9 Dec 2022
Cranioplasty for treating caudal occipital malformation syndrome
Shirley Simpson CertSAN, DipAVN (Surg), VPAC, AVLM, RVN, provides a comprehensive insight into – and a case study on – the treatment of this disorder, common in certain breeds, including a new technique created by Katia Marioni-Henry DipACVIM, PhD, DipECVN, SFHEA, MRCVS.

Figure 1. Depicting prominent compact skull.
The cavalier King Charles spaniel, Pomeranian, Chihuahua and griffon Bruxellois all have high, small skulls typical of brachycephalic breeds. MRI has shown that in these breeds, due to their under-sized skull, overcrowding of the brain and the cervical spinal cord occurs. The cerebellum is forced through the foramen magnum during development and this may lead to the progressive formation of cavities within the spinal cord called syringomyelia (SM).
SM is responsible for the majority of clinical signs. The clinical signs in dogs with Chiari-like malformation-syringomyelia, also known as caudal occipital malformation syndrome, are variable, but common among them are reluctance to exercise, pain, and an intermittent repetitive scratching action towards the shoulder, neck, or back of the head called “phantom scratching” (Nalborczyk et al, 2017). Chiari malformation (CM) is a congenital disorder with a delayed onset of clinical signs – typically between one and four years of age. The first documented case of CM was in the late 1990s (Rusbridge, 1997).
In this article, we will look at how a surgical technique used for the treatment of Chiari type-one malformation in humans was modified by veterinarians for our canine patients (Dewey et al, 2007). We will also show how our application of 3D printing has been employed to optimise this surgical procedure.
Chiari-like malformation-syringomyelia (CM-SM) is a common disorder in young, small breeds of dogs and is particularly prevalent in cavalier King Charles spaniels (CKCS) and their cross-breeds (Rusbridge, 2020). It is also frequently diagnosed in the King Charles spaniel, griffon Bruxellois, Chihuahua, Yorkshire terrier and Maltese, among others.
All these breeds typically are brachycephalic and have a retro-flexion (caudo-ventral tilting) of the facial part of the skull (Figure 1). In all the canine breeds with CM, the skull is considered too short to contact the brain and the cervical spinal cord; in the CKCS, it appears that the brain is also too big.

The result is a condition whereby the cerebellum is forced through the foramen magnum due to lack of space in the skull. This obstruction is thought to partially block the flow of CSF.
Most dogs afflicted with this condition have secondary syringomyelia (Rusbridge et al, 2003). Syringomyelia (SM) is when a cavity forms within the spinal cord. This cavity called a syrinx or syringomyelia, which can expand and elongate over time, pressing on the spinal cord. This pressure may result in paresthesia (a burning or prickling sensation), and/or pain affecting the back of the head, neck, shoulder and back, which provokes frequent scratching of these areas without making skin contact.
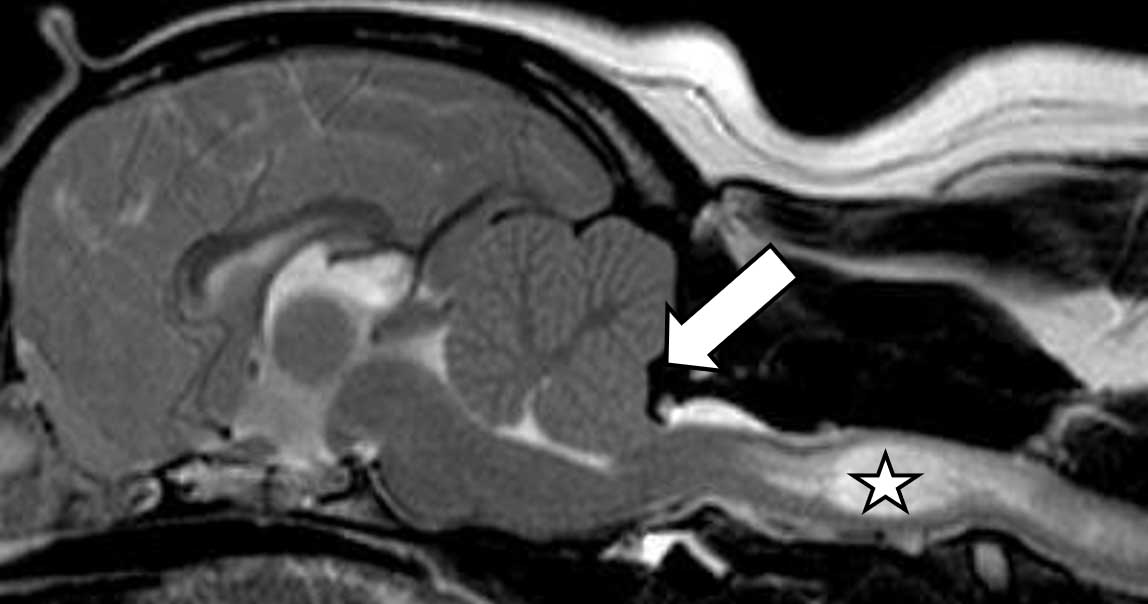
A diagnosis of CM-SM confirmed using MRI can be seen in Figure 2.
