14 Nov 2022
Common poisons in dogs
Nicola Bates describes clinical signs and management options for treating poisoning from household substances.

Image © Elles Rijsdijk / Adobe Stock
Dogs have access to a huge number of potentially toxic substances, including drugs, plants, pesticides and household products. But the most common substances involved in canine poisoning are those readily accessible around the home, such as ibuprofen, anticoagulant rodenticides, chocolate, grapes, and dried fruit and xylitol.
The clinical signs and management of poisoning with these substances is outlined in this article, but advice for a specific case can be obtained from a poisons information service, if required.
Ibuprofen
Ibuprofen is a readily available NSAID used in human medicine (Figure 1). Dogs are particularly sensitive to ibuprofen, and can develop severe gastric ulceration and intestinal irritation. Ibuprofen competitively inhibits the production of prostaglandins and this accounts for the major effects seen in ibuprofen toxicosis.
Vomiting can occur after 25mg/kg of ibuprofen in dogs (Dunayer, 2004) with gastrointestinal ulceration after doses of less than 50mg/kg (Poortinga and Hungerford, 1998). Acute renal failure has been reported at doses of greater than or equal to 175mg/kg (Villar et al, 1998; Dunayer, 2004), but can occur at lower doses. Severe neurological signs and death can occur at greater than or equal to 400mg/kg to 500mg/kg (Villar et al, 1998). Very large overdoses can be survived with prompt, aggressive treatment.

Clinical signs
Initial signs after ingestion of ibuprofen are vomiting, haematemesis, diarrhoea, melaena and abdominal tenderness. Ingestion of a large dose (more than 400mg/kg) may result in rapid onset neurological signs with agitation, tremors, twitching, seizures and coma; dyspnoea, tachycardia, vocalisation and metabolic acidosis can also occur. Death can occur within a few hours of ingestion after a large dose, but fatal cases are uncommon.
As signs progress, protracted vomiting, pyrexia, anaemia, anorexia, polyuria, polydipsia, dehydration and collapse may also occur. Gastric erosion, ulceration and perforation may occur, sometimes in the absence of any major clinical effects. Dark, tarry stools may be observed in animals with gastric ulceration.
Hypotensive or dehydrated animals are more at risk from renal effects, as are those with pre-existing renal impairment.
Signs of liver damage (raised liver enzymes, bleeding, jaundice) are uncommon, but can occur in severe cases (Bolfer et al, 2014), generally within 24 to 48 hours of ingestion.
Management
Treatment is aimed at preventing or treating gastrointestinal and renal signs. After a large dose, treatment may also be required for neurological signs.
An emetic and activated charcoal can be given if ingestion was recent, but if vomiting has already occurred, an antiemetic and activated charcoal should be given.
In severe cases where the dose ingestion is large, administration of IV lipid emulsion should be considered. This should be given as soon as possible and may reduce the severity of neurological effects, which can be rapid in onset. It will not prevent the renal, gastrointestinal or hepatic effects, and monitoring and treatment for these will still be required over the following days (Bolfer et al, 2014).
Therapeutic plasma exchange has also been used in dogs with ibuprofen toxicosis (Walton et al, 2017). It would only be warranted in life‑threatening cases.
Gastroprotectants are advised following ibuprofen ingestion and should be given for 7 to 14 days, or longer depending on clinical condition and the dose ingested (Poppenga and Gwaltney-Brant, 2011).
A proton pump inhibitor (such as omeprazole twice daily) and misoprostol are recommended. Sucralfate is only recommended if ulceration is suspected or confirmed.
If severe or persistent vomiting occurs, then antiemetics should be administered as vomiting may result in dehydration and subsequent renal impairment. Renal function should be monitored at 24 and 48 hours post‑ingestion (Tegzes, 2016), although renal failure may occasionally be delayed for up to five days post-ingestion.
If possible, blood gases and electrolytes should be checked and corrected – especially if evidence is present of renal dysfunction and/or oliguria.
Routine monitoring of liver function is not required, except after ingestion of a significant quantity. Acetylcysteine and S-adenosyl methionine have been used for ibuprofen‑induced liver damage (Bolfer et al, 2014).
