13 Jan 2025
Phil Witte looks at a common cause of hindlimb lameness in dogs.
The patella usually tracks in a proximo-distal direction in the femur’s trochlear groove. Patellar luxation is a common cause of hindlimb lameness in dogs, involving displacement of the patella from the groove to a medial or lateral location.
This can occur intermittently (grades 1 and 2), or continuously, with the patella returning to the groove only with digital pressure (grade 3) or not at all (grade 4). Luxation of the patella from the trochlear groove is a mechanical problem with a mechanical surgical solution.
In theatre we have two aims: to increase the resistance to luxation of the patella and to realign the quadriceps mechanism. Standard patellar luxation surgery therefore consists of groove deepening and tibial tuberosity transposition. The application of these techniques has been documented to result in a re-luxation rate of 8 per cent (Arthurs and Langley-Hobbs, 2006).
Distal femoral varus (a bend to the medial) is present in most dogs, but when significant it may contribute to medial luxation of the patella. Some surgeons advocate addressing femoral deformity as a component of surgery to correct patellar luxation in select cases. This article explores patellar luxation with emphasis on the underlying deformities, particularly distal femoral varus, and how we can, and whether we should, correct this deformity.
For the purposes of this article the author refers to medial patellar luxation, as this is more common than lateral patellar luxation.
Reminder of knowledge of quadriceps anatomy. The quadriceps muscles comprise:
Rectus femoris
Origin: ilium just cranial to the acetabulum
Course: passes down the cranial surface of the femur, over the cranial surface of the patella with some attachment to the bone itself and continues as the patellar tendon/straight patellar ligament.
Insertion: tibial tuberosity
Vastus medialis, lateralis and intermedius
Origins: proximal femur and adjacent soft tissues
