9 Dec 2020
Management of the airway in companion animal anaesthesia
Nuria Quesada Vicent reviews the importance of this process, as well as the equipment options and their features, and main differences
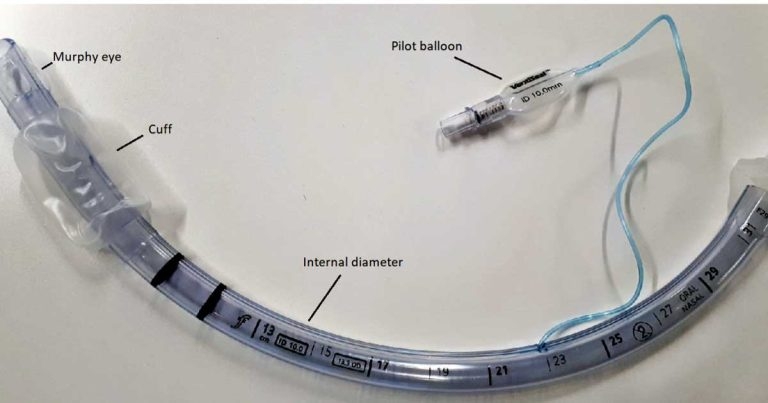
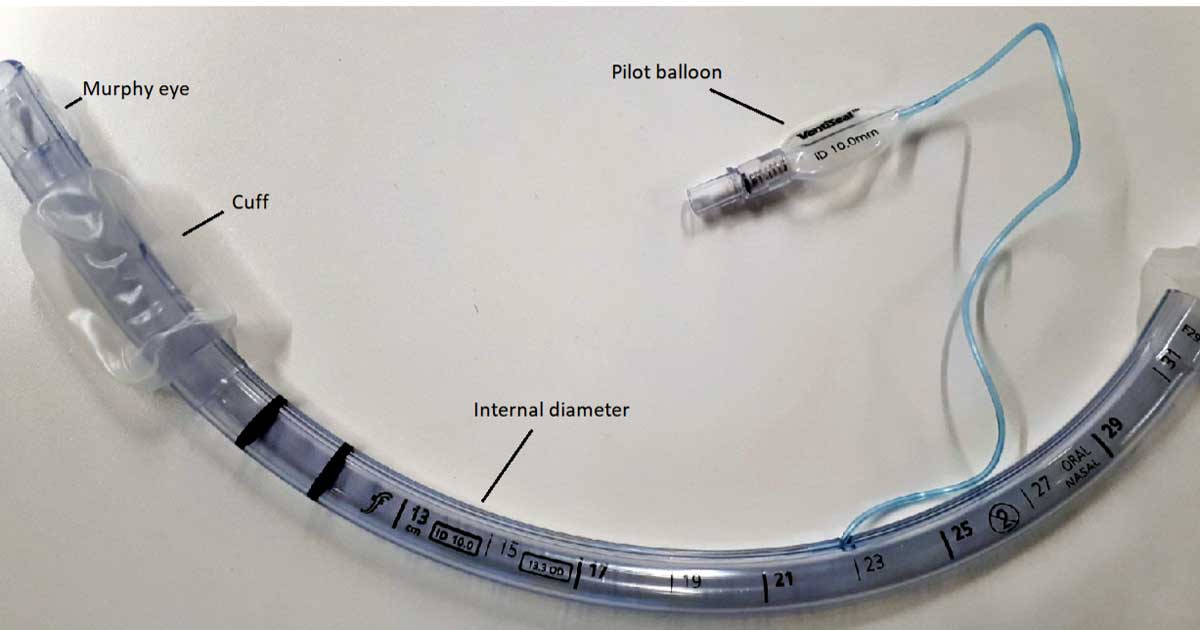
Figure 1. An endotracheal tube with a cuff.
Airway management (AM) is a life-saving procedure that should be implemented as a routine technique in all animals undergoing general anaesthesia.
AM technique ensures gas exchange through the pathway between the upper respiratory airway and lungs. A reliable AM reduces the likelihood of adverse events in animals with airway complications and/or under procedural sedation.
