7 Jan 2019
Managing canine and feline trauma and surgical wounds
Daniela Murgia details methods of handling this condition, referencing the primary and secondary surveys of patient trauma.

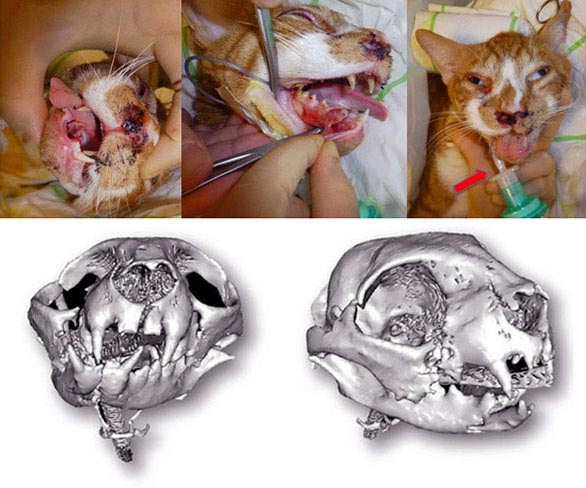
Figure 1. A young cat with head trauma following a road traffic accident. Multiple mandibular, maxillary, left orbital and nasal bone fractures resulted in malocclusion and nasal bleeding, with increased upper respiratory noises, but no respiratory distress. The red arrow indicates the endotracheal tube placed via a pharyngostomic approach to allow surgical reduction of the mandibular/maxillary fractures. Image: © AHT, Newmarket.
Trauma is one of the most common problems dogs and cats encounter.
Trauma is defined as a “wound or injury” and may occur secondary to the likes of motor vehicle accidents, fall from heights, animal interactions and human-animal interactions. Severity may range from mild to fatal. Trauma may affect only one organ system or multiple ones, either directly or indirectly. Therefore, a global and thorough approach is required to improve survival and decrease morbidity in trauma patients.
General practitioners are expected to have an intimate understanding of every condition affecting pets – trauma being one of them. The requirement for global understanding is very challenging, hence the attempt with this article to provide some practical suggestions the practising vet can use in the everyday clinic to assist in the quick assessment and treatment of the trauma patient.
Success in the management of small animal trauma patients is based on the ability of the veterinary team to rapidly identify and manage immediately life-threatening problems.
Triage is defined by Encarta 2001 as “the process of prioritising sick or injured people for treatment according to the seriousness of the condition or injury”. Triage of small animal patients presented for emergent problems serves the dual purpose of allowing the clinician to prioritise one patient over another, but also identifies life-threatening problems and the need for immediate intervention.
Initial assessment of the trauma patient occurs quickly, but can theoretically be broken down into two major phases: primary survey and secondary survey.
The primary survey is the assessment of the respiratory and cardiovascular systems, followed by assessment of the CNS and urinary tract system. The secondary survey is the assessment of all other systems once the animal’s most immediately life-threatening problems – identified during the primary survey – are dealt with.
Primary survey
The primary goal in attending to a critically injured trauma patient is to optimise oxygen delivery to the tissues assessing and maintaining oxygen saturation of haemoglobin. In fact, during the initial approach and resuscitation of these patients, all procedures are oriented toward this goal. Oxygen delivery is dependent on respiratory function, cardiac output, haemoglobin concentration and oxygen saturation of haemoglobin. It is important to optimise these variables at all times.
Clinical signs of respiratory compromise include increased respiratory rate or effort, restlessness, extended head and neck, abducted elbows, paradoxic movement of the chest and abdominal walls (normally should move in and out together, but with paradoxical movement they move in opposite directions), flail chest, pale or cyanotic mucous membranes, increased heart rate, increased upper airway sounds or altered lower airway sounds (increased or decreased airway sounds).
Nasal airway and frontal sinus injuries can result in bleeding into the nasal passages, causing upper airway sounds. Despite this problem, most animals do not suffer respiratory compromise from these injuries (Figure 1).
Decreased air sounds on auscultation usually indicates pleural space disease. Traumatic causes of pleural space disease include pneumothorax (most common), diaphragmatic hernia and severe haemothorax.
