4 Nov 2025
Ellie Kohut DipVN, APVN, RVN provides the latest on guidance for VNs on a highly beneficial area of veterinary medicine in pets.

Image: sabbra_cadabra / Adobe Stock
Intravenous fluid therapy (IVFT) is a key part of veterinary medicine, supporting patients through conditions such as dehydration, hypovolaemia, electrolyte imbalances and other medical challenges (Hughston, 2016).
Although fluid therapy can be highly beneficial to patients, evidence-based practice is often overlooked in favour of the most familiar and widely used fluid types, such as Hartmann’s or saline, and standardised rates.
In some cases, patients may tolerate inappropriate fluid types or rates because compensatory mechanisms within the kidneys and cardiovascular system adjust to the excess volume or electrolyte load. However, in more vulnerable or critically ill patients, these compensations are less effective, and errors in fluid selection can worsen pre-existing conditions.
It is vital that we follow and utilise up-to-date guidelines and be considerate when selecting a fluid therapy (Londono, 2019). This article aims to provide veterinary nurses with the current information on different types of fluids, correct fluid rates and acid-base balance considerations.
Fluid therapy is one of the most important tools we have to treat and stabilise patients. Several types of fluids are available, and choosing the right one depends on the patient’s individual requirements. Two groups of fluids are commonly used: crystalloids and colloids.
Crystalloids are an aqueous solution of electrolytes, mineral salts and other water-soluble molecules that cross a semipermeable membrane into all body fluid compartments (Cooper, Mullineaux and Turner, 2020). Crystalloids are subdivided into isotonic, hypotonic and hypertonic solutions.
Isotonic solutions are the most commonly used fluid in general practice as they contain an equal concentration of solutes to extracellular fluid (Cooper, Mullineaux and Turner, 2020). They are used to replace losses from the extracellular space (Robinson, 2016).
Within 30 minutes, 75% to 98% of the fluids shift into the extravascular space, meaning continuous, large volumes of fluids are required to be effective (Newfield, 2021). Isotonic crystalloids are divided into:
Replacement solutions. These are used to restore extracellular fluid compartments, increase intravascular volume and improve perfusion, particularly in cases where fluid losses are greater than fluid intake (Zero to Finals, 2021) such as vomiting and diarrhoea. Their electrolyte composition and pH are similar to extracellular fluid, therefore making them a good option to treat dehydration (Hughston, 2016).
Maintenance solutions. Maintenance solutions have less sodium and more potassium than replacement fluids. Thus, they are better suited for long-term therapy once blood volume is restored and electrolytes are corrected (Hughston, 2016). They are used to sustain maintenance needs, correct solute-free water deficits, and as carriers for drug administration (Rudloff and Hopper, 2021).
Hypotonic crystalloids. Hypotonic solutions contain a lower concentration of impermeable solutes like sodium ions and chloride ions than extravascular fluid on the other side of the semi-permeable membrane (Cooper, Mullineaux and Turner, 2020).
The lower osmolarity causes fluid to redistribute across all compartments, with most moving into the intracellular space. Hypotonic fluids replenish free water deficits while accounting for maintenance requirements (Robinson, 2016).
Hypertonic crystalloids. Hypertonic solutions contain a greater concentration of impermeable solutes like sodium and chloride than extravascular fluid on the other side of the semi-permeable membrane (Cooper, Mullineaux and Turner, 2020).
This causes fluid to move from the cells and tissues into the bloodstream, leading to a rapid increase in circulating volume. They are mainly used in cases of severe hypovolaemia or to reduce raised intracranial pressure (Robinson, 2016).
Colloids are fluids that contain large molecules that increase intravascular colloid osmotic pressure because they cannot easily pass through capillary walls. They help keep fluid in the blood vessels, making them useful for expanding blood volume and treating conditions such as hypoproteinaemia (Robinson, 2016). Colloids include both synthetic preparations such as starch-based fluids and natural products such as plasma and whole blood (Newfield, 2021).
