20 Aug 2018
Anaesthesia in asthmatic feline patients
Robyn Thomson and Derek Flaherty guide readers through the stages and considerations for anaesthetising cats diagnosed with asthma.

Asthma is a common inflammatory condition of the airways in cats, and can result in bronchospasm/bronchoconstriction when these patients undergo general anaesthesia. Appropriate management and treatment in the perioperative period is, therefore, essential to ensure a favourable outcome.
Stabilisation of asthma prior to general anaesthesia can reduce the risk of bronchoconstriction, but does not eliminate it entirely. Commonly used medications are corticosteroids and beta-2 agonists. Pre-stabilisation is not always possible, though, as use of corticosteroids can interfere with diagnosis.
Induction of anaesthesia, following preoxygenation, can be carried out using the majority of induction agents. However, it is essential to ensure adequate “depth” prior to instrumentation of the airway as “light” anaesthesia at this point can induce bronchoconstriction. Alternatively, a supraglottic airway device can be used. Recognition of bronchoconstriction is essential in these patients. Changes in respiratory pattern, airway resistance and capnogram trace can all allude to bronchoconstriction having occurred. In the event it does arise, 100 per cent oxygen should be provided and any stimulus (for example, surgery) discontinued, if possible.
Anaesthetic depth should be “deepened” if any doubt exists as to its adequacy and intermitted positive pressure ventilation instituted. If possible, an inhaled beta-2 agonist should be administered – or, alternatively, terbutaline or adrenaline can be given IM or IV.
Tracheal extubation should follow anaesthesia at a relatively “deep” plane of anaesthesia and oxygen provided, if necessary.
Feline asthma is an inflammatory condition affecting the lower airways (Trzil and Reinero, 2014). It is suspected to be the result of a type one hypersensitivity reaction to allergens, with eosinophils being the main driving force (Venema and Patterson, 2010).
The distinguishing features of asthma from other forms of lower airway disease are reversible bronchospasm or bronchoconstriction and airway hyperreactivity, accompanied by increased mucus production, and hypertrophy of the smooth muscle and mucous glands (Brainard and King, 2010; Venema and Patterson, 2010).
Asthma is considered one of the most common respiratory disorders in cats, affecting between 1% and 5% of the population (Trzil and Reinero, 2014); however, the true incidence is probably significantly higher, as owners may not always seek veterinary consultation due to the intermittent nature of the condition and – in some cases – the presence of only relatively minor clinical signs.
In addition, even with appropriate investigation, a proportion of cats may not be identified as asthmatic, given potential difficulties in achieving a definitive diagnosis.
Given the relatively high incidence of asthma in cats, it is not uncommon for individuals to be presented for anaesthesia – either for unrelated procedures, such as dentistry; or for investigations, such as bronchoscopy and/or bronchioalveolar lavage – in an attempt to diagnose the patient as asthmatic, with a view to instigating appropriate treatment. The risk of bronchoconstriction in human patients with asthma undergoing anaesthesia is 2%, compared with an overall incidence of 0.2% (Looseley, 2011).
Although severe perioperative bronchospasm appears relatively uncommon in asthmatic cats undergoing anaesthesia, when it does occur, it may be life-threatening, and it is vital close attention is paid to adequate pre-anaesthetic assessment and stabilisation, as well as avoidance of potential triggering factors.
Consequently, a high index of suspicion for asthma must always be maintained when anaesthetising cats with any history of previous respiratory signs, although some individuals may still develop bronchoconstriction during anaesthesia, even in the absence of any previous relevant history. It is, therefore, essential to be able to recognise and appropriately manage bronchospasm, should it occur during anaesthesia.
Pre-anaesthetic stabilisation
Cats previously diagnosed with asthma may be on various treatment regimens when presented for anaesthesia, including inhaled beta-2 agonist drugs, and inhaled and oral corticosteroids.
On the other hand, individuals undergoing diagnostic work-up for possible asthma may be on no treatment, and certain agents, such as corticosteroids, may have to be avoided prior to investigation, as they may interfere with accurate diagnosis from bronchial washes. It is likely the latter group is, therefore, at increased risk of bronchospasm during anaesthesia.
Even in cats receiving appropriate asthma treatment, and where symptoms are absent, it is likely exacerbations of the condition may be missed by owners, and control of the condition may be suboptimal in many cases; with such individuals, bronchospasm may still occur with appropriate triggering factors.