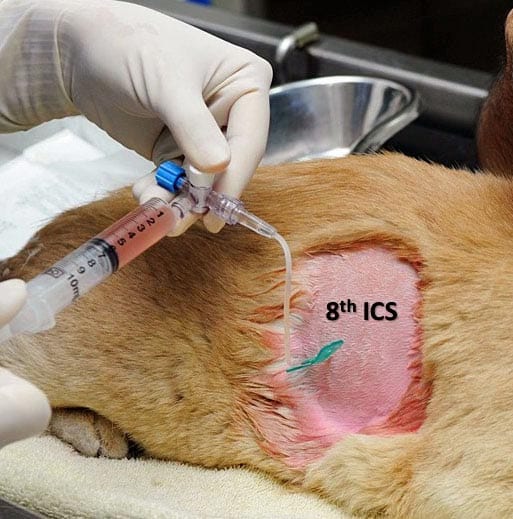
If the patient is in respiratory distress and the lung sounds cannot be heard then thoracocentesis is warranted (Figures 2a and 2b). Increased lung sounds on auscultation indicate lower airway/pulmonary parenchymal injury, such as pulmonary contusions. Therapy for pulmonary contusions is largely supportive, with caution of overzealous fluid therapy.

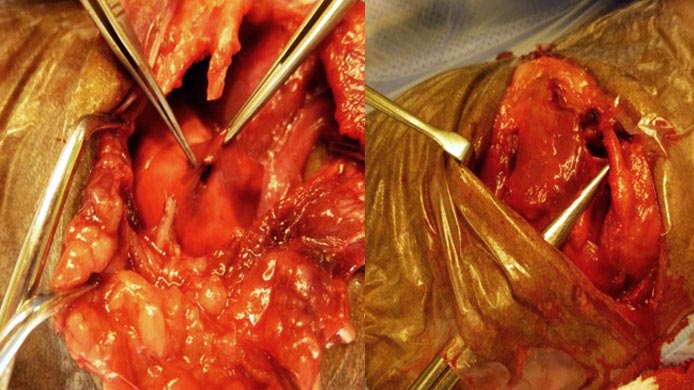
Loud upper airway sounds heard without the stethoscope indicate upper airway compromise (from the carina forward). Traumatic causes of upper airway problems include cervical tracheal crush injury (bite wounds are most common), pharyngeal injury (swelling/bleeding) and tracheal avulsion (Figures 3a and 3b).


Open chest wounds
Thoracic injury is common following trauma and is a leading cause of small animal death. Thoracic wall trauma is relatively common in dogs and cats, and may occur as a result of either blunt force trauma (motor vehicle accidents, falling from a height) or after attacks by other animals.
Penetrating injuries resulting from knives, projectiles and foreign bodies may also be encountered. Although the risk of damage to intrathoracic structures after blunt force trauma is high, surprisingly few patients experience serious injury to the thoracic wall. Only few dogs experiencing blunt force trauma are diagnosed with chest wall trauma.
In human medicine, the following time intervals after injury to the respiratory and cardiovascular system have been described:
- Survival hour: during which most deaths occur due to catastrophic, unsalvageable injury to the respiratory and cardiovascular system. Will the patient survive the hospital journey?
- Golden period: the next two to four hours, which is the most common presentation at hospital. Prompt, aggressive treatment makes a difference in survival. Most treatable cardiovascular and respiratory injuries are seen in this period.
- The third interval occurs three to five days after the trauma. It is in this interval that hidden injuries, insidious decline, organ failures and imminent sepsis become evident.
Patients with thoracic trauma can decompensate rapidly. Any additional stress could, therefore, be life-threatening and lead to increase of the respiratory rate and oxygen requirements. Early stabilisation relies mainly on oxygen supplementation.
This can be achieved with the use of oxygen masks, which are inexpensive, easy to administer and can achieve high inspired O2; however, they require restraint in awake patients and they are not well tolerated by some patients.
For smaller patients an enriched oxygen environment, such as an oxygen cage and neonatal incubator, can also be used (Figure 4).

These offer the advantage of a non-stressful environment where high inspired O2 concentration can be achieved, and humidity and temperature controlled. However, a wastage of oxygen can occur and oxygen supplementation is interrupted when the cage door is opened.
Patients that have experienced known or suspected thoracic trauma should be carefully evaluated for flail chest, pulmonary contusion or laceration, and diaphragmatic rupture. Skin lacerations in the thoracic region should be examined for deeper wounds that might communicate with the pleural space.
