8 Jul 2025
Ellie Kohut DipVN RVN APVN looks at updated guidelines and considerations, including on team roles and the importance of debriefing.

Image: sudok1 / Adobe Stock
Less than 6% of dogs and cats that experience cardiopulmonary arrest (CPA) in practice survive to discharge (Boller and Fletcher, 2012).
CPA requires immediate intervention with a swift patient assessment and initiation of cardiopulmonary resuscitation (CPR). However, successful CPR is not just about speed — it’s about teamwork, preparation and communication. This article will discuss all these aspects, alongside the updated reassessment Campaign on Veterinary Resuscitation (RECOVER) guidelines and the importance of debriefing.
Recover was developed to improve the quality and outcomes of veterinary resuscitation efforts (Jones N, 2014). The 2024 RECOVER guidelines provide an evidence-based approach to CPR, expanding on the original 2012 guidelines. While the core principles remain, the updates bring new clarity, improved structure and gives veterinary professionals confidence to provide both basic and advanced life support.
Basic life support (BLS) is implemented to sustain the cardiorespiratory system in patients that are apnoeic. This is done through external chest compressions and positive pressure ventilation. The patient size and anatomy affects the techniques used and effective BLS requires a structured and prompt response to maximise the chances of achieving return of spontaneous circulation (ROSC) and survival.
If a patient is found to be unresponsive, ensure there is no more than a 10 to 15-second delay before starting chest compressions (Yagi, 2025).
Advanced life support (ALS) involves the use of monitoring tools like electrocardiography and capnography to guide cardiovascular interventions. It includes procedures such as defibrillation when needed, establishing vascular access, administering medications, and using additional supportive therapies. Unlike BLS, ALS requires specialised equipment and techniques, making it suitable only for clinical settings (Burkitt-Creedon et al, 2024).
The summarised 2024 updates are as follows:
Chest compressions. The 2024 update introduces a stronger emphasis on the correct depth of compressions. Veterinary professionals are encouraged to adapt technique based on the patient’s chest shape, as this ensures more effective perfusion and reduces the risk of ineffective compressions due to poor hand placement or force distribution (Burkitt-Creedon et al, 2024).
Wide-chested patients should receive compressions at a depth of approximately 25% of the anterior-to-posterior chest diameter, rather than the standard one-third to one-half used for other body types. This adjustment is because in these animals, a significant proportion of the posterior chest is occupied by non-compressible structures (Yagi, 2025).
The 2024 guidelines now outline three chest compression techniques tailored for small dogs and cats, focusing on targeting the ventricles to maximise blood flow and minimise injury risk:
Traditional two-handed compressions are no longer advised for small patients due to the high risk of over-compression and injury (Yagi, 2025).
The rate in which compressions should be performed remains at 100 to 120 compressions per minute and delivered in two-minute cycles with minimal interruptions.
Ventilation protocols. The recommended rate remains at 10 breaths per minute, with each breath lasting approximately one second (1 breath every 6 seconds). While the 2012 guidelines promoted mouth-to-snout ventilation when intubation wasn’t possible (Hopper et al, 2012), the updated recommendations now advise using a tight-fitting face mask instead (Burkitt-Creedon et al, 2024).
This method is more effective at delivering oxygen and reduces the risk of infection to the rescuer. However, without access to a tight-fitting facemask and if the risk to the rescuer is low, provide mouth-to-nose breaths, but if the risk is high or uncertain, perform chest compressions only.
Additionally, the guidelines have highlighted the difficulty of intubation in brachycephalic breeds and have advised to begin compressions in lateral recumbency until intubation is achieved. Once the airway is secured, reposition to dorsal recumbency (Yagi, 2025).
End tidal CO2 (ETCO2) monitoring. While previously encouraged, ETCO2 now plays a more vital role in guiding resuscitation to assess CPR quality. The updated guidelines have now set the target of 18mmHg during chest compressions as opposed to 15mmHg (Burkitt-Creedon et al, 2024). Higher values are associated with better perfusion, increased chances of ROSC and improves neurologic outcomes. While ETCO2 targets can differ between species, the key goal is to maximise ETCO2 levels for each individual patient.
Drug considerations and doses
Updated approaches to managing refractory shockable rhythms. Refractory shockable rhythm refers to any shockable rhythm – such as ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) – that persists after the first defibrillation attempt and remains shockable at the next rhythm check (Burkitt-Creedon et al, 2024). Under the 2012 recommendations defibrillation typically followed administration of drugs such as epinephrine in patients with shockable rhythms.
