20 Jan 2025
The liver has many important roles, so a disease of this organ can present in a variety of forms, cause a wide array of clinical signs, call for many different treatments and require a variety of nursing needs.
Nursing these patients can be time consuming, but provides great job satisfaction.
The liver is the largest gland in the body and has numerous functions (Figure 1). These include:
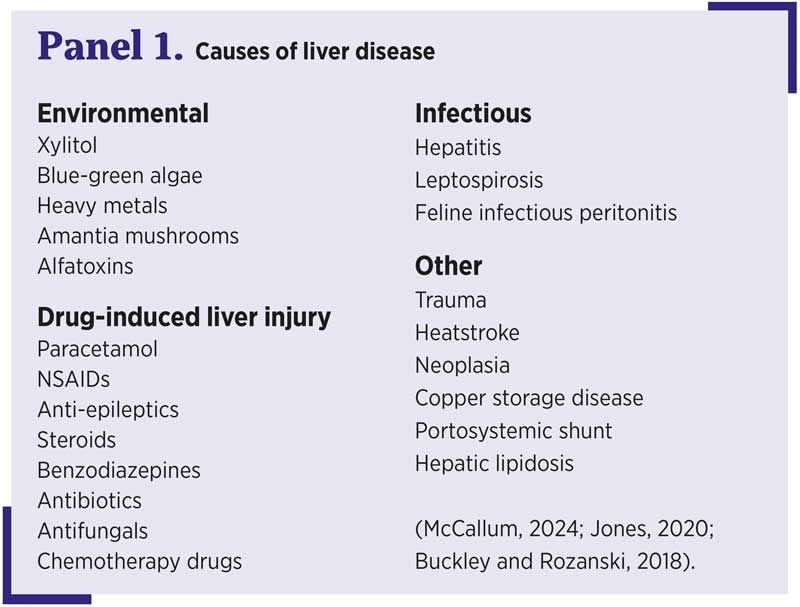
Diseases of the liver are many and diverse (Panel 1). Many patients will present with vague clinical signs such as weight loss, anorexia, lethargy, vomiting, diarrhoea, polyuria and polydipsia. Morlivee specific clinical signs include ascites, oedema, jaundice, coagulopathies, neurological signs and hypoglycaemia (Warland, 2019; Buckley and Rozanski, 2018).
As the liver has such a large reserve capacity, many signs of liver disease are not seen until more than 70 per cent of liver function is lost (McCallum, 2024).
 Jaundice occurs when excess amounts of bilirubin are in the blood (hyperbilirubinaemia). This can be seen most easily seen on non-pigmented areas of the inner pinna, abdomen and sclera. This does not necessarily indicate liver disease, so should be assessed along with other clinical signs (Arbach, 2023).
Jaundice occurs when excess amounts of bilirubin are in the blood (hyperbilirubinaemia). This can be seen most easily seen on non-pigmented areas of the inner pinna, abdomen and sclera. This does not necessarily indicate liver disease, so should be assessed along with other clinical signs (Arbach, 2023).
In particularly high levels, it is possible for bilirubin to cross the blood-brain barrier, which can induce bilirubin encephalopathy (Gow, 2024).
Ascites (Figure 2) occurs when fluid builds up in the abdomen, because fluid leaks from the splanchic vasculature faster than the rate at which the lymphatic system can drain it (Gow, 2024). This can be caused by portal hypertension or reduced colloid oncotic pressure from hypoalbuminaemia.

Hepatic encephalopathy is the manifestation of neurological signs due to increased levels of toxins usually metabolised in the liver, with ammonia (NH3) being the most significant (Warland, 2019). These signs include ataxia, lethargy, head pressing, ptyalism, seizures and stupor (Smith, 2018).
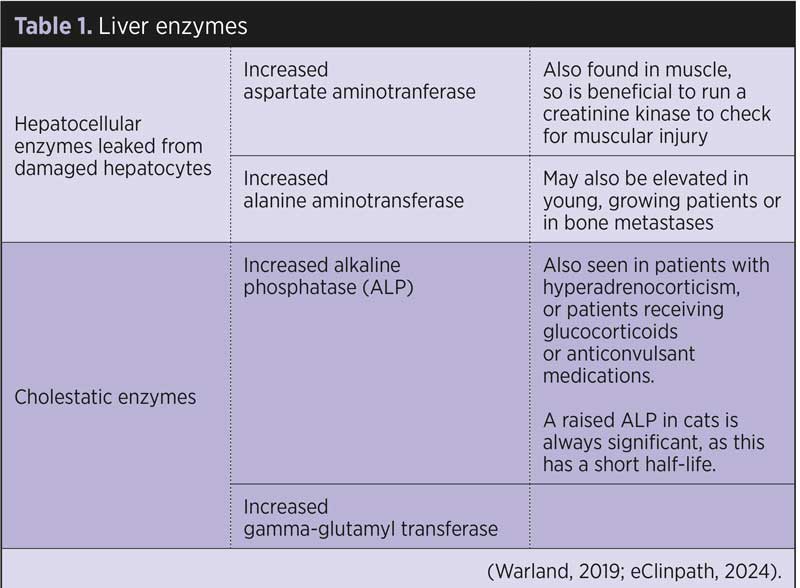
Bloodwork in hepatic patients may show increased liver enzymes, yet this does not tell us about the function of the liver (Table 1).