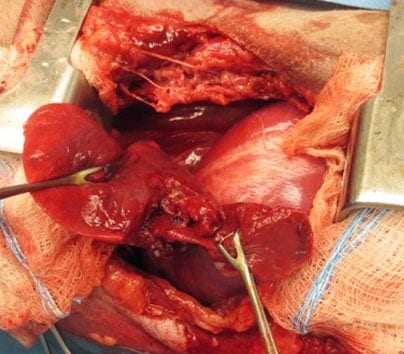
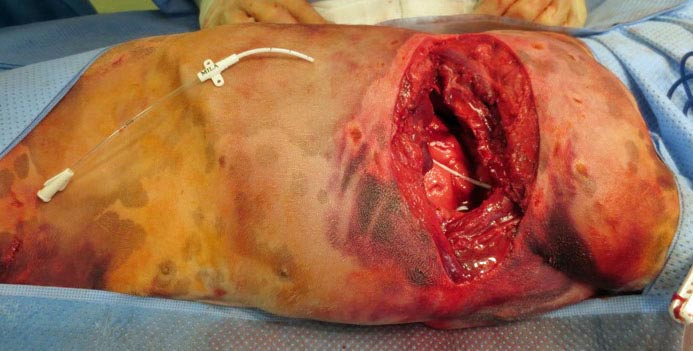
Dog bite injuries can be particularly severe because of the action of the canine teeth after they penetrate the skin and any shaking of the victim by the attacker. With bite wounds, the skin may remain largely intact except for a few puncture marks. Despite this, surgical exploration may reveal full-thickness tears of thoracic musculature, rib fractures and floating rib segments, and pulmonary lacerations (Figure 5).

Patients with penetrating injuries should undergo routine stabilisation followed by diagnostic imaging to determine if damage is to the lungs or the mediastinal structures.
Emergency thoracotomy for thoracic trauma has a very high mortality rate in humans (as high as 99% for blunt trauma and 91% for penetrating injuries); hence, the decision to operate requires careful consideration.
Full-thickness open defects of the chest wall connecting to the pleural space and that allow free air movement into the pleural space (so-called “sucking” chest wounds) should be immediately clipped and covered with a sterile bandage, which will create a seal, re-establishing pleural space integrity. Thoracocentesis or placement of a thoracostomy tube should then be performed to remove the residual air. If respiratory distress persists, intubation and positive pressure ventilation should be provided until the wounds can be surgically repaired.
Once stabilised, these patients should undergo exploratory thoracotomy for assessment of deep injuries, such as lung parenchyma perforation or laceration and for pleural space flushing. Surgery offers the opportunity to debride highly devitalised muscle, which may reduce the risk of infection, and to stabilise the thoracic wall as needed. It is always recommended to send a sample taken from the thoracic cavity for bacterial culture and sensitivity (Figures 5 to 7).
Pulmonary contusions are the most common injuries following blunt thoracic trauma. Hypoxaemia occurs, and pain-induced hypoventilation is also contributory. If the injuries are particularly severe, bloody fluid in the oropharynx and trachea can be seen. Thoracic auscultation may reveal moist rales, and/or bronchial sounds.
Pulmonary contusions may be seen on thoracic radiographs and may not be evident clinically or radiographically for more than 24 hours post-trauma. Arterial blood gas monitoring and clinical signs are the most sensitive means of detecting respiratory compromise. Treatment consists of supportive care with oxygen supplementation, analgesia and cage rest. In particularly severe cases, positive pressure ventilation is required.
Fractures of the thoracic cage and flail chest require copious analgesia and rest – they compromise respiration secondary to pain and are indicative of much underlying lung pathology. Fractures of cranial ribs are often seen in association with severe cardiovascular trauma and fractures of the caudal ribs are seen with cranial abdominal trauma.
Sternal recumbency or flail side down may limit pain and further injury. Wrapping the chest often decreases compliance instead of stabilising fractures.
If surgical exploration is required, the animal should be anaesthetised and ventilated in the event that a pneumothorax develops intraoperatively. The skin is incised over the area of greatest injury, and the soft tissues are carefully evaluated. Visibly devitalised tissue, including skin, should be excised.
Secondary to trauma, ribs may be stripped of their soft tissue attachments; floating segments without adequate blood supply should be removed. The lungs should be inspected for perforation, the thorax lavaged carefully and a thoracic drain inserted (Figure 8). Appropriate antibiotic therapy should be instituted.