The 2024 guidelines now advocate delivering defibrillation before administering medications in cases of VF or PEA. This adjustment reflects a shift toward electrical intervention as a first-line treatment in rhythm disturbances where it is appropriate (Hopper et al, 2012; Burkitt-Creedon et al, 2024).
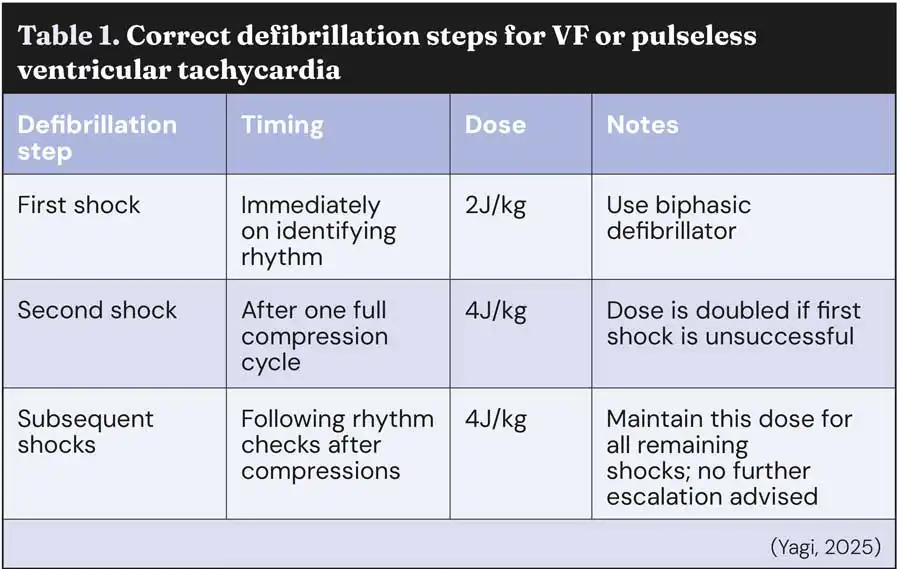
For VF or pulseless ventricular tachycardia, Table 1 discusses the correct defibrillation steps.
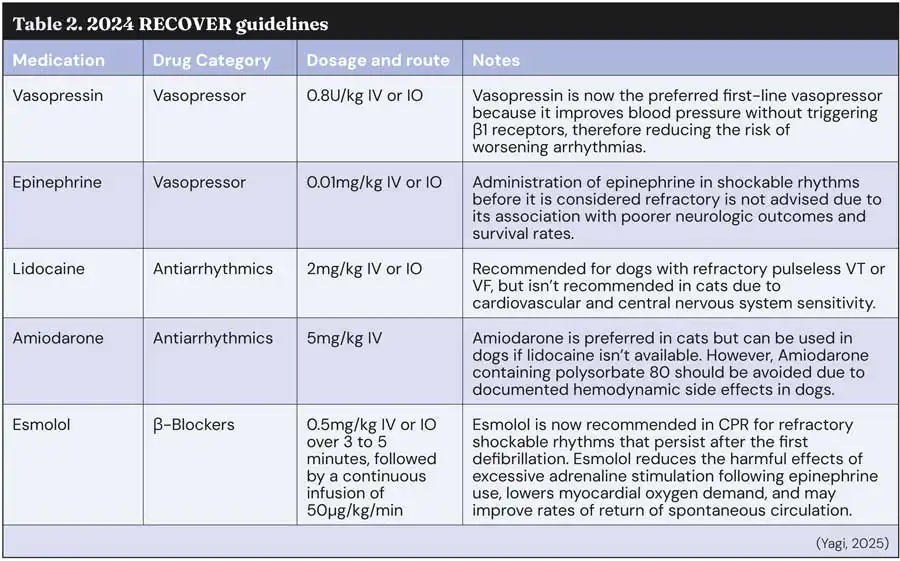
In addition to defibrillation protocol updates, the 2024 RECOVER guidelines provide recommendations for appropriate drugs and their doses in the event of refractory shockable rhythms. They are listed in Table 2.
The sheer amount of information and updates to the RECOVER guidelines may overwhelm and confuse some staff members and in the event of an emergency, visual aids and guidelines may be beneficial to utilise and display around the practice, so they are easily accessible and clear to understand.
Furthermore, regular training should be conducted and ideally a staff meeting should be held to discuss these crucial updates.
Effective CPR relies on every team member clearly communicating, understanding and executing their assigned role. Key roles during CPR are discussed in Table 3 and understanding each role and rehearsing/practising them regularly through simulation training ensures smooth transitions during real emergencies.