 Other blood abnormalities that may be seen are low urea, albumin, glucose and cholesterol; prolonged prothrombin time (PT) and activated partial PT; anaemia; and increased bile acids, ammonia and bilirubin (Warland, 2019; Arbach, 2023; eClinpath, 2024).
Other blood abnormalities that may be seen are low urea, albumin, glucose and cholesterol; prolonged prothrombin time (PT) and activated partial PT; anaemia; and increased bile acids, ammonia and bilirubin (Warland, 2019; Arbach, 2023; eClinpath, 2024).
X-rays may show an enlarged liver, hepatic masses and ascites.
Ultrasound gives more information on the vasculature and parenchyma, and allows us to examine the biliary tract and gall bladder, and identify the presence of any free fluid. Abdominocentesis can then be performed. Large volume drainage is controversial, but may be required in rare cases if the patient is very uncomfortable and dyspnoeic (Gow, 2024).
Ultrasound-guided fine-needle aspirates of the liver may be undiagnostic (Warland, 2019). Surgical biopsies may be needed, but coagulation times must be measured before this to assess the risks of bleeding during the procedure (Jones, 2020).
Serial blood samples can help to assess trends and tailor treatment plans. A central line is advantageous in taking serial blood samples, as it is less stressful than multiple venepuncture (Gray, 2019).
Schumacher (2016) pointed out that it is still important to remember not to take a volume that exceeds 10 per cent of the patient’s total blood volume per week.
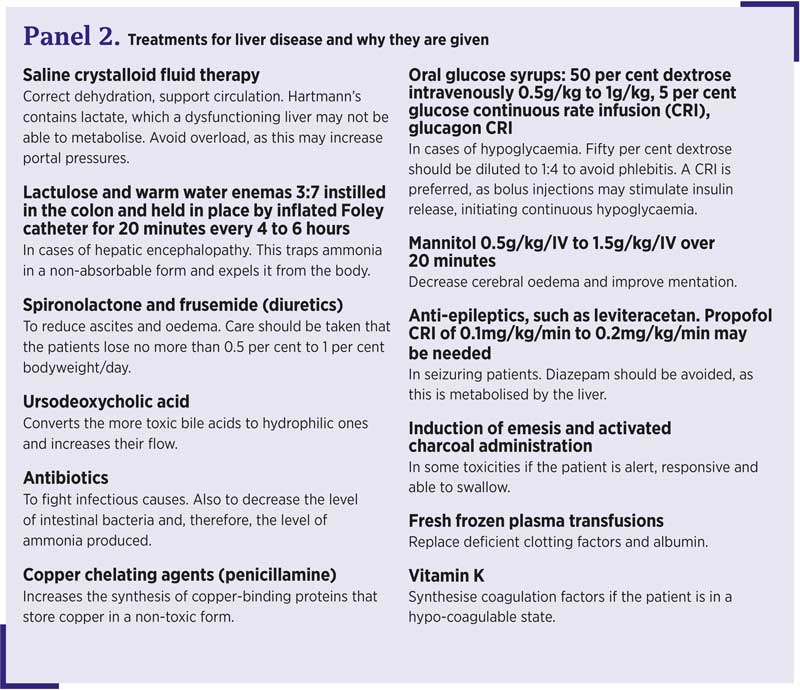
Panel 2 shows the numerous treatments that may be prescribed in the hepatic patient.
It is important that animals receive good-quality nursing care to alleviate pain, stress and anxiety. Veterinary nurses can do this by providing comfortable housing, dimmed lighting, places to retreat or hide, playing calming music or audiobooks, pheromone therapy, and grouping treatments and walks so the patient has time to rest (Lloyd, 2017).
The hepatic patient may have various lines in place such as feeding tubes, wound drains and central or peripheral IV lines. Gray (2019) suggests all lines should be labelled to avoid any confusion with administering medications and feeds (Figure 3). A patient should be reverse barrier nursed if it has any kind of wound drain (Gray, 2019).

Various nursing care plans are used in veterinary practice to tailor nursing care to the individual. Nelson (2015) suggests a client interview on admission to gain an insight into the patient’s normal behaviours, so stress and anxiety can be better managed.
