26 Apr 2010
Common bacterial skin infections in dogs: recognition and treatment
Jane Coatesworth examines commonly presented skin conditions, highlighting the hot spots where infection can multiply, and an approach to effective treatment.
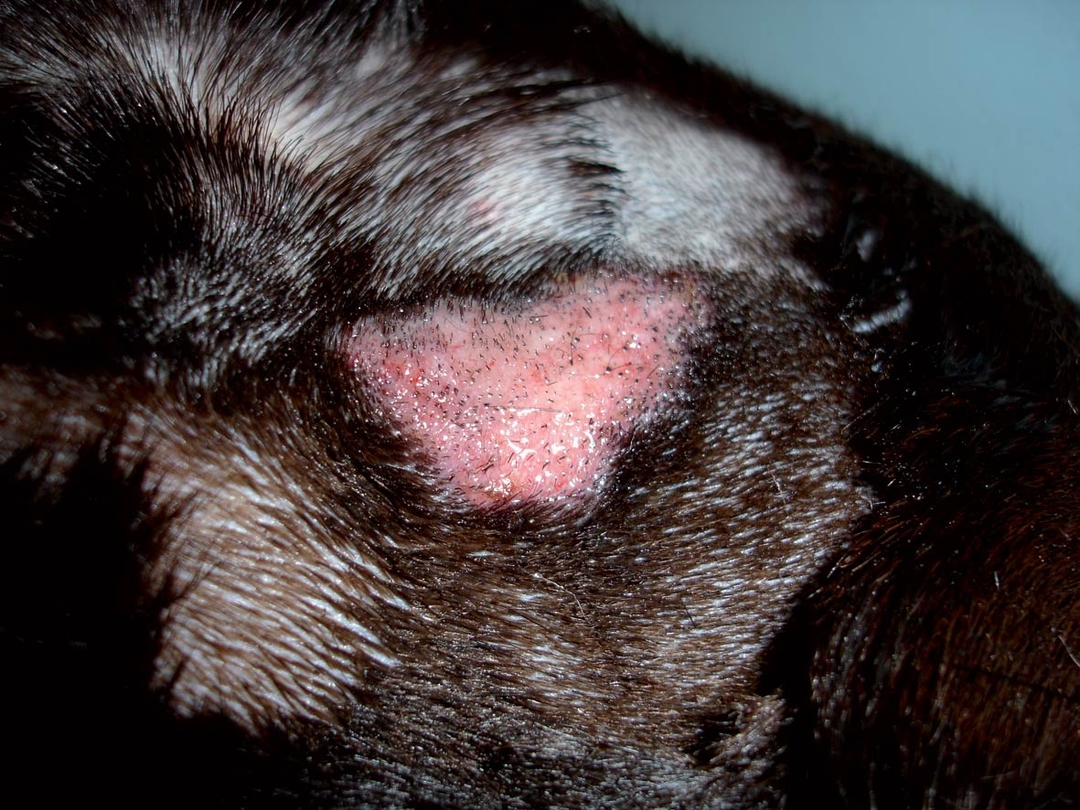
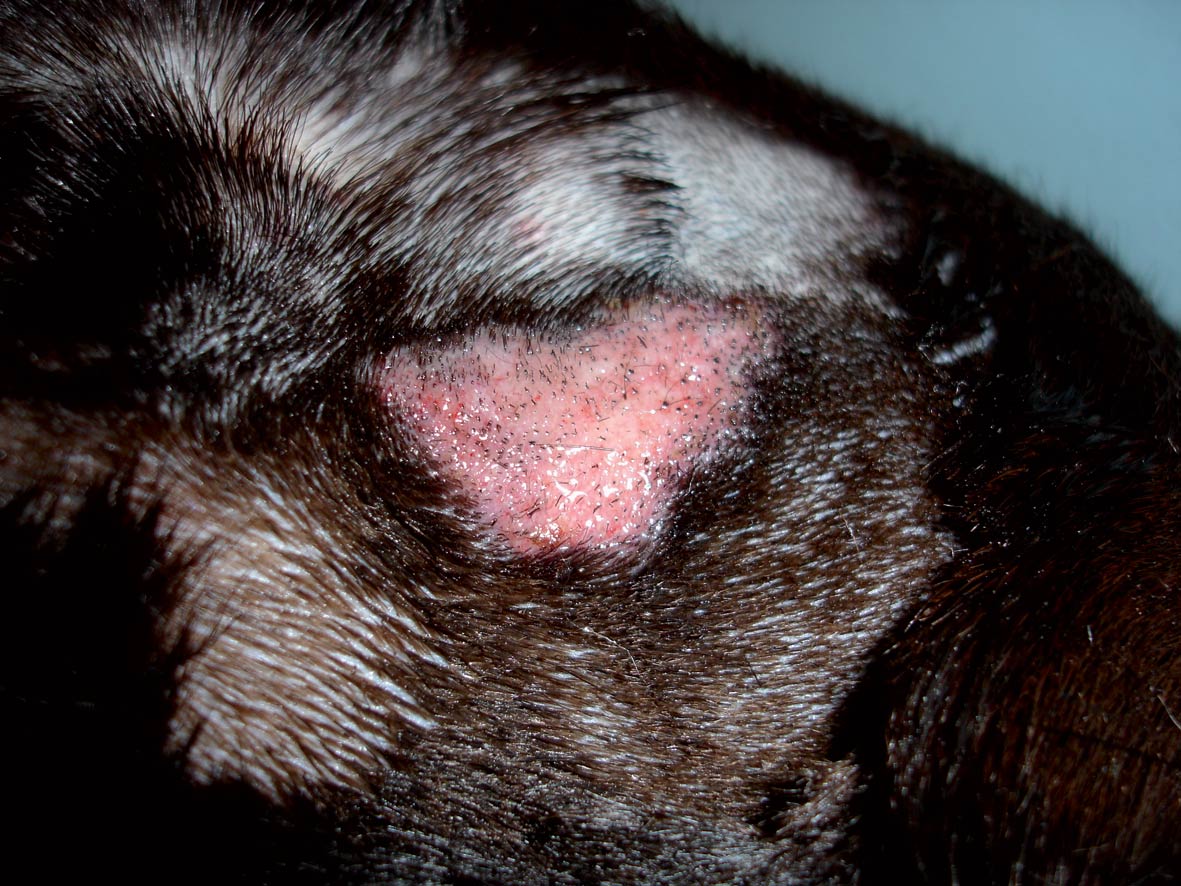
Figure 2. Same Labrador as in Figure 1 after clipping. Well demarcated exudative and erythematous lesion.
- This article is more than 15 years old. For a more up-to-date article on pruritus, check out this one from the Vet Times archive – An itchy dog – diagnostics and importance of cytology
Bacteria that cause skin infection may come from the environment – for example, Pseudomonas or mycobacteria from other animals – or from an individual’s own microflora.
The skin of a healthy dog is home to many thousands of bacteria. Micrococci and gramnegative staphylococci are common skin commensals. They live in balance with the host skin defences, and maintain populations in niches on the skin, where temperature, humidity and available nutrients are favourable.
A newborn puppy will start to encounter bacteria when the bitch bites open the amniotic sac and licks the puppy’s skin. Staphylococcus intermedius (now recognised as Staphylococcus pseudintermedius) is a common commensal of the nose, lips, anus, conjunctiva and vulva.
Away from these mucosal sites it seems to be found only in low numbers and with sporadic incidence on the healthy skin surface. Recall a warm heap of sleeping puppies, or a suckling bitch with pups crawling about the floor and climbing over her and one another – the bitch will transfer her commensals through contact, suckling and washing. Pups will also share microflora among themselves and with their environment, including people with whom they are in regular close contact.
Infection factors
A healthy balance of commensal bacteria has a protective effect against potentially pathogenic invaders. Established commensal bacteria physically occupy favourable skin niches and can produce a range of antibacterial substances to deter competing invaders – for example, locally active inhibitory or toxic factors. Potentially pathogenic bacteria, such as S pseudintermedius, require the ability to stay on the skin, to establish themselves, and to circumvent the host immune system, if they are to cause infection. Such abilities are called virulence factors. S pseudintermedius is the most common isolate from bacterial skin infections.