The canine CM-SM condition is similar to the Chiari malformation type-one in humans, originally described in the late 19th century by Hans Chiari, a Viennese pathologist. He described seemingly related abnormalities of the hindbrain, the so-called Chiari malformations, and patients with CM type-one describe neck pain, ataxia, muscle atrophy, limb numbness and debilitating headaches.
The surgical aim is to reduce pressure applied by the cerebellar vermis on the spinal cord at the foramen magnum. The preferred technique in human medicine for the treatment of CM is foramen magnum decompression (FMD). This surgery initially alleviates symptoms; however, 8% to 30% of human patients require reoperation due to the excessive scar formation (Sacco and Scott, 2003). The scar tissue leads to compression at the foramen magnum, mimicking the original disease state.
FMD performed for the treatment of canine CM-SM has similar success to human CM surgery and it is also reported to have a similar reoperation occurrence (Dewey et al, 2007). A cranioplasty technique originally developed in the US to treat human CM patients has been modified for dogs to help reduce the incidence of scar formation. This technique uses a moulded plate made of titanium mesh and polymethyl methacrylate (PMMA; Dewey et al, 2007).
We do not expect a complete resolution of clinical signs after surgery and the dimension of the chronic SM tends to remain the same. The main goal is to stop the progressive enlargement of the spinal cavity that leads to increased levels of pain and progressive neurological dysfunction (Dewey et al, 2007). In this paper, repeat MRI was performed in 10 (48%) dogs. Three dogs had no evidence of syringomyelia preoperatively, and had no such evidence on repeat MRI. Of the remaining seven dogs, the cervical spinal cord syrinx appeared subjectively unchanged on postoperative MRI.
Surgery preparation
At The University of Edinburgh, once diagnosis is confirmed, an exact 3D copy of the dog’s skull is printed by colleagues at the College of Art using CT images (Figure 3).
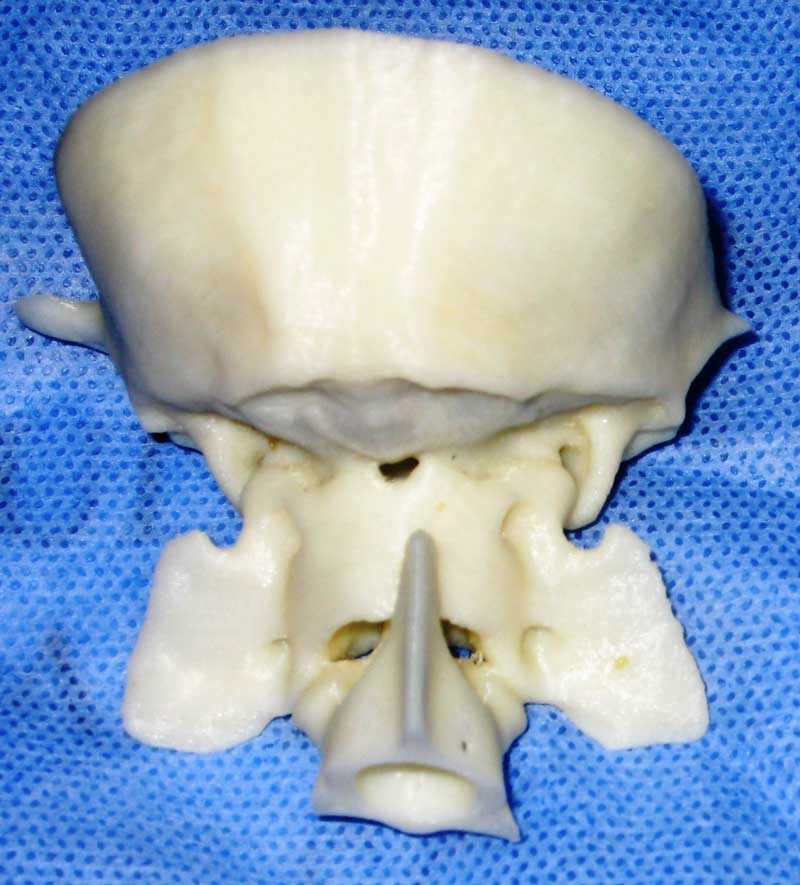
The 3D model is vital as it enables the surgeon to mould a piece of titanium mesh to the back of the model skull prior to surgery, thereby reducing anaesthesia and surgery time. The mesh is then sterilised in its moulded form with 2mm titanium screws in preparation for the operation.