It is important to obtain a thorough history to be as confident as possible that the condition is well controlled before considering anaesthesia. Any possible respiratory infection (for example, feline influenza) within the previous month should be considered a contraindication to elective anaesthesia, as airway hyperreactivity may persist for several weeks following infection.
Use of oral corticosteroids for five days prior to general anaesthesia may reduce inflammation and subsequent wheezing postintubation in newly diagnosed asthmatics or those with poor compliance (Silvanus et al, 2004; Woods and Sladen, 2009). They can, however, interfere with obtaining a diagnosis,if that is the purpose of general anaesthesia.
If the cat has been on long-term corticosteroids for management for asthma prior to general anaesthesia, the risk of steroid-induced adrenal suppression should be considered, as these patients may be unable to mount a normal “stress response” to surgery/anaesthesia. Based on human guidelines, if corticosteroids have been administered for more than two weeks in the preceding six months and the cat is undergoing anaesthesia or surgery, steroid supplementation should be administered throughout the perioperative period.
Various recommendations regarding steroid dose and type are to be found in the literature (Trepanier, 2015; Veres-Nyeki, 2016), but the most practical is to administer dexamethasone at 0.1mg/kg IM at the time of premedication (or slightly before), with the same dose repeated at the end of the procedure if the cat has undergone major surgery. In any case, it is important to continue administering parenteral steroid supplementation until the oral route can be recommenced.
For cats that have not been receiving oral steroids for several months prior to anaesthesia, it is probably sufficient to administer parenteral steroids for 24 to 48 hours post-anaesthesia, with the longer duration being reserved for patients having more major procedures.
Unfortunately, the majority of pre-anaesthetic testing carried out in asthmatic humans to assess ventilatory function (for example, peak expiratory flow and forced expiratory time) are simply not feasible in animals – and, therefore, the clinician is almost entirely reliant on history and “basic” clinical examination when deciding if an asthmatic cat is suitably stable for anaesthesia.
Pre-anaesthetic medication (premedication)
Since anxiety or pain can trigger bronchospasm, it is important asthmatic cats receive adequate premedication. While acepromazine has an antihistamine effect, this is relatively mild and likely insufficient to provide any beneficial effect should histamine release occur (for whatever reason) during anaesthesia.
Therefore, while acepromazine is a suitable premedication agent for asthmatic cats, it should not be used on the basis it will protect against bronchospasm. The alpha-2 adrenoceptor agonists medetomidine and dexmedetomidine provide excellent anxiolysis and are sympatholytic – both of which may help reduce bronchospasm. These drugs are generally preferred over acepromazine by the authors when dealing with asthmatic cats (in the absence of other pathological conditions). The dose chosen is largely dependent on the temperament of the cat, but varies from approximately 5µg/kg to 20µg/kg of medetomidine IM, or around half of this if using dexmedetomidine.
The tranquilliser/sedative chosen should be combined with an opioid drug, even in patients undergoing non-painful procedures, such as radiography, as combining the two drug groups provides synergistic sedative effects. In general, a partial opioid agonist (butorphanol or buprenorphine) should be selected for non-painful procedures, while a full agonist (methadone) should be selected if the procedure is likely to be moderately to severely painful.
While pethidine is another full agonist licensed for use in cats, its propensity to cause histamine release would contraindicate its use in cats with asthma. Similarly, morphine may also cause histamine release – and, therefore, bronchoconstriction – although studies from human asthmatic patients show it may actually suppress bronchospasm in cases of mild asthma (Woods and Sladen, 2009). However, morphine is not licensed for veterinary use, and no justification would exist for selecting it over methadone for the vast majority of cases.
Controversy exists in the human literature regarding use of antimuscarinics (atropine or glycopyrronium) for premedication in asthmatic patients. While these drugs cause a vagolytic-mediated bronchodilation and help dry airway secretions, they tend to “thicken” the secretions produced, and these may then be more difficult to clear from the airway. Based on the limited evidence of any beneficial effect of these drugs in asthmatic patients, the authors do not use them for premedication of asthmatic cats.
Use of beta-2 agonist drugs, such as terbutaline or salbutamol (also known as albuterol), prior to anaesthesia is likely to be of benefit, as they may improve air flow by dilating narrowed airways, which may be present in asthmatic cats, where some degree of underlying bronchospasm many be present. These bronchodilators can be given via a meter dose inhaler and a spacer device (Figure 1) approximately 5 to 10 minutes before induction of anaesthesia.