Synthetic colloids. Synthetic colloids are fluids with large molecules designed to provide oncotic pressure support within the intravascular space (Hughston, 2016). Examples include hydroxyethyl starches, gelatines and dextrans. They are sometimes used as opposed to natural colloids as they are often more readily available and cheaper (American Animal Hospital Association [AAHA], 2024a).
Natural colloids. Natural colloids include blood products such as whole blood, packed red blood cells, plasma, albumin, cryoprecipitate, and platelet-rich plasma. Unlike synthetic colloids, they also provide additional physiological benefits, such as oxygen-carrying capacity and clotting factors (Hughston, 2016).
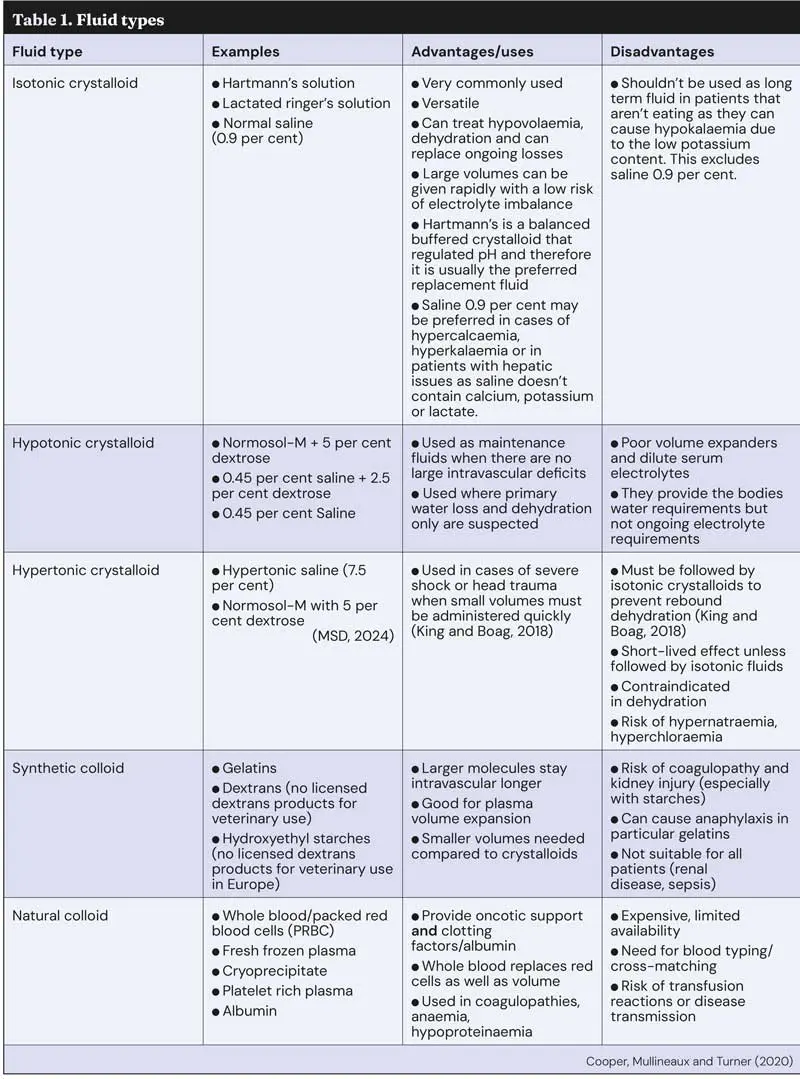
Selecting the appropriate fluid depends on the patient’s clinical status and therapeutic objectives, as each fluid type has its own indications, advantages and disadvantages, therefore making it essential for veterinary nurses to understand when and how they should be used. Table 1 shows various fluid types, their uses, and advantages and disadvantages.