A range of factors determine the likelihood of developing a bacterial skin infection. A nonpruritic beagle in a clean laboratory environment is likely to have a much lower bacterial skin population than a pruritic dog in a dirty kennel environment, especially if the temperature and humidity in the kennel area is high. Licking, chewing and nibbling of the body transfers staphylococci from mucosal carriage sites on to inflamed skin.
The normal skin surface is a challenging environment for bacteria to survive and multiply. Corneocytes, the tough nonnucleated outer skin cells, are continuously exfoliated from the skin surface as the epidermis reproduces itself with new cells from the basal layer. Bacteria will be shed with the skin cells into the environment. Corneocytes are embedded in a mixture of intercellular lipids, forming a “bricks and mortar” pattern. The lipid emulsion helps to resist bacterial penetration of the epidermis. Staphylococci are known to adhere more to the corneocytes of atopic dogs than to those of normal individuals, thereby raising the carriage potential, and weight of bacterial challenge.
Dogs with atopic dermatitis also have abnormal intercellular lipid profiles, resulting in poor skin barrier function. These factors may contribute to a relatively high incidence of bacterial skin infections, compared to normal dogs.
Recognising infection
Bacterial skin infections can look very different from each other, depending on infection depth.
Surface infections
These only involve the outermost layer of the skin – the stratum corneum. They are often triggered by scratching or biting at a focal itchy area, abrading the skin and allowing rapid proliferation of bacteria (Figure 1).
Hot spots are usually intensely pruritic and erythematous, with a copious exudate that mats the overlying or surrounding fur. The full extent of the lesion may only be apparent after clipping and cleaning to remove the matted hair and encrusted exudate (Figure 2).
Hot spots are also known as acute moist dermatitis or pyotraumatic dermatitis. Breeds with a dense coat are predisposed – for example, Newfoundlands, huskies and golden retrievers.
The skin surface does not look or feel raised or thickened, but it may be eroded. The lesion has a clear demarcation from adjacent healthy skin. The location of a hot spot can indicate the original cause of the pruritus. For example, a lesion on the lateral face may indicate a sore ear on that side, and a lesion on the rump may suggest flea infestation or anal gland irritation.
Skin fold infection, or intertrigo, occurs when haired skin rubs on an adjacent area of haired skin, creating abrasion and an area of relatively high temperature and humidity. Certain breeds have specific skin fold problems, created by their unique conformation. Nasal folds are seen in short-nosed breeds, such as pugs and Boston terriers. Bulldogs with tight screw tails may have tail folds, and the excess skin of Shar Peis and basset hounds can create folds at the hocks.
Mucocutaneous pyoderma most commonly presents as erythema, swelling, fissuring, crusting and erosion of the lips. Occasionally, the anus, prepuce, vulva, nares or periocular skin is affected. German shepherd dogs are predisposed, and the pathogenesis is poorly understood.
Superficial infections
These involve the epidermis between the hair follicles (intertrigo) or the hair follicles themselves (bacterial folliculitis). The latter is the most common form of bacterial skin infection in the dog (Figure 3).

Superficial infections start as small red bumps on the skin (papules), and progress to pustules. The thin epidermis of the dog makes the pustule a readily ruptured and short-lived stage. Follicular pustules may have a central hair protruding, while the pustules of intertrigo occur between the hair follicles. It is important to remember that pustules are not always bacterial, such as the sterile pustules of pemphigus foliaceus. The content of a ruptured pustule will dry to a crust, while the pustular wall will peel back in a ring to form an epidermal collarette (Figure 4).

Collarettes frequently have dark-coloured centres of postinflammatory hyperpigmentation. Circular patches of darker coloured skin (hyperpigmented macules) can be seen at the former site of a bacterial skin infection after the collarettes have resolved.