Therefore, all veterinary practitioners should be familiarised with AM techniques, the available equipment, its utility, the advantages and limitations, and its suitability, depending on the specific situation.
The aim of this article is to review the importance of securing the airway, the available equipment in veterinary medicine, the specific features and the main differences.
The importance of AM
AM has two main goals:
to provide a gas exchange
to avoid the diversion of gastric contents from the stomach into the airways
In daily practice, clinicians may face two scenarios in which AM must be required. The first one is an emergency situation due to upper respiratory airway obstruction; the second a routine situation when an animal is anaesthetised. However, the second situation could become the first one if an appropriate technique is not performed.
- Specific cases in which securing the airway is mandatory include:
- surgical or diagnostic procedures:
- rhinoscopy, bronchoscopy and gastrointestinal endoscopy
- dental procedures (Bellows et al, 2019)
- cervical CSF collection
- oral and maxillofacial procedures
- emergency situations that affect the neck and impair the passage of air, resulting in an upper airway obstruction (for example, neck swelling, brachycephalic obstructive airway syndrome or laryngeal paralysis)
- lower respiratory diseases that impair oxygenation and require ventilation (for example, severe lung disease, acute bronchospasm or asthma)
- cardiorespiratory arrest
Other cases in which intubation may be required – and practitioners should be prepared for – are:
- clinical conditions in which sedation may impair ventilation (for example, obesity, pregnancy, neuromuscular disease, hypothyroidism or brachycephalic breeds)
- sedation of animals with a history of vomiting and/or regurgitation, megaoesophagus, or content in the stomach, due to the elevated risk of aspiration pneumonia
- heavily sedated animals with signs of respiratory depression and hypoventilation
In most of these cases, the airway can be secured with an orotracheal intubation, but in specific situations in which oral intubation is difficult to perform – due to, for example, swelling, inflammation or oral masses – a percutaneous tracheostomy is indicated. The surgical technique is beyond the scope of this article, but information can be found in the literature.
Equipment
Face masks
Face masks were designed to fit the human nose and mouth, creating a seal. However, it is difficult to achieve a proper seal in veterinary medicine due to the differences in facial conformation.
Face masks consist of three parts:
- The mount: connects to the breathing system through a standard 15mm connection.
- The body.
- The edge: in contact with the patient´s face.
A wide variety of sizes, designs and materials (black rubber, neoprene, plastic, polycarbonate or silicone rubber) are available, and they are commonly reusable in veterinary medicine.
Polycarbonate masks: the body is transparent, and the edge has a black rubber diaphragm that can be replaced if it is damaged. In the market, clinicians can find sets that contain six masks, one of each size.
Hall’s anaesthesia masks: all parts together form one piece of soft, black, opaque rubber material. Three sizes (small, medium and large) are found in the market.
Air cushion: the body is shorter compared to the other masks and it is made by transparent plastic. The edge has a cushion that can be inflated or deflated through a valve.
In veterinary medicine, face masks are mainly used for preoxygenation in small animals and exotics, and for induction and maintenance of the anaesthesia in small mammals.
Face masks have several disadvantages:
- As they are placed outside the mouth, they do not prevent airway obstruction (Bateman et al, 2005) or protect against regurgitation.
- The differences in muzzle conformation between species and breeds make it difficult to create a seal in most cases. This produces a leakage of oxygen and/or anaesthetic gases, leading to operating room contamination. For the same reason, animals cannot be mechanically ventilated.
- They can be harmful in animals with bulging eyeballs if care is not taken.
- Some animals can feel aversive and will not tolerate them for preoxygenation if they are not well sedated.
Endotracheal tubes
Endotracheal tubes (ETTs) are tubes placed into the trachea to allow the passage of gases into the lungs.
ETTs are slightly curved to accommodate to the trachea and the distal ending is opened in a bevelled way to help the tube insertion.
Next to this opening, and opposite to the bevel, some ETTs have another hole called the “Murphy eye”. The purpose of the Murphy eye is to avoid a complete obstruction of the airway in case the distal opening is obstructed with foreign material (for example, secretions) or has been placed against the tracheal mucosa.