Selecting the appropriate fluid depends on a patient’s condition, the clinical goals and any underlying disease. The patient’s hydration status, electrolyte level and acid-base balance also need to be considered. Fluid selection is an important component of any patient’s therapeutic plan, and it is important to remember that the initial fluid type used may not continue to be the ideal fluid type for the patient’s dynamic condition and changing needs (Donohoe, 2012). So, reassessment throughout treatment and case progression is essential.
Isotonic crystalloids are generally the first-line choice for restoring fluid deficits and maintaining hydration.
Hypotonic fluids are reserved for correcting free water deficits or hypernatraemia and for patients requiring sodium restriction, such as those with heart or liver disease.
Hypertonic crystalloids are used for rapid, small-volume resuscitation, for example, in shock or head trauma, but must be followed by isotonic fluids.
Colloids, including natural products like blood, plasma, or albumin, are used selectively for conditions such as anaemia, hypoalbuminaemia or clotting disorders (King and Boag, 2018).
Overall, fluid choice should be tailored to the patient’s specific needs, with careful consideration of electrolytes and acid-base balance. Although veterinary nurses cannot prescribe or select fluids independently, they play a vital role in advising the veterinary surgeon, monitoring patients closely and highlighting when adjustments may be required.
Fluid therapy must always be individualised to the patient, and it should never be “one size fits all”. That includes fluid rates, too.
Maintenance fluid requirements are based on sensible (sweat, urination and defecation) and insensible (respiratory) losses; however, they can be estimated as 40ml/kg per day to 60ml/kg per day or 2ml/kg per hour to 3ml/kg per hour (Lyons and Waddell, 2018).
To correct hypovolaemia in patients, a buffered isotonic fluid bolus is required. Cats require 5ml/kg to 10ml/kg and dogs require 15ml/kg to 20ml/kg across 15 to 30 minutes. This bolus can be repeated if the patient remains hypovolaemic. (AAHA, 2024b).
To treat patients suffering from dehydration, the patient’s fluid deficit needs to be calculated based on the degree of dehydration. This can be estimated using the formula:
Fluid deficit (L) = bodyweight (kg) × percentage dehydration (as a decimal).
Once the deficit has been established, fluid therapy is administered across 12 to 24 hours, alongside maintenance requirements and any ongoing losses, in order to restore hydration (AAHAb, 2024).
In hypovolaemic and distributive shock, the aim of fluid therapy is to rapidly restore circulating volume and improve tissue oxygenation, though cardiogenic shock should be excluded first to avoid fluid overload. Shock bolus volumes are based on estimated blood volume (60ml/kg to 90ml/kg in dogs, 40ml/kg to 60ml/kg in cats), but full volumes are rarely required. Instead, dogs are typically given 10ml/kg to 20ml/kg boluses of isotonic crystalloids across 15 to 30 minutes, with reassessment after each to guide further therapy. Cats are less tolerant and receive 10ml/kg to 15ml/kg boluses. When synthetic colloids are used, doses of 5ml/kg in dogs and 3ml/kg in cats are recommended (Lyons and Waddell, 2018).
Acid based balance is the body’s ability to regulate blood pH within a very narrow range. pH reflects the concentration of hydrogen ions, with lower values indicating acidity and higher values indicating alkalinity. Normal blood pH is maintained between 7.35 and 7.45, and even small deviations outside this range can have significant effects. A decrease below 7.35 is termed acidosis, while an increase above 7.45 is referred to as alkalosis (Jones, 2025).
Treating the underlying cause of an acid-base disturbance is essential and once addressed, fluid therapy can then be used. It is important to remember that certain fluids can worsen imbalances if used inappropriately. For example, studies have shown that large volumes of 0.9% sodium chloride may contribute to hyperchloraemic metabolic acidosis (Semler and Kellum, 2019).