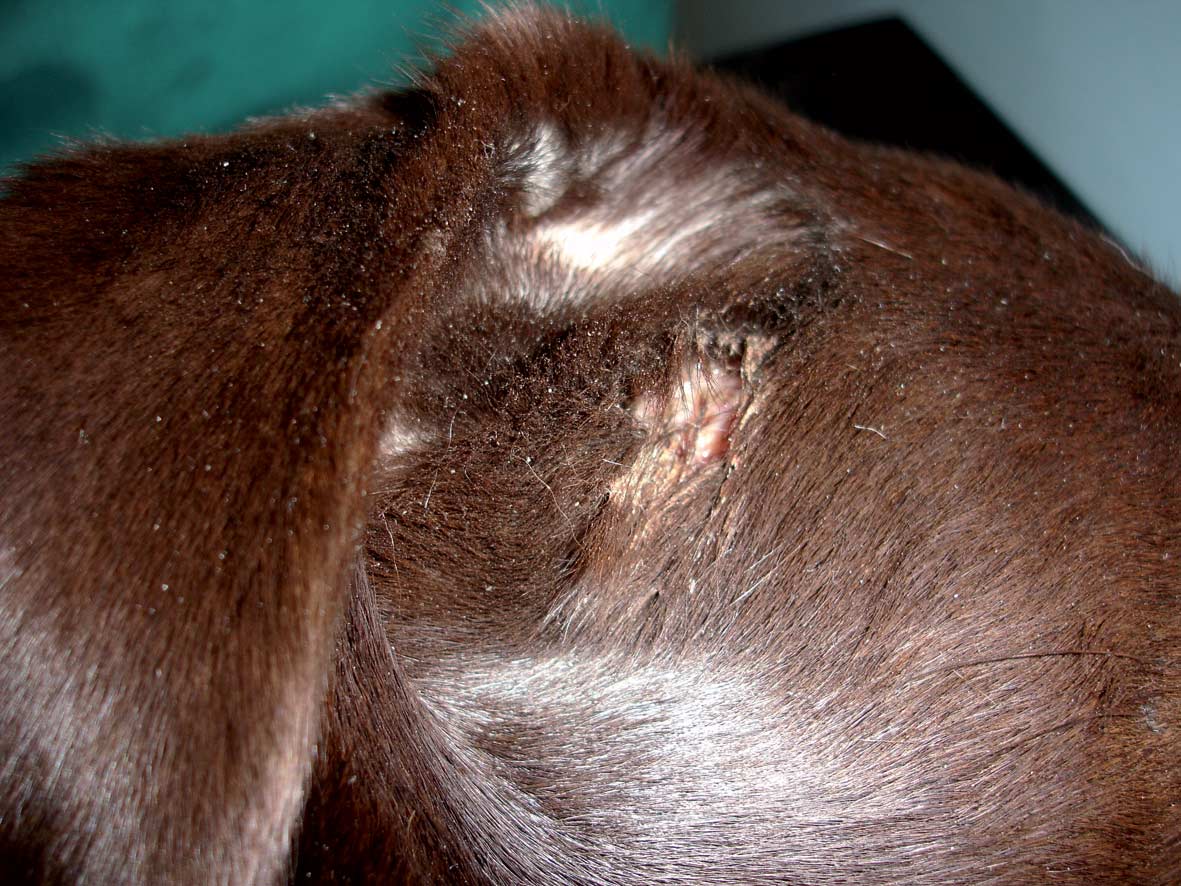
• Deep infections penetrate the epidermis, often through rupture of infected hair follicles, and are active in the dermis. The skin may initially show pink to purple papules or haemorrhagic bullae. These often rupture and discharge purulent to haemorrhagic fluid on to the skin surface from sinuses and fistulae (Figures 5 and 6). The fluid may dry, and matt overlying hair to form a crust. Ulceration is also common. The inflammation and fibrosis creates palpably thickened areas and plaques.


Deep pyodermas can be localised or generalised. Localised cases can result from foreign body penetration, focal trauma or bite wounds where environmental, oral or host-commensal bacteria are implanted into the dermis. Localised or generalised cases can be seen with patients receiving immunosuppressive medication, and in cases of demodicosis, and immunocompromising endocrinopathies, such as hyperadrenocorticism and hypothyroidism.