For the procedure, theatre temperature should be maintained at 21°C. This is vital as diverse temperatures may affect the PMMA curing time.
Preoperative preparation
The clip should be proximal to the eyes and caudal to the thoracic vertebrae. The width of the clip should be slightly wider than the atlas (Figure 4).

Artificial tears should be administered bilaterally to prevent drying of the cornea or contact lenses should be placed for the duration of the surgical procedure.
As the surgery involves implants, preoperative and perioperative antibiotics are indicated. Cefuroxime 20mg/kg IV is administered 20 minutes prior to surgery and every 90 minutes thereafter until the end of surgery.
Mannitol (0.5mg/kg IV over 30 minutes) is administered perioperatively and prevents cerebral oedema.
The use of an armoured endotracheal tube to protect the airway in the flexed position can be considered, but is not always necessary.
Intraoperative warming is essential as the surgery is extensive. The use of warm air devices should be considered. The temperature of the patient needs to be monitored throughout the procedure.
Positioning
The positioning of the patient is critical for the surgeon. The dog must be straight on the operating table. The neck should be ventro-flexed over a rolled towel or vacuum support cushion. The rostrum should be taped to the table to prevent the flexed position relaxing during surgery (Figure 5).

Instrumentation
- Orthopaedic instrument pack (includes drill bits, drill guides and screwdrivers).
- Suction with Frazier suction tip.
- Incise drape.
- Monopolar and bipolar cautery.
- Spinal drill with a selection of long burrs.
- Pneumatic drill and hose.
- Kerrison laminectomy rongeurs (-2mm).
- Scalpel blade no 11 and no 10.
- Titanium mesh and titanium screws.
- PMMA.
- A stopwatch to time bone cement.
- Kidney dish and spatula.
- Sterile saline.
Surgery
An approach is made over the dorsal aspect of C1. For the FMD part of the surgical procedure, bone is removed proximal to the foramen magnum and below the occipital crest using a high-speed burr.
After creating the FMD defect, guide holes are drilled into the occipital bone around the periphery of the defect using a pneumatic drill. The patient’s head is then released from the ventro-flexed position and aligned with C2. The pre-moulded titanium mesh plate (Figure 6) is screwed on to the caudal aspect of the skull using 2mm titanium screws.