Anticoagulant rodenticides
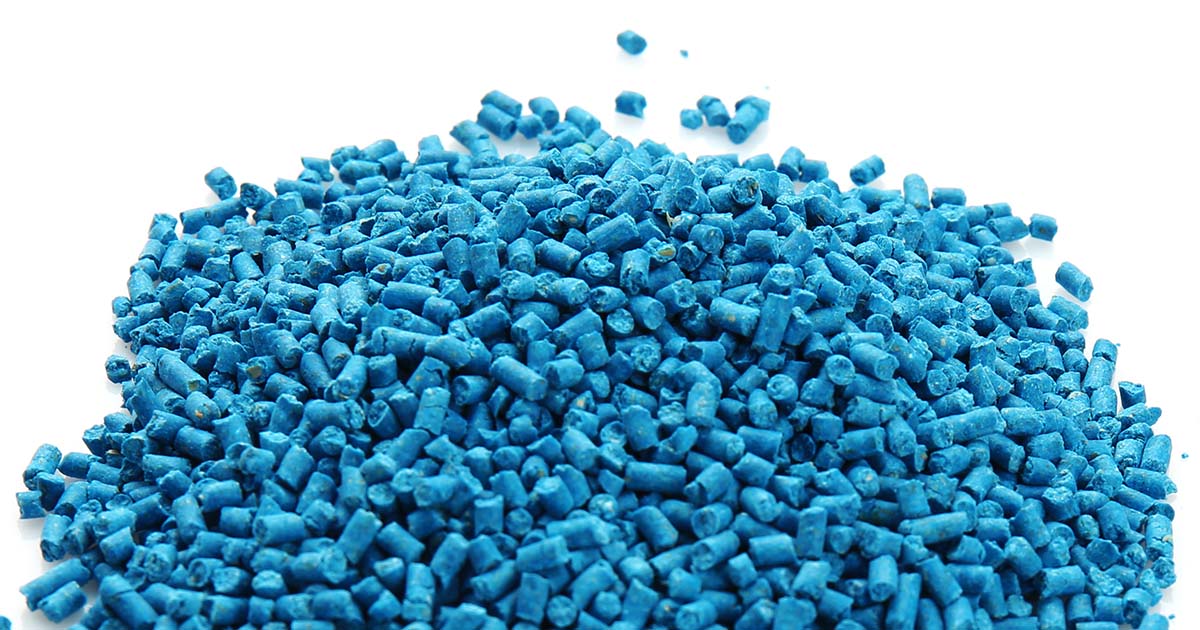
Ingestion of anticoagulant rodenticides is very common in dogs. The products are left out for the control of rats and mice, but are often readily accessible to pets in the form of ready-to-use baits in blocks, gels, grain, pasta baits or pre-baited boxes. Products are often dyed and coloured faeces may be the first indication that the bait has been ingested.
Vitamin K1 is a cofactor in the activation of clotting factors II (prothrombin), VII, IX and X. Anticoagulant rodenticides inhibit the enzymes involved in the conversion of inactive vitamin K1 epoxide to active vitamin K1, resulting in the gradual depletion of the body stores of vitamin K1. Once vitamin K1 and the clotting factors have been depleted, signs of bleeding occur; hence, a time lag between acute ingestion and onset of signs occurs.
The acute toxic doses of the anticoagulant rodenticides are variable and usually based on one-tenth of the LD50 value (Murphy and Talcott, 2013). Chronic ingestion is more hazardous than acute ingestion. In an experimental study, dogs could tolerate 10mg/kg of bromadiolone in a single dose and repeated doses of 0.005mg/kg to 0.01mg/kg for several days, but 0.015mg/kg/day caused haemorrhagic diarrhoea; 0.1mg/kg/day resulted in death after 5 to 22 days (Grand, 1976).
Clinical signs
Clinical effects of anticoagulant rodenticide toxicosis are typically seen within three to five days of exposure, but may be delayed for up to seven days (DeClementi and Sobczak, 2012), but clotting parameters become prolonged before the onset of clinical signs.
The prothrombin time (PT) is the first test to become prolonged and the first to return to normal. Prolongation of the PT occurs from 36 to 72 hours, and after 72 hours, the activated partial thromboplastin and activated clotting time become prolonged (DeClementi and Sobczak, 2012).