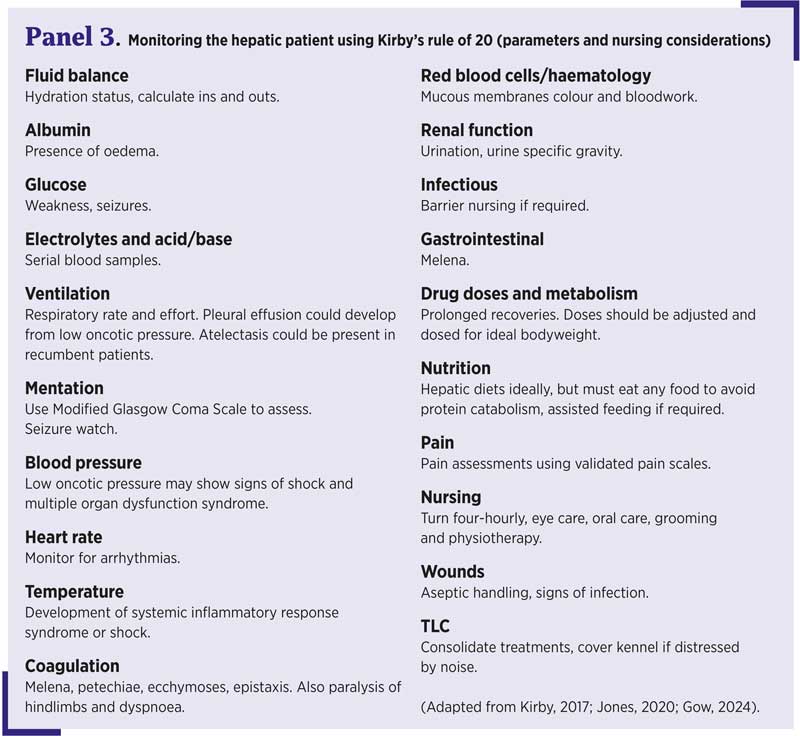
General monitoring of these patients is extremely important to detect any deterioration. Using Kirby’s rule of 20 can help nurses to think about what nursing care to provide and what signs to watch out for (Panel 3).
 Patients should frequently be offered water and walks or easy access to a litter tray, as polyuria and polydipsia are common signs. Good hygiene should be applied to the patient to avoid urine scalding. Patients should be turned every four hours to prevent atelectasis, pressure sores and muscle stiffness, and promote circulation (Monteiro et al, 2022).
Patients should frequently be offered water and walks or easy access to a litter tray, as polyuria and polydipsia are common signs. Good hygiene should be applied to the patient to avoid urine scalding. Patients should be turned every four hours to prevent atelectasis, pressure sores and muscle stiffness, and promote circulation (Monteiro et al, 2022).
Providing pain relief for any patient is vital. Pain assessment can be challenging due to the sensory and emotional components of pain. Validated composite pain scales should be used to help with this. This has been shown to decrease variability and observer bias. Grimace scales have also been shown to be reliable in cats (Gruen et al, 2022).
Abdominal visceral pain can be diffuse and hard to localise, and may be referred to surrounding musculature. Signs of abdominal pain in dogs can include behavioural changes (hiding, aggression, reluctance to move, and disinterest), postural changes (praying position and stretching limbs), vocalisation and anorexia.
Pain relief options for abdominal pain include opioids, ketamine, lidocaine (continuous rate infusions provide a more constant level of analgesia rather than intermittent injections) and intraperitoneal blocks (Monteiro et al, 2022).
Adjunctive non-pharmacological therapies such as acupuncture, massage, anti-emetics and cold or warm compresses are encouraged (Monteiro et al, 2022).
Positive interactions with the patient such as grooming, walking and alleviating fear can also reduce pain.
It is important to measure the resting energy requirement (RER) of any patient with the following calculation:
70 × bodyweight in kilograms0.75
If a patient has been anorexic for a period of time, this daily RER should be gradually built up over a period of four to seven days to prevent re-feeding syndrome (Biorge, 2024).
Debate exists over current feeding guidelines for patients with liver disease. Protein should be reduced to prevent amino acid breakdown to ammonia, but minimal intakes of 2.1g/kg/day and 4g/kg/day for dogs and cats, respectively, should be provided to prevent muscle protein catabolism, which would then lead to further increases in NH3 (Smith, 2018).
Prescription liver diets contain high fat levels and limited copper, but also limited protein, which may not meet the daily requirements (Biorge, 2024). Extra protein such as chicken or cottage cheese can be added.
It is recommended to divide the daily RER into three or more meals throughout the day to enable the remaining healthy hepatocytes to cope with their usual jobs of gluconeogenesis, and glycogen storage (Biorge, 2024).
If a patient consistently eats less than 85 per cent of their daily RER, a feeding tube should be placed (Arbach, 2023).
Potassium supplementation may be required, as vomiting, diarrhoea and polyuria will all lower the amount of potassium in the body.
Zinc supplementation may be beneficial in patients with copper storage disease (Figure 4), as it reduces absorption of copper. Vitamins B, C and K can all be depleted in the liver patient, so are worth supplementing (Biorge, 2024).

Glutathione is an antioxidant that helps to regulate reactive oxygen species from causing damage to cells. In liver disease, these levels can be depleted, so antioxidants such as S-adenosylmethionine, N-acetylcysteine and silymarin (a milk thistle derivative) help to increase these levels (Nixon, 2017).
Nursing the hepatic patient is complex. Many clients will struggle to understand these conditions, so veterinary nurses can play an invaluable role in helping to provide support and education to clients.