3 Mar 2020
Marge Chandler concludes this article by discussing the nutritional management of a selection of disorders common in older pets.

Figure 1. Older dogs’ cognitive abilities may be helped by environmental enrichment as well as nutrition.
Part one of this article discussed the effects of ageing on the physiology and nutrient requirements of older dogs and cats.
As in humans, aged pets show great variability in age-related cognitive decline.
Prevalence estimates of cognitive dysfunction in dogs older than eight years of age have ranged from 14% to 60%, with prevalence increasing with increasing age (Fast et al, 2013; Roudebush et al, 2005).
For dogs 15 to 16 years old – and cats 15 to 21 years old – signs consistent with cognitive dysfunction syndrome (CDS) are 68% and 50%, respectively (Roudebush et al, 2005; Gunn-Moore et al, 2007).
Spatial learning and memory are affected by ageing. Aged dogs also show deficits in executive function and attention, and reduced learning ability and memory capacity.
Treatment with antioxidants has been suggested to reduce cognitive dysfunction by reducing the effects of free radicals. Many studies in humans have shown high intakes of fruits, vegetables, vitamins E and/or C, folate and/or vitamin B12 improve cognition, although studies also exist that fail to show improvement, and excessive intakes of antioxidants can – as noted in part one – paradoxically have a pro-oxidant effect.
The mitochondria are involved in numerous essential aspects of cell function – from energy production via the respiratory chain to steroid biosynthesis, pyrimidine biosynthesis, the tricarboxylic acid cycle, and apoptosis. They are also the main producers of reactive oxygen species within the cell and mitochondria‑mediated pathophysiology appears to be associated with ageing (Melov, 2004).
The addition of DL-alpha-lipoic acid and L-carnitine can enhance mitochondrial function, although lipoic acid used alone could have cognitive impairing effects (Milgram et al, 2007; Snigdha et al, 2016). Dogs supplemented with lipoic acid and carnitine had improved performance on the landmark task, the ability to locate the position of an object by reference to the position of an external referent or landmark.
These supplements may be effective in attenuating age-associated cognitive decline by slowing the rate of mitochondrial decay and cellular ageing (Milgram et al, 2007).
Note that DL-alpha-lipoic acid is toxic to cats.
Supplementation with phosphatidylserine, a membrane phospholipid, vitamins and ginkgo biloba has shown improvement in memory tests and other signs of CDS in aged dogs (Araujo et al, 2008; Osella et al, 2007). S-adenosyl methionine, often used as a nutraceutical for liver disease, has also shown improvements in awareness and activity in elderly dogs (Araujo et al, 2012; Rème et al, 2008).
Omega-3 fatty acids promote cell membrane health – and in humans, they appear to be beneficial in the treatment of dementia. Combinations of omega-3 fatty acids and antioxidants are likely to work best.
Dogs older than six years of age with signs of CDS were given a supplement containing omega-3-containing fish oils, vitamins C and E, L-carnitine, alpha-lipoic acid, co-enzyme Q, phosphatidylserine and selenium for two months (Dodd et al, 2002). The supplemented dogs showed significant improvement in signs of disorientation, social interaction, decreased house soiling and a non-significant improvement in sleep-wake patterns.
Aged dogs fed a diet supplemented with antioxidants, mitochondrial cofactors and fatty acids have also shown an improvement in cognition in several other studies (Pop et al, 2010; Cotman et al, 2002; Roudebush et al, 2005). Supplements have included vitamins C and E, beta-carotene, selenium, flavonoids and carotenoids from spinach flakes, tomato pomace, grape pomace, carrot granules and citrus pulp, alpha-lipoic acid, L-carnitine, and omega-3 fatty acids.
Antioxidant dietary supplements also increased brain-derived neurotrophic factor in the serum of aged dogs (Sechi et al, 2015), and improved mitochondrial function in older dogs (Head et al, 2009).
Environmental enrichment – along with antioxidant supplementation – has shown the best results for learning behaviours in older dogs (Roudebush et al, 2005; Figure 1), although behavioural enrichment did not improve mitochondrial function beyond the effect of antioxidant supplementation (Head et al, 2009).

Middle-aged and old cats with signs of CDS were fed either a control or test diet for 12 months. The test diet included antioxidants, arginine, B vitamins, and fish oil with eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). All added nutrients except vitamin C, DHA and EPA were included in the control diet in amounts adequate, but less than in the test diet. The cats fed the test diet had better learning, memory and executive functions than control-fed cats. The cats needed to consume nutrients at higher than their daily requirements to protect against cognitive decline (Pan et al, 2013).
In pets with disturbed sleep cycles, consider selegiline at 1mg/kg each morning as this may increase daytime alertness and activity, as well as diets and supplements as aforementioned for cognitive dysfunction.