Another feature of ETTs is a cuff, the main purpose of which is to completely fill the space between the trachea and the tube to improve the seal. For this purpose, the cuff is connected through an inflation line to an external balloon (pilot balloon). To inflate the cuff, air is injected through a valve into the pilot balloon; the cuff is inflated until reaching a pressure enough to seal the trachea without impairing the tracheal blood flow (less than 20cmH2O to 30cmH2O; Figure 1).
ETTs are classified as cuffed or uncuffed. Additionally, the cuff can be classified as follows:
High-pressure, low-volume cuffs: these cuffs are characteristic of red rubber and silicone tubes (see later), and it is due to the material employed. To be sterilised and reused, the material had to be rigid, so a high pressure was required to inflate the cuff, achieving a low volume. The area of contact of the cuff with the trachea mucosa is also small, so higher pressures are needed to get a good seal, resulting in overinflation and damage to the tracheal mucosa.
Low-pressure, high-volume cuffs: these are characteristic of plastic (polyvinyl chloride; PVC) tubes. The plastic is thinner and softer, so less pressure has to be applied to inflate them, achieving a higher volume. Additionally, the area of contact between the trachea and the cuff is larger.
The size of the tube is determined by the internal diameter, in millimetres, while the length of the tube is marked in centimetres. The correct length of the tube goes from the incisors until the thoracic inlet.
The materials employed in ETTs are red rubber, PVC or silicone.
Originally, tubes were made of red rubber or natural latex; these can still be found on the market. The advantages of these tubes is that although they are rigid, they produce minimal tissue damage. Moreover, they can be reused after being cleaned and disinfected. The disadvantages are that they are not transparent, so secretions cannot be observed, and reusing them can damage the tube. As aforementioned, the cuff is classified as high-pressure, low-volume, and it inflates in a circular shape.
Due to these disadvantages, red rubber material was replaced by PVC or polyurethane; these are the most commonly employed in clinical practice nowadays. They can be transparent or blue, and a radiopaque line runs the length of the tube to allow their identification on radiographs. They are quite inexpensive, and the manufacturer recommends a single use, although in veterinary medicine they are normally cleaned, sterilised and reused. The cuff is classified as low-pressure, high-volume. One disadvantage of this cuff is that when inflated, small folds that create small channels are produced, allowing the pass of some gastric content.
Another material employed is silicone rubber; these tubes are mainly found in equine anaesthesia. Silicone is a soft, opaque material that can be cleaned and sterilised, so they are reusable. They are more expensive compared to the other tubes. The cuff is classified as high‑pressure, low-volume.
Other ETTs have been designed, with different conformations:
Wire-reinforced ETTs or armoured tubes: these tubes have a metal wire embedded in the wall of the tube. This structure avoids a complete occlusion of the tube in those procedures in which a ventroflexion of the neck is required (for example, ophthalmology procedures such as phacoemulsification, cervical CSF collection or cervical myelography). However, care must be taken because a “wireless area” exists where the tube is connected to the breathing system that can be kinked (Wakamatsu and Ishii, 2019). As result of this wire, the walls are thicker compared with the standard tubes, so internal diameter is smaller.
Cole tracheal tubes: these tubes were designed by Frank Cole in 1945 for paediatric and child anaesthesia. The main characteristic of these tubes is that they are narrower only in the distal end of the tube to avoid high resistance to airflow. In veterinary medicine they are used in exotic animals.
The main complication of endotracheal intubation is tracheal damage, resulting in tracheal stenosis or tracheal rupture. Although a rare complication, it has been reported in several species – including humans (Austin, 2010; Xu et al, 2016), cats (Hardie et al, 1999; Mitchell et al, 2000), horses (Miller and Auckburally, 2020; Wylie et al, 2015) and rabbits (Grint et al, 2006; Phaneuf et al, 2006).
It can be related to the cuff (overinflation of the cuff; a partial deflation of the cuff on extubation; change the patient´s position without disconnecting from the breathing system) or the technique (abrupt intubation or the use of a stylet).
An adequate tube size, a good anaesthesia plane and avoiding overinflation of the cuff reduce considerably the risk of complications.
Supraglottic airway devices – laryngeal mask airways
Laryngeal mask airways (LMA) are one type of supraglottic airway device (SAD). They were first described by Brain (1983) as a substitute of face masks and ETTs in human medicine.