Depending on the cat’s temperament, the mask can be placed over the cat’s face, one puff of the inhaler ejected into the spacer chamber and then the mask held in place for 10 to 15 seconds. If less amenable, one puff can be placed into the spacer, then the mask applied to the cat’s face and a second puff subsequently delivered into the chamber.
Induction of anaesthesia
Prior to induction of anaesthesia, secure IV access should be established to allow delivery of emergency drugs, if necessary, during the perioperative period (Figure 2).

In addition, preoxygenation for approximately three to five minutes prior to induction of anaesthesia should be considered obligatory in asthmatic cats (Figure 3), in case of bronchospasm developing following induction or tracheal intubation.

This is preferably performed using a snug-fitting face mask, but some cats will be intolerant of this, or become excessively stressed, in which case the procedure should be abandoned and flow-by oxygen used instead. Although the IV induction agents do not directly cause bronchoconstriction per se, any of them can act as a trigger in a susceptible patient.
Ketamine may be useful as it causes bronchodilation, but it must be used in combination with either an alpha-2 agonist or benzodiazepine (diazepam or midazolam) to offset its side effects (such as muscle rigidity, CNS stimulation, increased respiratory secretions). In most cases, little exists to recommend one induction agent over any other.
Perhaps the greatest risk factor associated with development of bronchoconstriction is instrumentation of the airway. Cats are susceptible to laryngeal spasm, which necessitates the routine use of local anaesthetic spray on to the glottis prior to tracheal intubation, but passage of an endotracheal tube may still trigger bronchospasm.
It is important an adequate depth of anaesthesia is achieved in asthmatic cats both before spraying local anaesthetic or attempted endotracheal intubation, and it is probably wise to have cats slightly “deeper” than might normally be required due to the increased risk of bronchospasm occurring when the airway is stimulated. Certainly, “light” anaesthesia should be avoided.
The use of inhaled and IV lidocaine has been used in humans prior to instrumentation of the airway to reduce the risk of laryngeal spasm; however, in cats, IV lidocaine can result in marked cardiovascular depression, so should be avoided (Pypendop and Ilkiw, 2005).
An alternative to tracheal intubation is the use of a supraglottic airway device. These devices sit over the larynx, creating a seal, and allow oxygen and volatile anaesthetic agent to be administered to the patient. Not only are these devices unlikely to induce laryngeal spasm in cats (since they don’t pass through the glottis), but bronchospasm is also less likely in asthmatic patients, since they are less stimulating to the airway than endotracheal tubes.
This is not to say bronchospasm cannot occur in patients where a supraglottic airway is used, as other factors – such as “light” anaesthesia or inadequate analgesia during a procedure – may also play a role. If bronchospasm does occur while using a supraglottic airway device, mechanical ventilation is still possible, but a relatively low inflation pressure should be used, given the risk of gaseous dilation of the stomach.
Maintenance of anaesthesia
Volatile agents, such a sevoflurane and isoflurane, may be used as maintenance agents for anaesthesia in asthmatic cats, as they result in bronchodilation and may, therefore, provide some degree of protection against bronchoconstriction.
Of the two, sevoflurane is less irritating to the airway so may be preferential. Although sevoflurane is not licensed for feline administration, its use can be justified in asthmatic cats under the cascade. Ensuring adequate “depth” of anaesthesia throughout the procedure is essential, as bronchospasm may be precipitated at any point if anaesthesia is too “light”.
Other considerations
Depending on the reason for anaesthesia, an array of other drugs may be used – many of which can result in undesirable effects. All drugs have the potential to result in anaphylaxis; and, therefore, if any drug sensitivities are known, these agents should be avoided. Although not extensively used in veterinary practice, neuromuscular blocking agents (NMBAs) are the commonest cause of perioperative allergic reactions in humans, with bronchoconstriction being one potential consequence.
Although (for a variety of reasons) they are potentially less likely to provoke anaphylactic reactions in animals, consideration should still be given to the drug chosen if they are required, and agents inducing histamine release (for example, atracurium) should be avoided in favour of aminosteroidal relaxants (rocuronium and vecuronium).
Reversal of NMBAs is usually performed by administration of anticholinesterase drugs, such as neostigmine or edrophonium, in combination with an antimuscarinic (atropine or glycopyrronium); however, the anticholinesterases can trigger bronchoconstriction, so it may, therefore, be preferable to allow NMBAs to wear off spontaneously in asthmatic patients, where possible, rather than attempting reversal.