Hormone diffusers (for example, dog appeasing pheromone or feline pheromone) may help with anxiety. Melatonin is a derivative of serotonin that may inhibit dopamine; it has been used in patients with cognitive dysfunction for its influence on the sleep/wake cycle that may improve night‑time waking, phobias and noise-related fears. Note that night-time pacing/anxiety/panting can be a symptom of other problems besides cognitive dysfunction – for example, reflux oesophagitis (try omeprazole/metoclopramide at bedtime [not dinnertime] for this, with a small meal 30 minutes later).
The dose of melatonin is fairly empirical – for example, between 3mg and 9mg per dog, or between 0.1mg/kg and 1mg/kg for cats.
Note that in the UK, melatonin is not an over‑the‑counter drug and can be quite expensive. Tryptophan is a precursor to melatonin and found in some supplements used for anxiety. While these have not been studied for their sleep cycle effects, they may also help a pet that is not sleeping at the appropriate times.
It is also very important to stimulate the pet’s brain regularly throughout the day with new play toys, exercise and basic reward training.
Supplementation with medium-chain triglycerides (MCTs) – which are converted to ketone bodies in the liver – may provide an alternative brain energy source to glucose. This may compensate for the declining ability of neurons to use glucose as energy.
Aged beagles were fed either a control or test diet containing 5.5% MCTs for eight months. Feeding the test diet increased blood ketone body concentrations – and resulted in significantly better learning, memory, executive function and attention ability – compared to control-fed dogs (Pan et al, 2010).
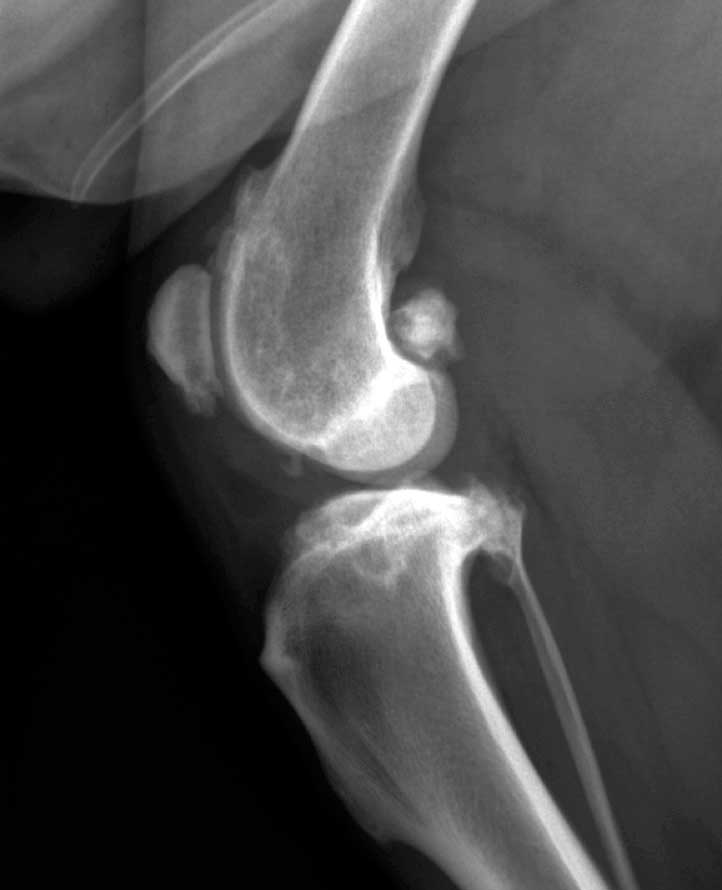
OA is common in old dogs (Figure 2) and may be even more common in old cats. Obesity and overweight body condition worsen signs of OA, and may contribute to the development of DJD (Marshall et al, 2009; Huck et al, 2009).
Weight loss of between 6.1% and 8.85% improved clinical signs in some dogs (Marshall et al, 2013).
Promoting exercise to maintain muscle mass and decrease age-related sarcopenia may also help delay the onset or progression of joint disease (Larsen and Farcas, 2014).
EPA and DHA result in production of less inflammatory fatty acids than omega-6 fatty acids, and have some anti-inflammatory properties. Good evidence exists for the use of these omega-3 fatty acids for the improvement of clinical signs of OA in dogs and cats (Rousch et al, 2010; Mehler et al, 2016; Corbee et al, 2013).
A diet enriched with green-lipped mussel has also been associated with improvement in assessed peak vertical force and gait function, and showed an increase in concentrations of plasma omega-3 fatty acids (Rialland et al, 2013), although study results vary (Larsen and Farcas, 2014; Dobenecker et al, 2002).
Glucosamine and chondroitin sulfate are precursors of cartilage, and are sometimes used orally to support cartilage synthesis in pets with OA. It has been suggested glucosamine may also have anti-inflammatory properties, and may stimulate the synthesis of joint lubricants and collagen.
Type-two collagen from chicken sternum cartilage contains high levels of proline and glycine, and, given orally, inhibits killer T-cell attack. Studies have shown a decrease in overall pain and pain on limb manipulation (Deparle et al, 2005; Comblain et al, 2017; Gupta et al, 2012).