More than 40 SADs are on the market that can be divided into first-generation and second‑generation SADs. Second generation SADs tried to reduce the risk of aspiration pneumonia by adding some more features.
This article will focus on the classic LMA (cLMA), as it is the one more frequently used in veterinary medicine (Figure 2).
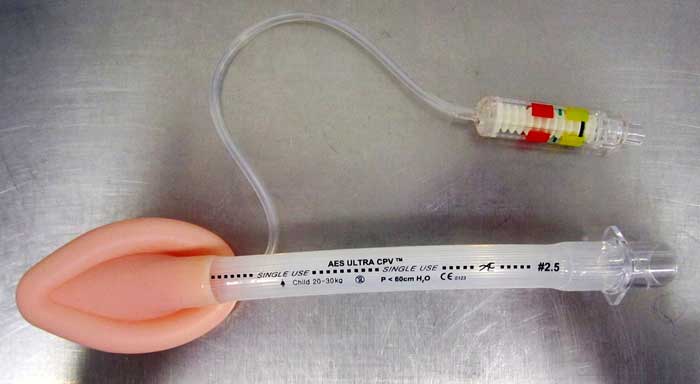
The cLMA consists of an airway tube that is connected to a bowl, surrounded by an elliptical inflatable cuff that sits over the larynx. As in the ETTs, air is injected through a valve to a pilot balloon to inflate the cuff. A maximum volume of inflation is recommended depending on the size of the mask (eight sizes are available).
The airway tube has a black line that runs the length of the convex part and helps to orientate the mask during its insertion.
LMAs are made of silicone, so can be cleaned, sterilised and reused.
According to the manufacturer, the mask has to be held like a pen with the dominant hand, with the index finger between the tube and the bowl, and inserted pressing against the hard palate until a resistance is felt. It has been reported a success rate of insertion of more than 95 per cent in human (Brimacombe, 1996) and 96.7 per cent in dogs (Wiederstein and Moens, 2008).
Although no specific design exists for veterinary medicine, Wiederstein and Moens (2008) evaluated whether the criteria used in human medicine for insertion technique and confirmation of placement could be applied in dogs. This study concluded the insertion technique described for humans is suitable for dogs of different breeds, and correct position was achieved in 96.7 per cent of the dogs at first attempt.
The device was also previously used in other species with success (Fujita et al, 1991; Cruz et al, 2000; Bateman et al, 2005).
The masks have some disadvantages making them not suitable for all patients:
- Regurgitation and aspiration pneumonia, as a complete seal is difficult to achieve.
- Mechanical ventilation can be used, but high ventilatory pressures (higher than 14cmH2O) should be avoided, as the air leaked increases gastric inflation and the risk of aspiration pneumonia. In one study comparing face masks and LMAs, some rabbits developed gastric tympanism after being mechanically ventilated (Bateman et al, 2005).
- They can be dislodged quite easily.
- Likelihood of airway obstruction if they are not correctly positioned.
- Possibility of pharyngeal damage due to pressure inflations. Bateman et al (2005) described lyngual cyanosis in two rabbits.
SADs – v-gel
V-gel devices are a variation of i-gel devices (Levitan and Kinkle, 2005), another type of SAD used in human medicine, developed by Muhammed A Nasir and launched to the market in 2007.
V-gel devices are designed for veterinary use – specifically cats, rabbits and small dogs, although its use has been reported in other species, such as hedgehogs (Baldo and Boelke, 2020). The prototype was presented by Cortaz (2010) and introduced to the market in 2012.
In 2020, a second‑generation device (v-gel advanced) for cats and rabbits has been introduced in the market, with features that improve the previous generation.
These devices are made of soft plastic and silicone, and are species-specific to ensure a proper seal in the oropharyngeal inlet. They are inserted orally until reaching the pharynx where, due to their shape, they fit the anatomy and self-guide into the position.
Six sizes are available in both cats (C0 to C5) and rabbits (R1 to R6), related to the ideal bodyweight of the animal (Figure 3). According to the manufacturer, they can be sterilised and reused up to 40 times.