NSAIDs must also be used with caution in asthmatic cats. NSAIDs result in decreased production of prostaglandins through inhibition of the enzyme cyclooxygenase, but this may, in turn, lead to increased production of another group of inflammatory mediators – the leukotrienes – which play a key role in the genesis of bronchoconstriction in asthma. Indeed, leukotriene receptor antagonists are widely used in human asthmatics as an “add-on” therapy where standard treatment is poorly effective.
The use of NSAIDs in asthmatic patients is also questionable on the basis they would limit the potential use of corticosteroids in the perioperative period. If a patient has been on long-term NSAIDs, ideally, these should be stopped several days prior to anaesthesia, if possible, and gastric protectants administered in case corticosteroids have to be administered in the perioperative period.
Recognition of bronchospasm
While it is possible to reduce the risk of bronchospasm in cats with reactive airway disease, in some patients it may still, unfortunately, occur. Rapid recognition and treatment is key to a positive outcome (Panels 1 and 2).
- Prolonged expiration with increased abdominal effort
- “Shark fin” appearance on capnograph
- Change in respiratory rate and pattern
- Apnoea
- Increase in pressure within the airways
- Increased manual ventilation resistance
- Increased peak airway pressure when mechanically ventilating
- Can also be seen on spirometry as increased resistance
- Rule out other airway obstruction causes
- Provide 100% oxygen as carrier gas
- Increase anaesthetic depth by increasing volatile agent
- Initiate intermittent positive pressure ventilation
- Administer bronchodilator – inhaled metered dose inhaler via endotracheal tube and/or beta-2 agonist IV
Bronchospasm can manifest in several ways and recognition will be based on monitoring equipment available. Clinically, it may present as exaggerated ventilation with increased abdominal effort – particularly evident during expiration (Looseley, 2011).
This can be visualised if watching movement of the cat’s chest, but is less likely to be noticed if the animal is under surgical drapes. Some cats may become apnoeic with bronchospasm.
As many potential causes of apnoea exist in the anaesthetised patient, this is of low specificity for bronchospasm; but, in susceptible patients, should lead to a high index of suspicion. Ventilation of the apnoeic patient can give more indication if bronchospasm has occurred, as it results in increased resistance to breathing – this may be felt when squeezing the reservoir bag of the anaesthetic breathing system with manual ventilation, and seen by an increase in peak airway pressure with mechanical ventilation. While clinical signs may be suggestive of bronchospasm, the earliest alert is likely to be provided by capnography.
The prolonged expiration, due to narrowed airways, is visualised on a capnogram as a slow upward ascent during phase II of the graph, and a loss in the normal alveolar plateau (phase III) producing a “shark fin” appearance (Figure 4).
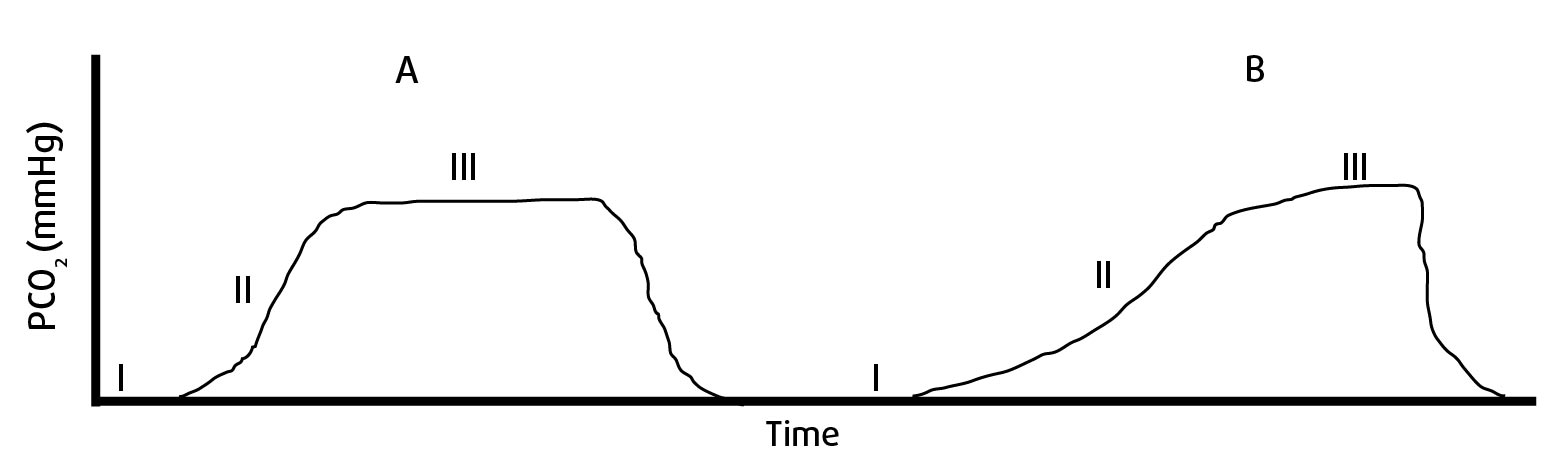
This type of trace can also be seen with other forms of airway obstruction; therefore, it is essential to rule out a kinked or blocked endotracheal (ET) tube (Looseley, 2011). This can be aided by straightening the cat’s head and neck as much as possible, and passage of a wide-bore urinary catheter down the ET tube to ensure patency.