Course: down the cranial aspect of the femur (craniomedial, cranial and craniolateral, respectively).
Insertions: proximal pole of the patella.
When the patella luxates, it does not do this in isolation. The patella luxates from the trochlear groove alongside medial displacement of the entire quadriceps mechanism. The term “patellar luxation” fails to emphasise this important point.
The quadriceps mechanism consists of the quadriceps muscles (Panel 1), patella and patellar ligament (which should be thought of as the quadriceps tendon of insertion).
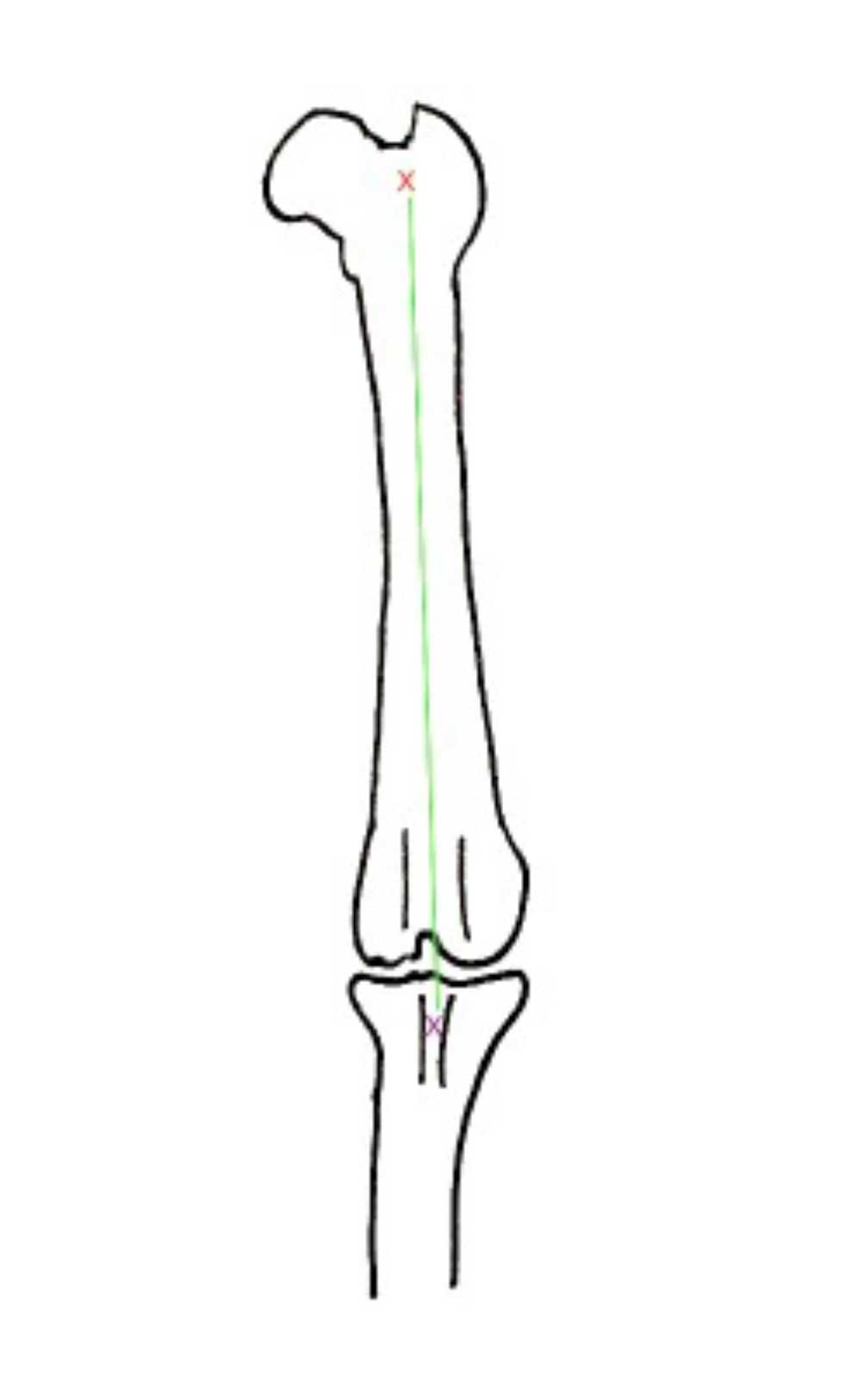
Theoretically, if three points – the origin of the quadriceps muscles (an approximation, since this is the origins of four muscle bellies), the trochlear groove and the tibial tuberosity – are in line then the patella will track within the trochlear groove (Figure 1). Dogs in which those three points are not aligned are at risk of luxation of the quadriceps mechanism, which we term “patellar luxation”.
Deepening the trochlear groove (trochleoplasty) is considered an important component of the surgery for the majority of dogs with patellar luxation (Arthurs and Langley-Hobbs, 2006). We deepen the groove by various techniques to increase the resistance to luxation of the patella from the trochlear groove. However, groove deepening is not enough and realignment of the quadriceps mechanism is widely accepted to be of primary importance.
Realignment of the quadriceps mechanism involves lining up three points: the origin of the quadriceps muscles, the trochlear groove and the tibial tuberosity. In order to achieve this, it is simplest to move the tibial tuberosity.
The tibial tuberosity can be elevated from the proximal tibial diaphysis and metaphysis and transposed laterally. It is typically fixed in place with various combinations of Kirschner wires and tension band wires.
This is a routine technique used frequently to realign the quadriceps mechanism.