As LMAs, they do not protect completely against regurgitation and may be dislodged quite easily. Correct positioning should always be checked with capnography to avoid airway obstruction.
Comparison between devices
Several studies have compared the different airway devices, which mainly focused on the ease of insertion (for example, amount of inductor agent used, time for placement and number of attempts) and the likelihood of air leakage during controlled mechanical ventilation (CMV).
Ease of placement
Dogs
Wiederstein and Moens (2008) compared the dose of anaesthetic agent required to insert an LMA versus an ETT in dogs.
In 14 of 30 cases (47 per cent) in the LMA group, the insertion was achieved with sedation, and the administration of an induction anaesthetic agent was not required. On the other hand, intubation with sedation alone was only possible in 1 of 60 cases (3.3 per cent) in the ETT group; besides, 50 per cent (30 of 60) of the dogs required two doses of propofol to be intubated.
Therefore, although the correct placement of the device was not confirmed with imaging in this study, a significantly less dose of inductor anaesthetic agent was required for LMA placement compared to ETT.
Cats
Prasse et al (2016) compared v-gel, ETT and LMA devices, and showed that significant less propofol was needed for v-gel placement when compared with ETT, while no difference in propofol dose was found between the v-gel and LMA devices. No differences in number of attempts were found among groups either.
Cassu et al (2004) reported as well that a lower dose of thiopental was required for LMA insertion compared to ETT.
On the contrary, van Oostrom et al (2013), and Niyatiwatchanchai and Thengchaisri (2020) showed no significant differences in propofol dose between v-gel and SAD versus ETT for intubation in cats. However, less time was recorded to place the v-gel (van Oostrom et al, 2013).
Minor propofol dosage, short time and reduced number of attempts were shown when the technique placement was performed by inexperienced veterinary students in comparison with ETT (Barletta et al, 2015).
Rabbits
Similarly to cats, inexperienced clinicians needed four to six minutes to place the ETT versus 30 seconds for the LMA, although no difference in time was reported when a trained person performed the placement of the airway device (Smith et al, 2004).
Cruz et al (2000) and Engbers et al (2017) compared LMA and SAD with ETT insertion. A significantly lower dose of thiopental was needed to insert the LMA (Cruz et al, 2000) and less time to insert the SAD (Engbers et al, 2017), with no difference in number of attempts.
Finally, Wenger et al (2017), compared the four devices (v-gel, LMA, face mask and ETT). The face mask needed significantly less propofol and time to be placed compared to the other three techniques. No difference in the total dose or duration among v-gel, LMA and ETT were found. Face mask placement took fewer attempts than the ETT, but no difference with v-gel and LMA was reported.
CMV and air leakage
Cats
Cassu et al (2004) compared an LMA and an ETT in cats ventilated with a tidal volume (Vt) of 20ml/kg-1 and a peak inspiratory pressure (PIP) between 10cmH2O and 12cmH2O. No differences in arterial oxygen pressure (PaO2), arterial carbon dioxide pressure (PaCO2) or air leakage were found between groups. Nevertheless, gastric reflux was detected in some cats in both CMV groups.
On the other hand, Prasse et al (2016) compared the LMA, v-gel and ETT devices in cats ventilated at different PIPs (8 cmH2O to 16cmH2O), and concluded that ETT had significantly more leakage than the v-gel and LMA groups when PIP was superior to 8cmH2O.
Rabbits
Bateman et al (2005) compared face mask and LMA devices. Rabbits in dorsal recumbency showed dyspnoea and airway obstruction with FM, while four out of six developed gastric tympanism after being mechanically ventilated with a pressure of 14cmH2O in the LMA group.
Wenger et al (2017) compared the four devices when applying CMV at different PIPs (6cmH2O to more than 16cmH2O). Nine of 10 rabbits in the face mask group, 2 of 10 in the LMA group and 4 of 10 in the v-gel group had a leak at 6cmH2O. No air leakage was detected in the ETT group with PIP below 16cmH2O. In this study, the amount of gas in the stomach was significantly higher in the face mask and LMA groups after a CMV of 14cmH2O.
- Some drugs are not licensed for veterinary use.