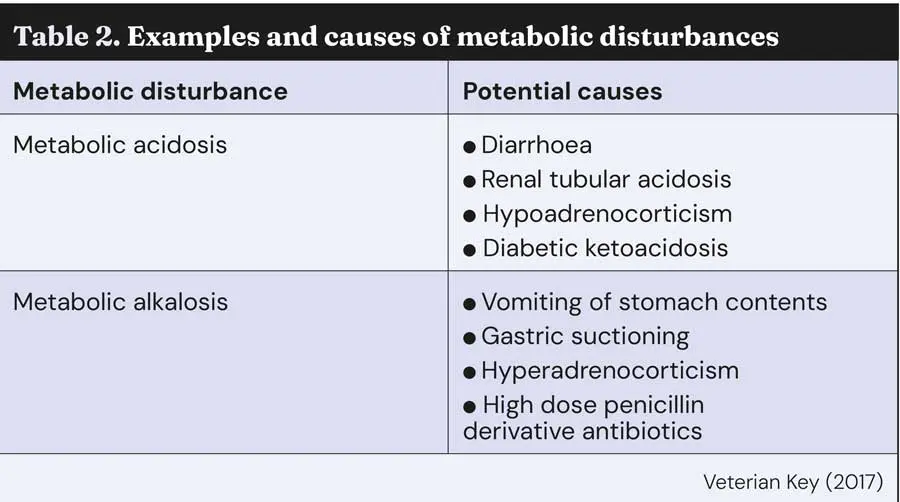
Respiratory acidosis is caused by hypoventilation (airway obstruction, depression of respiratory centres by anaesthetic drugs or neurological disease, for example), and respiratory alkalosis is caused by hyperventilation (including panting due to fear, anxiety or pain), so IVFT is going to do very minimal to correct respiratory disturbances. Metabolic disturbances can, however, be caused by a multitude of reasons that fluid therapy can help correct.
Balanced isotonic crystalloids (for example, Hartmann’s solution) contain molecules such as lactate or gluconate, which the liver metabolises into glycogen, eventually leading to the formation of CO2 and water, providing bicarbonate. Bicarbonate acts as a natural buffer, stabilising blood pH (Linklater and Hanson, 2020).
Buffered fluids, therefore, reduce the risk of acid–base disturbances, as bicarbonate buffers excess hydrogen ions, helping to restore normal pH (Veterian Key, 2017). In contrast, 0.9% saline is isotonic, but not buffered and is commonly used for patients in metabolic alkalosis.
Its high chloride content is particularly beneficial in conditions, such as persistent vomiting, where chloride loss contributes to the alkalosis (Linklater and Hanson, 2020). Acid base status and electrolytes can alter over time, therefore ongoing monitoring via blood gas analysis and assessing clinical response is vital to ensure the correct adjustments are made to the patient’s fluids as their condition alters.

A patient who has undergone surgery with prolonged gastric suctioning may develop metabolic alkalosis due to the loss of gastric acid. In this situation, Hartmann’s solution would not be ideal initially, as its lactate content is metabolised to bicarbonate and may worsen the alkalosis. Instead, 0.9% sodium chloride is preferred, as its high chloride content promotes renal excretion of bicarbonate and helps correct the alkalosis. However, prolonged use of saline carries the risk of hyperchloraemia and associated metabolic acidosis. Therefore, regular assessment of acid–base status and electrolytes is essential. Once the alkalosis has resolved, it may be more appropriate to switch to a balanced crystalloid such as Hartmann’s solution for ongoing maintenance.
Active monitoring is essential for safe and effective fluid therapy, and veterinary nurses play a vital role in this process. Regular assessment of heart and respiratory rates, perfusion parameters, body weight, urine output and laboratory values allows early identification of changes in the patient’s condition. Fluid plans should be adjusted in response to these findings, and any concerns promptly escalated to the veterinary surgeon for reassessment.
For fluid therapy to be effective and support optimal patient outcomes, the choice of fluid must be tailored to the patient’s individual needs.
Consistent and comprehensive monitoring is essential; beyond routine observations such as temperature, pulse and respiration, regular blood gas analysis provides critical insight into acid–base status. The veterinary nurse’s expertise in monitoring, and their understanding of fluid types, administration rates and acid–base physiology, plays a vital role in guiding therapy and directly impacts patient outcomes.