Treatment
Surface pyodermas
These respond well to topical treatment. Clipping and gentle cleaning of the area allows the lesion to be clearly assessed, reduces the local temperature and humidity, and allows treatment to more easily reach the skin. The patient may need sedation or anaesthesia to do this thoroughly, without distress. Antibacterial agents like fucidin, or astringents such as Hamamelis (witch hazel), can be applied in a gel or spray form; topical glucocorticoids can be used, short term, to reduce pruritus. It is important to identify and treat the underlying cause associated with hot spots, such as otitis externa or impacted anal sacs, and to palpate the skin around the hot spot, as some can be circled by foci of deeper infection, which require systemic antibiotics.
Skin folds benefit from regular cleaning to prevent the accumulation of bacteria, yeasts, exudates and debris. Antibacterial wipes and cotton buds are useful and convenient tools. Medical management is likely to be life-long, so owner commitment and motivation is essential. Touching a glass slide on to the skin surface, drying it, staining with Diff-Quik and looking under oil immersion down the microscope, can differentiate bacterial, Malassezia and mixed infections. Overweight animals will benefit from bodyweight reduction and the investigation of possible related problems, such as hypothyroidism or degenerative joint disease.
Excessive tear production, as identified by Schirmer teat testing, can lead to macerated skin within a wet facial fold and subsequent overpopulation by opportunistic micro-organisms. Epiphora has a range of underlying causes, including entropion and distichiasis. Surgery can be a definitive solution to skin-fold problems, for example removing lip folds in affected spaniels, but requires good surgical judgement and technique.
Superficial infections respond well to the correct antibiotic given for an appropriate length of time. Infections that fail to respond to logical therapy should be swabbed promptly for bacterial culture and sensitivity as they may be methicillinresistant strains of S aureus or S pseudintermedius.
Clindamycin is the antibiotic of choice for initial episodes of superficial pyoderma. It is narrow spectrum, fast acting, has good penetration and can be given once daily. Unfortunately, inducible resistance can rapidly occur, so repeated episodes should be treated with cephalexin or potentiated amoxycillin.
Potentiated sulphonamides are effective and inexpensive, but have potential adverse reactions of keratoconjunctivitis sicca, arthropathies and depressed T4 values. Antibiotics should be given for one week beyond apparent clinical cure – requiring a total course of three weeks. Glucocorticoids are not indicated in the treatment of superficial infections. Chronic relapsing cases of mucocutaneous pyoderma can be managed with the regular topical application of antibacterial gel or cream to the affected skin.
Antibacterial bathing can help reduce the incidence of recurrent pyoderma. Active ingredients of antibacterial shampoos include chlorhexidine, ethyl lactate and benzoyl peroxide. Recurrent pyoderma suggests a persistent underlying cause, requiring further investigation and specific treatment. Conditions commonly associated with recurrent pyoderma include demodicosis (Figure 7), atopic dermatitis, hyperadrenocorticism and hypothyroidism.

Deep pyoderma
This can involve a range of bacteria with unpredictable antibiotic sensitivities. Treatment should be based on tissue culture and sensitivity testing. Full-thickness biopsy samples are obtained using clipping, cleaning and strict aseptic technique to avoid confusing contamination from surface commensal bacteria. The tissue samples can be rolled in a moist sterile swab, and submitted to the laboratory in a sterile container, such as a universal bottle. Antibiotics are often required for many weeks, and should be given for two weeks beyond clinical cure. Gentle clipping and bathing of affected skin reduces crust formation and keep sinuses patent. Patients with deep pyoderma can be very sick and require careful monitoring to ensure full recovery, as well as timely treatment of their underlying disease. Glucocorticoids should be avoided in any form. Analgesia with NSAIDs or opiates may be beneficial in the early phases of treatment, as deep pyoderma tends to be painful rather than pruritic.
Summary
Bacterial skin disease is common. Recognition of the depth of infection is useful to guide the type and duration of treatment. Infection is secondary, therefore, diagnosis and treatment of the underlying cause is as important as diagnosis and treatment of the infection.
Glucocorticoids are only helpful in surface infections. Clindamycin is the antibiotic of choice for first-occurrence superficial infections. Persistent infection, despite the logical treatment of superficial infection, should trigger swabbing for bacterial culture and sensitivity.
- For a more up-to-date article on pruritus, check out this one from the Vet Times archive – An itchy dog – diagnostics and importance of cytology