The necessity for reconstruction or stabilisation of the thoracic wall depends on the type of damage sustained. In most instances, rib fractures can be treated conservatively with pain relief, and control of problems arising from pleural fluid and pulmonary compromise. Fractured ribs may also be stabilised by securing them to intact adjacent ribs with circumcostal sutures of heavy-gauge material. If multiple intercostal lacerations are present, sutures may be preplaced in a “basket-weave” fashion, in which encircling sutures alternate around cranial ribs and caudal ribs, so the sutures overlap.
Current thought is respiratory problems in patients with flail chest are most commonly from underlying pulmonary trauma rather than the presence of the flail segment.
When flail segment stabilisation is considered appropriate, the most commonly used method is one that involves percutaneous fixation of the ribs within the flail segment to an external brace. Non-absorbable sutures of an appropriately sized material (2-0 to 1, depending on the size of the patient) are passed around the ribs within the flail segment, and at least one rib cranial and caudal to the flail segment.
The principle is similar to that used when treating pectus excavatum. Pericostal sutures are tied to a rigid or semi-rigid splint, pulling the flail segment outward and encouraging it to move in concert with the intact thoracic wall. Sutures and external scaffolding are left in place for approximately two weeks until enough fibrous tissue has formed to reduce mobility of the fractured ribs.
Acrylate plate has been investigated as a method for rib stabilisation, but sound evidence supporting its use in clinical patients has not yet been reported.
Traumatic shock
Traumatic shock results in a maldistribution of blood flow mainly because of hypovolaemia. This leads to persistent peripheral hypoperfusion, which can damage the cellular membranes. This results in release of enzymes (phospholipase, cyclooxygenase and lipoxygenase) that produce thromboxane and leukotrienes:
- Thromboxane causes vasoconstriction, further compromising tissue perfusion and stimulating platelet aggregation.
- Leukotrienes propagate the inflammatory response with mobilisation and activation of neutrophils.
- Neutrophil release lysosomal enzymes and toxic oxygen metabolites that cause further cellular damage, leading to oedema with subsequent increase of oxygen diffusion distance to the cells from the capillaries.
At presentation, supplemental oxygen should be provided to the trauma patient until assessment of an arterial blood gas is available because optimising tissue oxygen delivery will minimise the perpetuation of these inflammation-producing cascades.
One of the most vital functions of the circulation is to maintain tissue oxygen delivery at a level that meets the tissue’s metabolic requirement for oxygen.
When tissue oxygen delivery and the tissue’s metabolic requirement for oxygen are in balance, aerobic metabolism can be sustained. This is an efficient way to maintain adenosine triphosphate (ATP) production and, therefore, cell membrane pump function and cellular integrity. Shock occurs when tissue oxygen delivery is insufficient to meet the metabolic requirement for oxygen delivery at the tissue level.
Aerobic metabolism, therefore, can no longer be sustained and anaerobic metabolism ensues. Anaerobic metabolism is an inefficient means of ATP production and leads to generation of a lactic acidosis. Left uncorrected, a tissue oxygen debt develops, cells and organs become hypoxaemic, and cellular and/or end-organ damage occurs, which can ultimately result in cell death and organ failure.
As previously mentioned, assessment of the cardiovascular systems and tissue perfusion belong to the primary survey.
Initial assessment of adequate cardiac output and circulating volume includes mucous membrane colour, capillary refill time, pulse rate, and quality. Abnormalities indicating poor tissue perfusion include pale or grey mucous membranes, prolonged capillary refill time (more than two seconds), and weak and rapid pulses.
Measurement of arterial blood pressure should be performed when possible: a Doppler systolic blood pressure of less than 80 is suggestive of decreased tissue perfusion. A mean arterial pressure of under 60mmHg is suggestive of decreased tissue perfusion. It should be kept in mind blood pressure may be normal or even high and peripheral tissue perfusion could still be inadequate for the body’s requirements.
The most common cause of poor tissue perfusion in the trauma patient is hypovolaemia from blood loss. The signs and symptoms of acute peripheral circulatory failure (shock) depend on the degree of blood volume depletion, the duration of that depletion and the ability of the body to compensate.