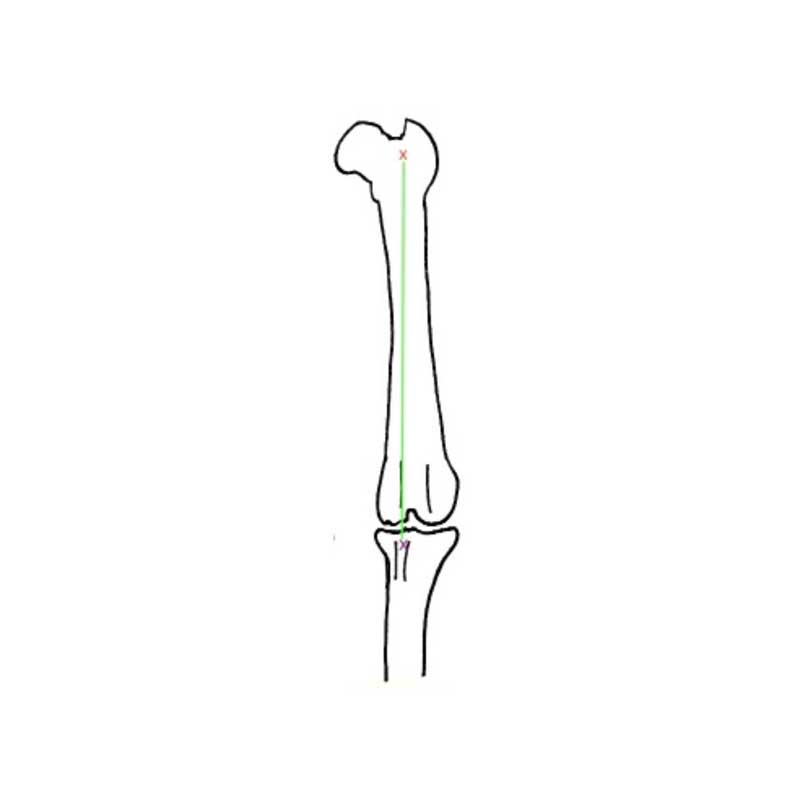
If the tibial tuberosity is medially positioned pre-operatively then realigning the three points by shifting it laterally seems like a reasonable thing to do (Figure 2). But it is worth stopping to ask whether the tibial tuberosity actually is located medially in cases with medial patellar luxation.
A study using computed tomography (CT) to compare the anatomy dogs in three groups – those with no patellar luxation, those with low grade patellar luxation (grade 1 and 2) and those with high grade patellar luxation (grades 3 and 4) – found that tibial tuberosity location was no further medial for dogs in the low grade group than for dogs with no patellar luxation (Yasukawa et al, 2016).
Dogs in the higher grade groups did show greater medialisation of the tibial tuberosity than those without patellar luxation (Yasukawa et al, 2016). Surgeons with experience of patellar luxation surgery are well aware of this disparity between theory and practice, at least for the lower grade cases. Still, we perform tibial tuberosity transposition frequently because it works (frequently).
In the theatre, surgeons will perform a lateral parapatellar arthrotomy, deepen the trochlear groove as they wish then proceed to tibial tuberosity transposition. The extent to which the tibial tuberosity is lateralised is subjective. Theoretically, positioning the tibial tuberosity on the midline should be sufficient. The author will move the tibial tuberosity, place a single Kirschner wire from the tibial tuberosity into the proximal tibial metaphysis and check the stability of the patella by flexing and extending the stifle with internal and external rotation of the tibia.
If the patella is stable at this check-point despite the lateral arthrotomy, then the tibial tuberosity has been moved enough. The surgery is completed as follows: the first Kirschner wire is driven to engage the caudal tibial cortex, a second Kirchner wire is driven distal and parallel to the first, and a figure-of-eight tension band wire is applied over the proximal Kirschner wire and through a more distal bone tunnel to counter the pull from the quadriceps muscles.
If the patella is not stable at this check-point, the tibial tuberosity is moved further laterally until patellar stability is achieved. However, surgeons may be aware that we often move the tibial tuberosity well beyond the midline.
When it comes to tibial tuberosity transposition there are two things that do not add up. Firstly, in agreement with Yasukawa et al (2016), some dogs with medial patellar luxation do not appear to have a medially positioned tibial tuberosity for us to “correct”, and secondly, in some cases we seem to move the tibial tuberosity surprisingly far to the lateral aspect, beyond the midline in order to achieve a stable patella. So, we move the tibial tuberosity in almost all cases, but in a proportion; we are not correcting a deformity (medially positioned tibial tuberosity) and we may even be making one (laterally positioned tibial tuberosity). Something is being missed.
The connection between medial patellar luxation and distal femoral varus deformity was mentioned in an imaging (radiography and computed tomography) study in 2006 (Dudley et al) and highlighted in two case series published in 2007 and 2008 (Swiderski and Palmer; Roch and Gemmill). In both case series, distal femoral varus deformities were corrected as a component of surgery to address medial patellar luxation (Figure 3).