The results of studies using these and other nutraceuticals in pets are varied, with some reporting improvement in pain and motion, and others indicating no objective changes (Larsen and Farcas, 2014). Products vary in purity and adherence to label claims.
One meta-analysis of nutraceuticals from 16 dog studies and 1 cat study concluded the evidence of efficacy of nutraceuticals is poor, with the exception of diets supplemented with omega-3 fatty acids in dogs (Vanderweerd et al, 2012). Owners report subjective improvement in their pets with nutraceuticals, and individual responses may vary.
Other than cost, the ones mentioned in this article are generally safe at reasonable doses and worth trying – especially omega-3 fatty acids.
Older cats may be thin due to disorders such as hyperthyroidism, chronic kidney disease, exocrine pancreatic deficiency, poor food intake (for example, dental disease), diabetes mellitus, or chronic enteropathy with vomiting and/or diarrhoea.
In some older cats with weight loss, none of these disorders are apparent and the cat otherwise seems to be in good health (Figure 3).

As aforementioned, cats older than 15 years of age have profound loss of fat and muscle, especially in the past two years of their lives.
It has been estimated up to 40% of cats older than 10 years of age have an apparent enteropathy that affects absorption of nutrients, including protein and fat (Williams, 2018). Pancreatitis may be part of this disorder, as these cats may have increased feline trypsin-like immunoreactivity and feline pancreatic lipase.
Due to malabsorption of fat, the faecal fat content of these cats is increased, although this is rarely measured in clinical practice. The faeces may appear relatively normal, other than possibly large in volume, but without signs of diarrhoea. The stools may have a clay‑like consistency, rather than the greasy appearance, sometimes thought to occur with steatorrhoea.
These cats are also often low in serum vitamin E, vitamin B12 and folate, and may be concurrently hyperthyroid (Williams, 2018).
Treatment for these cats is somewhat empiric, but approached similar to other chronic enteropathies. A change in diet to a hydrolysed or novel protein diet – possibly with low carbohydrate content – may help.
Supplementation of cobalamin, folate and vitamin E should be given where indicated (Williams, 2018). Lifelong supplementation of cobalamin may be needed; this can be provided orally (Toresson et al, 2017).
Prebiotics or probiotics may be also beneficial – the addition of a prebiotic (chicory) was thought to have a positive effect on weight and longevity in old cats (Cupp et al, 2008).
Many middle-aged cats – those 8 to 11 years of age – are overweight. Should the looming spectre of old-age cachexia and sarcopenia indicate that we should let these cats stay overweight?
In small one study, increasing fat reserves during middle age was not associated with longevity (Pérez-Camargo, 2010); however, in a larger study, cats with a mild overweight body condition (body condition score of 6/9) in young middle age (one to three years) lived longer than cats that had a body condition score lower than 5 – or 9/9 – at this age (Teng et al, 2018).
Maintaining activity and a diet that supports a high percentage of lean tissue is a reasonable approach. Initiation of a rigorous weight loss programme in mildly overweight senior cats should be decided on an individual basis and may be contraindicated as weight loss in senior cats is associated with decreased survival time.
“Senior” dog and cat diets have been around since about 1977. No European Pet Food Industry Federation (FEDIAF) or Association of American Feed Control Officials nutrient profile exists for senior pets, although FEDIAF has developed an information sheet about feeding older dogs (FEDIAF, 2017).
The initial concepts for senior diets were that older dogs and cats were prone to being overweight, and were at risk for development of renal disease, so these diets were lower in calories and protein than the diets designed for younger adult pets.
The body condition of senior pets can vary from very thin to very fat, so their calorie requirement varies the same way. Older cats are especially prone to weight loss, as aforementioned.
No evidence exists that increased dietary protein causes renal disease or affects the progression of renal disease. Moderate protein diets cause no ill effects in renal failure animals and are associated with a general improvement compared with either high-protein or low‑protein diets.
Inadequate protein contributes to loss of muscle mass, decreased immune competence, and decreased functions of the heart, lungs, endocrine system, gastrointestinal tract and liver.
Diets for senior pets vary in their macronutrient make-up and in supplementation with “functional foods” or ingredients, such as antioxidant cocktails or prebiotics. A cat food supplemented with vitamin E, beta‑Carotene, omega-3 and omega-6 fatty acids, and a prebiotic (chicory root) resulted in less weight loss and increased longevity, compared to a diet supplemented with vitamin E and beta‑Carotene alone (Cupp et al, 2007; 2008).
As aforementioned for cognitive dysfunction, the inclusion of antioxidants and omega-3 fatty acids that are present in some senior diets may improve alertness and brain function. Similarly, some senior diets have increased amounts of nutrients – for example, omega-3 fatty acids – which can improve the signs of OA.
The choice of whether and when to change to a diet for senior pets depends on the individual dog or cat, and its owner, as no one size fits all.
More variability exists in the needs of older pets for growing or adult pets.
The research in the benefits of senior diets for older pets certainly merits consideration of their inclusion in the feeding plan for older dogs and cats.