a sudden increase in ETCO2 occurs – this is likely to be related to an increase in circulation, metabolism or cardiac output (Farry and Norkus, 2019).

Prolonged hypercapnia causes direct vasodilation. It can also cause a respiratory acidosis due to being a higher amount of CO2 present in the blood. However, most CO2 is transported in the blood as an acid (carbonic acid) prior to being exhaled as CO2 gas.
Permissive hypercapnia involves tolerating a slightly above normal ETCO2. The vasodilation is compensated by an increase in sympathetic tone – a result of the acidosis. Vasodilation may help improve perfusion and oxygen delivery, but can be devastating in cases where an increase in intracranial pressure (ICP) exists, such as head trauma or brain tumour patients. This is because any increase in intracranial blood volume (caused by the vasodilation) increases ICP even more (Hopper, 2017).
Healthy patients may tolerate an ETCO2 of 50mmHg to 60mmHg if other clinical parameters are within normal limits, but this information should still be communicated to the vet.
Prolonged hypocapnia (ETCO2 lower than 35mmHg) causes vasoconstriction and can reduce blood flow to the brain. In addition, if a patient is voiding a lot of CO2 (which, remember, is an acid) they may develop a respiratory alkalosis.
Increasing your patient’s minute volume to encourage a lower ETCO2 (30mmHg to 35mmHg) may be advantageous in patients with head trauma or neoplastic cerebral processes due to the reduction in intracranial pressure from vasoconstriction (Sager and Norkus, 2019).
The shape of the capnography waveform can also give valuable information about many other things that may be going on with the patient. For example:
A systolic arterial pressure of 90mmHg and mean arterial pressure (MAP) of 70mmHg to 80mmHg is necessary to provide the tissues and vital organs with blood (O’Dwyer and Aldridge, 2013).
Volatile inhalation agents cause dose-dependent vasodilation and, therefore, if used in excess, can contribute to arterial hypotension in the anaesthetised patient.
“Balanced anaesthesia” is the use of smaller doses of a combination of drugs to achieve the various components of anaesthesia (narcosis, analgesia and muscle relaxation), therefore reducing the disadvantages of using large doses of any one drug.
Providing multimodal analgesia (using two or more analgesics that target different parts of the pain pathway) enables a lower percentage of volatile agent to be used, which helps reduce the dose-dependent side effects.
If you are not measuring arterial blood pressure in practice, it is very important to push to make this change. You will see interventions are very often required to help support your patient.
From a day-to-day perspective, geriatric animals make up a big group of patients who may have a level of underlying renal or other organ dysfunction. The standard blood screens we perform in practice for renal disease tend to only show an abnormality when 75% of nephrons (kidney cells) have been damaged. An episode of unaddressed hypotension under anaesthesia could cause further renal damage – but we can help protect our patients if we monitor their blood pressure and respond effectively.
When discussing the possible interventions, consider what part of the following equation is affecting your patient’s blood pressure:
MAP = (cardiac output × systemic vascular resistance)
Is your patient vasodilated due to the drugs given – for example, acepromazine or isoflurane? Is it because the patient is hypovolaemic and, therefore, stroke volume is reduced? Is the patient bradycardic due to the drugs administered, with a concomitant reduction in cardiac output? Is it hypothermic? Because this can also lead to bradycardia and hypotension.
As RVN Courtney Scales said at SVN FEST 2019: “Think about whether it is the pump or the pipes” (whether it is the pump – heart, or pipes – vasculature). Therefore, remember a fluid bolus is not always the solution to addressing hypotension.
To summarise:
Planning and forethought are key before anaesthetising any patient. Take time to discuss the patient with the vet prior to induction. What do you expect? What interventions may be required? Do we have everything we may need? Have your checklists been completed?
The relationship and communication between the RVN and vet is vitally important. Although we must adhere to the codes of professional conduct, the opportunities for professional clinical discussion and planning are endless.
In this article, we have only discussed two of the clinical measurements we can look at; we haven’t even touched on ECG or pulse oximetry. The author hopes you can appreciate just how much better prepared you will be if your practice invests in advanced monitors.
The author believes RVNs, in collaboration with their vets, are key to enhancing patient safety and improving anaesthetic outcomes for patients. Discussion of possible complications and interventions will help to build knowledge and trust between colleagues, and improve patient outcomes in the process.
Nurses should value their knowledge and clinical skills, and share them with their team. While the skills and knowledge of the RVN alone are paramount, the use of advanced monitors, along with a thorough understanding of the information they can provides is essential.
Multiparameter monitors have no purpose unless you understand what the information means. If that is not the case, the monitor will simply be a distraction from basic clinical measurements.
Arrange for some CPD for you and your team to make the most of your equipment – the author believes they are much needed to help us do our jobs even better.
The author’s view is that, in the future, the use of electronic multiparameter monitoring equipment should become a standard requirement in every patient that undergoes an anaesthetic, no matter whether it is in a referral or first-opinion setting. In addition, the author hopes monitoring anaesthesia is delegated specifically to RVNs or SVNs (with another RVN present for support) who can work in collaboration with the vet to monitor the patient – and, when necessary, intervene effectively to the best of their combined ability.
Lou Northway
Job Title