The most common areas for haemorrhage causing hypovolaemia are, in order of frequency: the peritoneal space, retroperitoneal space, thigh musculature, pleural space or a combination of spaces (such as retroperitoneal and peritoneal).
The less common causes of poor tissue perfusion are cardiac arrhythmias, tension pneumothorax, diaphragmatic hernia, peritoneopericardial diaphragmatic hernia, and cardiac tamponade due to haemopericardium from traumatic atrial rupture.
Poor tissue perfusion should be treated with IV fluids, colloids or blood products. Fluids resuscitation should be used with caution when pulmonary contusions are present.
The primary survey also includes the assessment of the brain and neurologic function, and the renal system. It is important to assess brain function at presentation to obtain a baseline for potential dynamic changes that may occur. However, conclusions regarding brain and neurologic function (brain and spinal cord) should be withheld until perfusion is adequate and function is reassessed.
Assessment of brain function includes the grade of mentation, such as excited/agitated, normal, depressed, obtunded markedly decreased level of consciousness and arousable with auditory or tactile stimulation. Assessment of the spinal cord function includes palpation of full length of the spine and pelvis, observation of any voluntary movement of all legs, assessment of the ability to stand and ambulate, checking the anal tone and anal reflex, and checking proprioception of limbs with assessment of limb reflexes (Figure 9).

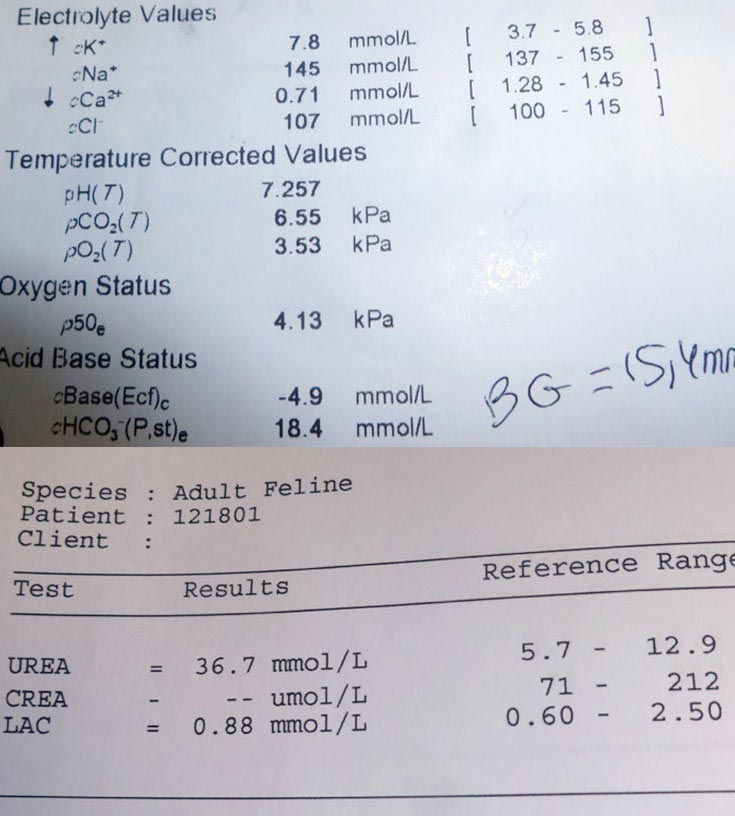
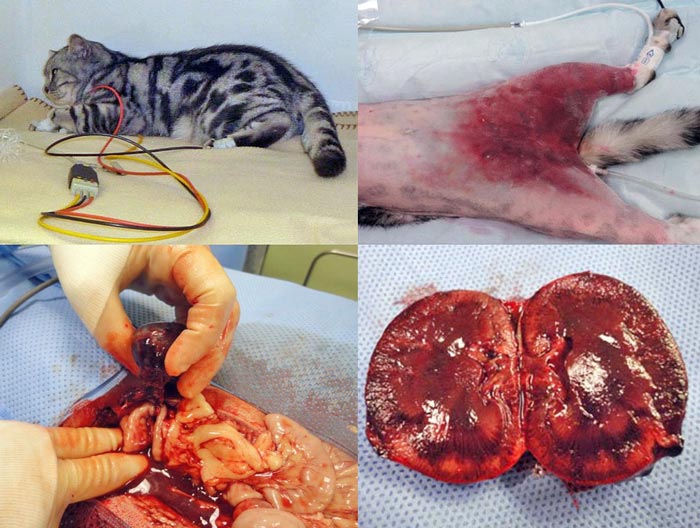
Physical assessment of the urinary tract is limited to palpation of the urinary bladder and kidneys. Urinary tract injury seems to occur more commonly with pelvic fractures and renal parameters, such as serum urea and creatinine may not have substantial increases until several hours after urinary tract rupture or injury.