In the absence of obvious ET tube obstruction, bronchoconstriction should be considered a likely cause of the abnormal capnogram trace and appropriate management instituted. Although not commonly available in vet practice, spirometry may also be used to identify increased airway resistance suggestive of bronchospasm; the graph will show increased expiratory pressure with decreased expiratory volume.
In animals that have been breathing supplemental oxygen, as is common during general anaesthesia, pulse oximetry is an extremely poor indicator that bronchospasm is occurring, and oxygen saturation will only decline late in the event. This is because, initially, sufficient oxygen dissolved in the plasma to ensure adequate haemoglobin saturation is still present. Once saturation begins to decline, however, the cat is in serious difficulty, and hypoxaemia is the usual terminal event in asthmatic cats during anaesthesia, unless successful treatment is rapidly instituted.
If bronchoconstriction is suspected, 100% O2 should be administered and any stimulation, such as surgery, stopped if possible (Looseley, 2011). Other possible increased airway resistance causes should be ruled out, such as a kinked ET tube, secretions within the ET tube and endobronchial intubation. Once an equipment fault has been ruled out, it is important to start managing the bronchoconstriction (Panel 2).
Anaesthesia should be deepened by means of a volatile agent, as this will, hopefully, reduce further airway stimulation. Volatile agents also have bronchodilator effects, so are beneficial in this situation. Intermittent positive pressure ventilation (IPPV) should be initiated, with rapid inspiration and prolonged expiration (Looseley, 2011). If possible, administration of an inhaled beta-2 agonist, using a metered dose inhaler via the ET tube, should be carried out.
A single puff should be used at a frequency up to once every 30 minutes throughout the remainder of anaesthesia, if required. If inhaled bronchodilators are not available or are ineffective, IV beta-2 adrenergic agonists should be used. Terbutaline can be administered at 10µg/kg to 15µg/kg IV or epinephrine at 1µg/kg to 2µg/kg IV, depending on what is available; tachycardia/tachyarrhythmias may result from administration of these agents.
Following effective management of bronchospasm, the patient should be recovered from anaesthesia, if safe to do so. If surgery is to continue, careful monitoring of anaesthetic depth should be carried out, ensuring the patient remains at an adequate depth.
Recovery
Anaesthesia recovery can be a high-risk period for development of bronchoconstriction. With a lightening plane of anaesthesia and stimulation of the airway by the ET tube, bronchospasm may occur at the time of extubation. To avoid this, extubation should occur at a “deeper” plane of anaesthesia than usual, and subsequent oxygen supplementation via face mask should be provided until the cat has sufficiently recovered consciousness and ventilating normally.
Injectable induction agents should be at hand, as well as equipment to intubate the airway, should suspected bronchospasm ensue. If it does occur, the aforementioned treatment process (Panel 2) should be followed; however, these patients will not be intubated, so IPPV cannot be performed.
Oxygen should continue to be supplied by face mask – and, if the use of inhaled or IV bronchodilators is not effective at reversing bronchospasm, the patient should be re-intubated (or a supraglottic airway device inserted) to allow manual ventilation.
Summary
Bronchoconstriction is a known and serious complication of anaesthesia in cats with hyperreactive airways. Appropriate pre-anaesthetic management can reduce the risk of its occurrence, but does not eliminate it completely. The ability to recognise and appropriately manage bronchoconstriction is essential for a favourable outcome.
- Some drugs and combinations mentioned in this article are not licensed for veterinary use.