Clinical signs are due to coagulopathy and any type of bleeding may occur. The initial signs may be non-specific with lethargy, weakness, cough and pale mucous membranes. Haemorrhage into the lungs is common (Schulman et al, 1986; Lewis et al, 1997), and can manifest as haemoptysis, epistaxis, dyspnoea and exercise intolerance.
Joint haemorrhage can manifest as lameness. Acute upper airway obstruction due to laryngeal, tracheal or thymic haemorrhage is possible. Gastrointestinal haemorrhage manifests as abdominal tenderness, haematemesis and melaena.
Management
Treatment is recommended for acute ingestion of a toxic dose with emesis and activated charcoal. Ingestion of a single dead rat or mouse will not cause poisoning, as the residue of anticoagulant in a dead rodent is very low. If the dog has suspected bleeding, it is too late for gut decontamination and is potentially hazardous.
In asymptomatic animals, vitamin K1 for at least 21 days followed by assessment of the PT at least 48 hours after the final dose should be started if a toxic dose has been ingested.
If any doubt exists about the amount ingested, or chronic exposure is suspected, then a course of vitamin K1 should be given. If the decision is made not to treat with vitamin K1, the PT can be checked 48 to 72 hours post‑ingestion to rule out the risk of bleeding.
If any delay occurs in obtaining results of PT measurement and concern exists about risk of bleeding, then vitamin K1 therapy could be started after bloods are taken until the results have been obtained and confirmed as normal.
Owners should be advised to monitor for any evidence of bleeding over the next few days and advised to return immediately if bleeding is suspected. It is also recommended that steps are taken to prevent further exposure.
If the dog is already bleeding, vitamin K1 should be given immediately. Animals with significant bleeding should be admitted for at least 24 hours in the first instance (Murphy and Talcott, 2013), and handled with care to avoid unnecessary stress and risk of haemorrhage.
Management of animals with active bleeding is aimed at replacing inactive clotting factors and providing vitamin K1 to allow the liver to synthesise its own clotting factors.
It is frequently stated that although vitamin K1 is immediately available to the body, it can be hours before it has an effect. In a recent study, however, in four dogs with anticoagulant rodenticide toxicosis, IV vitamin K1 corrected the PT one hour after dosing (Mooney et al, 2020). In another study, a marked improvement was recorded in the PT of 43 dogs with anticoagulant rodenticide toxicosis when tested at four hours after IV dosing (Senzolo et al, 2014).
Vitamin K1 therapy must be maintained for as long as the anticoagulant is in the body. In most cases, therapy is required for three weeks or more – due to the long half-life of these compounds – and it is essential to complete the full course.
Clotting parameters should be measured 48 to 72 hours after the final dose of vitamin K1 to check they have returned to – and remain – normal. If necessary, vitamin K1 can be given for another week and the clotting parameters rechecked.
Chocolate
Chocolate ingestion (Figure 2) is very common – particularly around Christmas and Easter (Noble et al, 2017). The main toxic component of chocolate is theobromine – a methylxanthine – but it also contains a small amount of caffeine (another methylxanthine).
The amount of theobromine in milk chocolate can vary from 1mg/g to 2.1mg/g (Bates et al, 2015). Dark chocolate can contain about four times the quantity of theobromine compared to milk chocolate, whereas the amount in white chocolate is minimal. Some chocolate products – particularly those for diabetics – can contain xylitol and chocolate-coated raisins pose a double hazard.
Methylxanthine intoxication produces CNS stimulation with cardiac and respiratory hyperactivity. Data suggests that toxic effects in dogs occur at theobromine doses of 20mg/kg, with severe signs at 40mg/kg to 50mg/kg and seizures at 60mg/kg (Gwaltney-Brant, 2001). Fatal theobromine poisoning has been reported in dogs following ingestion of 80mg/kg to 300mg/kg (European Food Safety Authority, 2008).

Clinical signs
Signs of chocolate toxicity generally occur within 2 to 4 hours of ingestion (Dolder, 2013), but can sometimes occur after 6 to 12 hours (Gwaltney-Brant, 2001).