The presence of haematuria may indicate urinary tract injury or simply small tears of the urinary bladder mucosa. Manifestations of renal damage may not be immediately evident at presentation and not detected until several hours later, after continuous monitoring. Potential trauma-induced urinary tract injuries include renal contusions, rupture, or avulsion, renal pelvis disruption, urethral disruption, urinary bladder rupture and urethral trauma/rupture.
In general, the treatments for urinary tract trauma include fluid therapy and stabilisation of cardiovascular manifestations of urinary tract injury, such as hyperkalaemia, which may manifest with bradyarrhythmia followed by reparative surgery (Figures 10 and 11).
Secondary survey
The secondary survey is the assessment of all other systems once the animal’s most immediately life-threatening problems, identified during the primary survey, are dealt with.
The secondary survey consists of a thorough full physical examination, with particular attention paid to the musculoskeletal system:
1. Observe limb function of all four legs.
2. Observe ambulation.
3. Complete palpation of appendicular and axial skeleton including rectal examination, palpation of skull, and manipulation of the jaws and peripheral nervous system with full evaluation of peripheral nerves.
The patient should be examined from the tip of the nose to the tip of the tail.
It is outside the scope of this article to cover the ABCs of emergency care, but it is essential vets (and the team as a whole) are familiar with this in presence of emergent trauma patients. It is recommended to consider running regular ”crash drills” in your practice, so everyone is confident about their role within a critical case and to have a “crash box” always available that is only used for emergencies.
The crash box (Table 1) should be restocked after every usage and a seal placed over the latch to document this. The crash box should be opened weekly to check drug expiration dates and ensure adequate stock of required supplies. This equipment will allow the practitioner to maintain an open airway, institute rescue breathing and carry out all aspects of cardiopulmonary resuscitation.
| Table 1. Contents of a crash box | |
|---|---|
| Equipment | Purpose |
| Laryngoscope | Facilitate intubation |
| Cuffed endotracheal tubes of different sizes | Endotracheal intubation of dogs and cats of all sizes |
| Cuff syringe | Endotracheal tube cuff inflation |
| Roll gauze | Secure endotracheal tube |
| Ambu-bag (to be connected to O2 source) | Positive pressure ventilation with 100% O2 |
| Epinephrine and atropine | Cardiopulmonary cerebral resuscitation (CPCR) and bradyarrhythmias |
| Naloxone 0.4mg/ml | Reversal of opiates |
| Calcium gluconate (10%) | Antagonise conduction disturbances associated with hyperkalaemia |
| Reversal agents for any anaesthetics commonly used (such as atipamezole and flumazenil) | Reversal of anaesthetics |
| Small surgical pack (scalpel, mayo scissors, hemostats, drape and tissue forceps) | Emergency thoracotomy, tracheostomy, venous cutdown and occlusion of arterial haemorrhage |
| Sterile gloves | Maintain sterile technique |
| Scalpel blades (10 and 11) | Surgical procedures |
| Drug dosing scale (based on bodyweight) for all drugs in box | Quick dose reference |
| IV catheters | IV access for drug and fluid therapy |
| IV fluid set | IV fluid delivery |
| Red rubber catheter | Intratracheal drug delivery for CPCR |
| Syringes and needles of various sizes | Drug delivery |
| 0.9% sterile saline solution | Flush solution for drug delivery |
| Butterfly needles (19g and 21g) | Feline thoracocentesis |
| IV extension tubing | Canine thoracocentesis |
| Three-way stopcock canine and feline | Thoracocentesis |
| Spinal needles | Intraosseous access in puppies and kittens |

In addition, the necessary supplies for venous or intraosseous access, the reversal of sedatives and anaesthetics, management of pleural space diseases, emergency tracheostomy and control of arterial or severe venous haemorrhage, are included (Figure 12).
- All cases described in this article are from patients treated when the author was working at the AHT in Newmarket.
Meet the authors
Daniela Murgia
Job Title