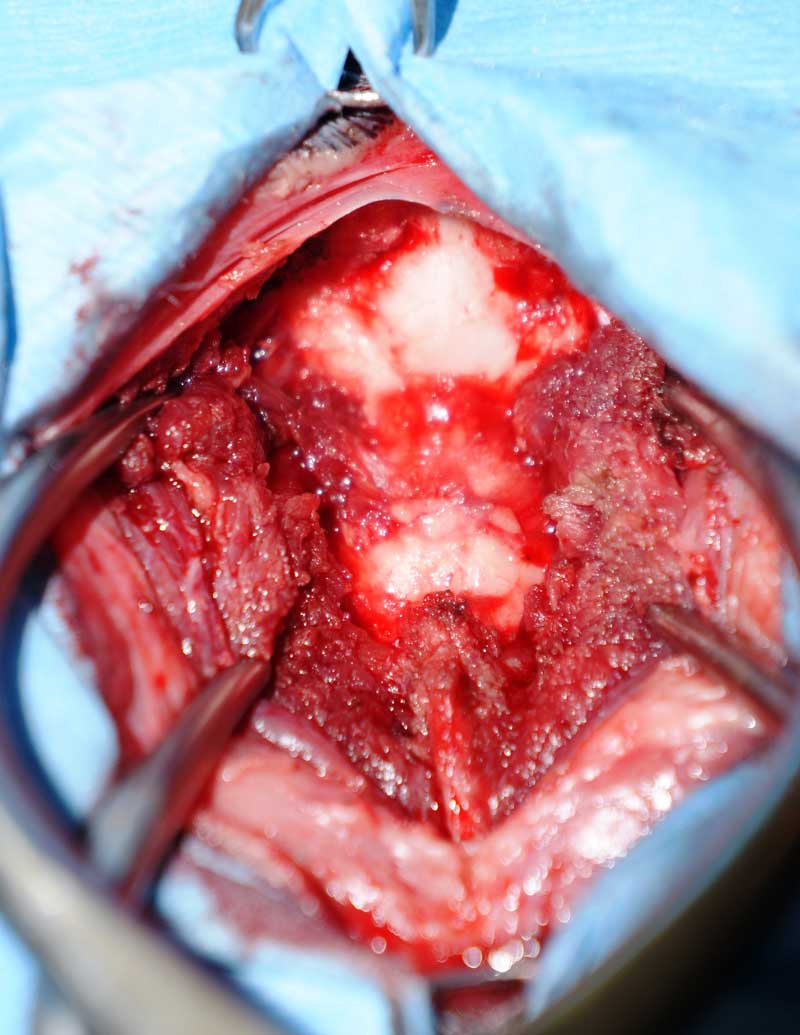
The mesh is covered with PMMA to prevent seeping of blood through the mesh and creation of a haematoma on the exposed cerebellar vermis, and to help secure the mesh to the skull. The caudal aspect of the plate extends over the dorsal defect of C1 – this protects the cerebellum.
A routine closure is performed. The incision should be covered with an adhesive film dressing to avoid contamination. Postoperative radiographs are taken immediately after surgery – these are recommended to assess the positioning of the mesh and screws.
The main aim of the surgery is to reduce the overcrowding at the cranio-cervical junction and prevent the progressive enlargement of the spinal cavity that leads to increased levels of pain and progressive neurological dysfunction (Dewey et al, 2007).
A four-year-old female neutered CKCS named Ruby (Figure 7) was presented with diffuse neck and back pain on palpation. She also demonstrated a left-sided head tilt and scratching of the right flank. The surgeon suspected SM secondary to Chiari-like formation.

An MRI was suggested to the owner to confirm this suspicion and rule out concurrent conditions such as intervertebral disc disease. MRI confirmed a Chiari–like malformation with severe and extensive asymmetrical SM. A CT scan of the skull and cervical vertebrae was performed to print a 3D model for surgical planning. The neurologist performed a FMD and cranioplasty.
Ruby made an excellent recovery from surgery and was discharged home four days after surgery. Her activity was restricted for four weeks after surgery. Two weeks after her surgery, she had a physical and neurological examination.
All vital parameters were within normal limits. Ruby had good movement of her head in all directions. She had a normal gait, postural reactions and cranial nerves function.
The neurologist found mild discomfort on palpation of the neck and abdomen. The spinal and abdominal discomfort was probably secondary to persistent SM.
It is not expected that the patient will have a sudden resolution of clinical signs, but it is expected that surgery should slow the progression of the condition.
Ruby continued receiving gabapentin for her SM, but she is still doing well, eight years after the diagnosis of severe SM and her surgery.
- Some of the drugs in this article are used under the cascade.
- This article was initially published in Vet Times without necessary due credit given at the time to Katia Marioni-Henry, European veterinary specialist in small animal neurology, who pointed out she created the new technique, including the use of 3D printing, and had supplied images and content for the article. We regret she was not correctly billed as a co-author at the time, and apologise to her and readers for any confusion this may have caused.