Initially, vomiting, abdominal discomfort, diarrhoea, polydipsia, polyuria and restlessness, excitability and hyperactivity may occur; this may be followed by ataxia, tremors, tachycardia, hypertension and hyperthermia. Convulsions after chocolate ingestion are rare.
Other less common effects include bradycardia, haematemesis, haematuria, bloat, tachypnoea, cyanosis and arrhythmias. Renal dysfunction is also uncommon. Pancreatitis may result 24 to 72 hours after ingestion because of the high fat content of some chocolate products (Gwaltney-Brant, 2001).
Recovery from theobromine toxicity can occur within 24 hours, but may take 48 to 72 hours.
Fatal chocolate poisoning is not common in dogs and is usually due to cardiac arrhythmias or, less commonly, respiratory failure.
Management
If a potentially toxic dose has been ingested (equivalent to more than 20mg/kg of theobromine), gut decontamination should be attempted. An emetic can be given, but is best avoided in animals with hyperactivity or excitability due to theobromine toxicity; however, activated charcoal can be given, if practical. Repeated doses of adsorbents may be useful in enhancing elimination as theobromine appears to undergo enterohepatic recirculation and has a long half-life. In symptomatic animals, the heart rate, body temperature and ECG should be monitored.
Treatment is supportive with antiemetics for severe or persistent vomiting, and fluids are recommended to support the cardiovascular system and enhance excretion (as theobromine is excreted renally). Diazepam or methocarbamol can be used for the management of tremors, with diazepam or barbiturates for hyperactivity or convulsions.
Where tachycardia is severe, a beta-blocker such as propranolol or metoprolol can be given. Lidocaine is the drug of choice for ventricular arrhythmias unresponsive to a beta-blocker.
Prognosis is good, but more guarded in dogs with seizures or arrhythmias (Dolder, 2013), and dogs with pre-existing cardiac disease may be more at risk of cardiac effects.
Grapes and their dried fruits
Grapes and their dried fruits (sultanas, raisins and currants; Figure 3) can cause acute kidney injury in dogs. The fatal dose of these fruits has not been established and a dose-response relationship does not appear to exist (Eubig et al, 2005). Individual variation in response may also occur, and some dogs have been reported to eat grapes and dried fruits without apparent adverse effects.
The lowest doses of grapes reported to result in renal failure is four or five grapes in one dog (Mazzaferro et al, 2004), and 2.8g/kg in another (Eubig et al, 2005). For raisins, the lowest dose to cause renal failure is 3g/kg (Morrow et al, 2005).
In a review of 49 cases, a higher proportion of dogs that ingested dried fruit (73.5 per cent) developed clinical signs compared to those that ingested grapes (26.5 per cent). Of the 17 fatal cases, 12 had ingested dried fruits and 5 had ingested grapes (Sutton et al, 2009).
The toxic dose of raisins, currants, sultanas or grapes has not been established, and a dose-response relationship does not appear to exist (Eubig et al, 2005). Individual variation in response may also occur, and some dogs have been reported to eat grapes and dried fruits without apparent adverse effects.
It has recently been suggested that tartaric acid in grapes is the cause of the acute kidney injury that occurs (Wegenast et al, 2021; 2022), but there is still much to learn about grape toxicosis in dogs.

Clinical signs
Clinical signs of poisoning usually occur within 6 hours and are always present within 24 hours. Initially, vomiting, diarrhoea, hypersalivation, haematemesis, bloody stools, anorexia, tender abdomen, ataxia, weakness and lethargy will be observable. Grapes or dried fruit may be present in the vomitus or faeces (Eubig et al, 2005).
From 24 to 72 hours, renal failure may develop with oliguria or anuria. Some animals appear dehydrated and may be polydipsic, and evidence of pancreatitis may be observable (Eubig et al, 2005). Bradycardia, tachycardia, hypothermia or hyperthermia, anaemia, leukocytosis, cyanosis, respiratory depression, tremor, rigidity and seizures have been reported in some cases. Fortunately, symptomatic acute kidney injury is rare in pets with grape or dried fruit ingestion (Reich et al, 2020; Dijkman et al, 2022).
Prognosis is good if treatment is started before the onset of renal signs, but prognosis is poor in dogs with oliguria or anuria after ingestion of grapes and grape products (Gwaltney-Brant et al, 2001).