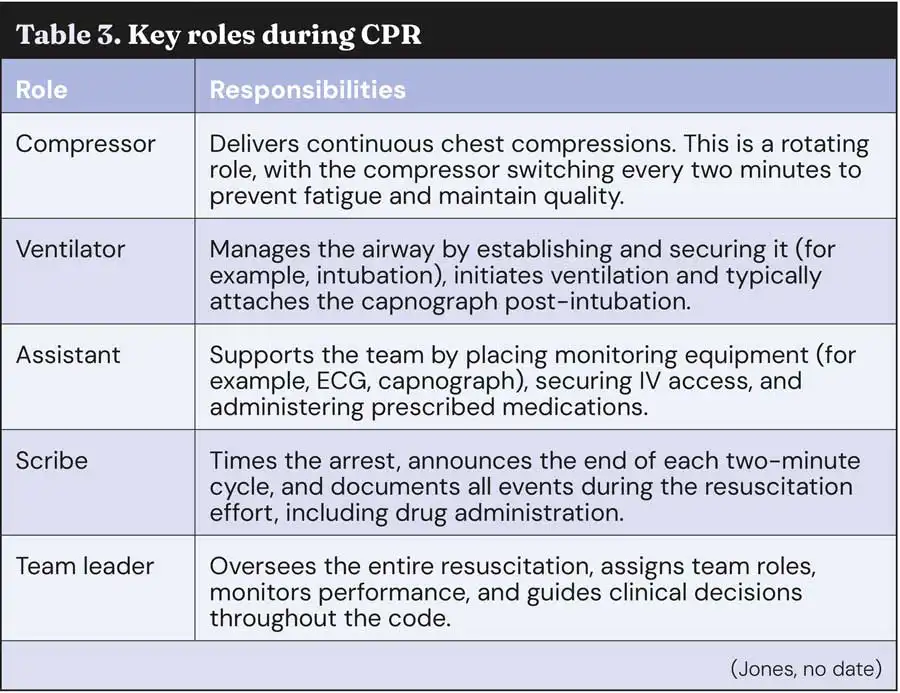
Leadership is one of the most influential factors affecting CPR team performance. An effective leader must demonstrate effective delegation, observation and time management skills (Hallam and Howarth, 2024).
Veterinary nurse-led CPR should be encouraged, as in many cases, it is veterinary nurses who first recognise CPA and initiate CPR. They should be empowered to lead or coordinate CPR if they are the first or most-experienced responder present.
Clear communication, quick decision-making and familiarity with the RECOVER guidelines can make the difference between confusion and control in an emergency.
In human medicine, evidence suggests that when nurses take the lead in BLS as opposed to a doctor, it allows the doctor to concentrate on advanced life support (ALS) and overall case management (Hallam and Howarth, 2024).
RECOVER recommends closed-loop communication during emergencies as it minimises errors. This type of communication consists of the sender giving a clear instruction, for example, “Administer 0.04 mg/kg of atropine IV”.
The receiver repeats the instruction back to confirm they heard and understood correctly, for example, “Administering 0.04 mg/kg of atropine IV”. And the sender confirms the repeated message, for example, “Correct”. Closed-loop communication reduces misunderstandings, limits background noise, and speeds up task execution (Hallam and Howarth, 2024).
Debriefing is an essential component of effective CPR and after every resuscitation attempt, the team should take time to review the case. This provides an opportunity to identify what went well, what could be improved and what changes could enhance future performance.
Debriefs are not to blame anyone for any errors, issues or areas for improvement, but to identify these and create a plan to manage them (Jones, no date).
Debriefs also support team well-being by providing space to process emotionally intense events, particularly when a case does not result in a positive outcome.
When debriefing becomes routine, it creates a safe environment to learn and reflect, and this is what strengthens the entire team and results in better patient outcomes.
One study of human CPA patients concluded that 52% of patients survived CPA once debriefing had been incorporated into clinical protocol in comparison to 33% before the intervention (Wolfe et al, 2014).
Effective CPR in veterinary practice relies on more than speed – it requires preparation, teamwork and clear communication.
The 2024 RECOVER updates refine both basic and advanced life support, offering clearer protocols, safer drug use and improved outcomes.
Veterinary nurses play a crucial role, often leading resuscitation efforts and ensuring team coordination.
Clear role delegation, closed-loop communication and regular training improve team performance during emergencies.
Debriefing after each case enhances learning, supports well-being and builds a stronger, more resilient team.