Management
Gut decontamination should be considered following ingestion of any quantity of grapes, raisins, sultanas or currants (Mazzaferro et al, 2004). Digestion of grapes and dried fruit appears to be slow, and gastric decontamination several hours post‑ingestion is possibly worthwhile.
Aggressive IV fluid therapy (such as twice the normal maintenance rate) for at least 48 hours for rehydration and to support renal function is recommended to prevent acute kidney injury. An antiemetic should be given if vomiting is protracted. Where fluid therapy is declined by the owner, serial monitoring of renal function is recommended.
Electrolytes and renal function should be monitored every 24 hours for 72 hours and animals should be monitored for signs of fluid overload. Where necessary, use of furosemide or mannitol may be considered to re-establish urine output, but efficacy is unproven, and evidence exists that tubular necrosis and obstruction of the renal tubules occurs, preventing urine flow (Mazzaferro et al, 2004).
Dopamine may be used to enhance renal perfusion. Haemodialysis and peritoneal dialysis have been used in the management of grape toxicosis (Mazzaferro et al, 2004, Eubig et al, 2005, Stanley and Langston, 2008), although availability and cost may be an issue.
Xylitol
Xylitol is a naturally occurring sugar alcohol that is manufactured and used as a sweetener in foods and confectionery (it may be listed under its food additive code, E967); it is also an excipient in some medicines and is available in granular form for baking.
Xylitol is a potent stimulator of insulin release in dogs, causing a dose-dependent and rapid increase in insulin concentrations, resulting in a decrease in glucose concentrations. The mechanism of xylitol-induced liver damage is unknown.
Clinical signs
Effects from xylitol can be rapid in onset or may be several hours after ingestion in the case of chewing gum.
Clinical features of hypoglycaemia include vomiting, tachycardia, ataxia, coma, convulsions, hemiparesis, hypokalaemia, hypomagnesaemia and hypophosphataemia. With severe hypoglycaemia, metabolic acidosis, status epilepticus, cerebral oedema, hypotension, ventricular tachycardia and cardiovascular collapse may also be present.
Liver failure can occur in the absence of hypoglycaemia and signs occur nine to 72 hours post‑ingestion, with raised liver enzymes, bilirubin, prolonged clotting time, thrombocytopenia and hyperphosphataemia.
Management
Treatment is recommended in dogs for more than 0.05g/kg (50mg/kg) of xylitol with emesis and activated charcoal, depending on the clinical condition of the dog.
In many products, the quantity of xylitol is not declared on the packaging, but a poisons information service may have access to this information.
Baseline glucose, potassium, phosphorus, total bilirubin, liver enzymes and clotting parameters should be obtained. The blood glucose should be monitored every 1 to 2 hours for at least 12 hours.
Management of hypoglycaemia is supportive, and S-adenosyl-L-methionine can be used as hepatic protectant (Dunayer and Gwaltney-Brant, 2006).
- Some of the drugs discussed in this article are used under the cascade.
| Dosages of drugs mentioned in the text | |
|---|---|
| Drug | Dosage |
| Activated charcoal | 1g/kg to 3g/kg once or every four hours until present in the stools. |
| Misoprostol | 2µg/kg to 5µg/kg orally every 8 to 12 hours for three to five days. |
| Omeprazole | 0.5mg/kg to 1.5mg/kg IV or orally every 24 hours. |
| S-adenosyl methionine | 40mg/kg once then 20mg/kg once daily for seven days or more. |
| Acetylcysteine | IV: 140mg/kg diluted in 12ml/kg to 25ml/kg of fluid IV over 6 hours, followed immediately by another slow infusion of 70mg/kg IV (similarly diluted) every 6 hours for 36 hours or more dependent on the clinical condition of the animal. Continue treatment until dog is clinically well. Oral: can be given orally (same dose as IV), but should be diluted to improve palatability. |
| Vitamin K1 | In animals with active bleeding IV: 5mg/kg by slow IV injection, then switch to oral therapy. A second injection can be given 12 to 18 hours later if oral treatment is not immediately possible. Other animals or after IV dosing Oral: 5mg/kg once a day for 21 days with food. It is essential to complete the full course of vitamin K therapy. |