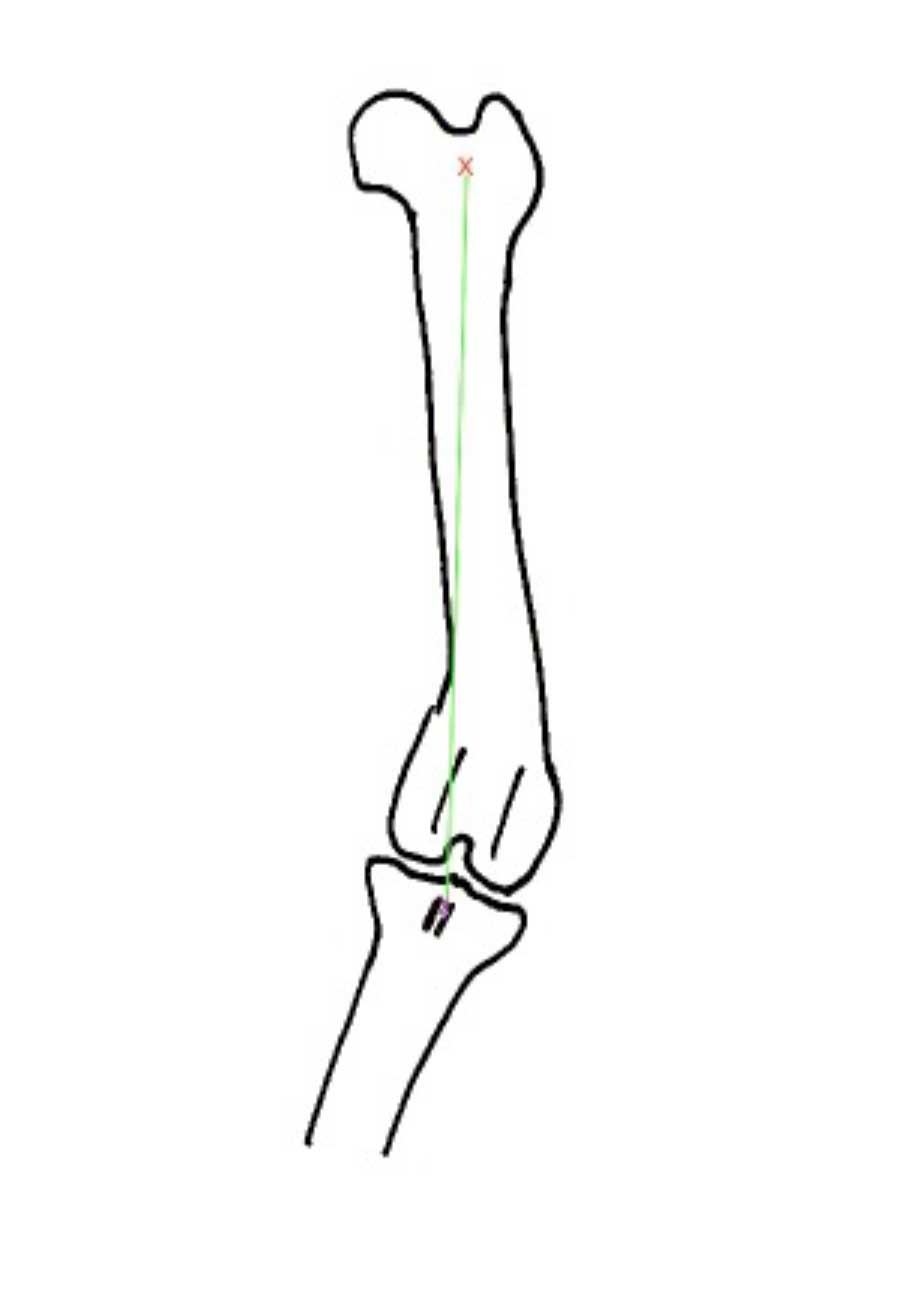
In the Swiderski and Palmer study, 12 dogs (16 stifles) underwent laterally based closing wedge ostectomies to address distal femoral varus. In most cases, other procedures, including groove deepening and tibial tuberosity transposition, were combined with the femoral deformity correction to achieve patellar stabilisation. Selection criteria for distal femoral ostectomy in this series of dogs was a femoral varus of >12° (femoral varus angles ranged from 12° to 29°). This value was selected because it was outside the range of previously reported femoral varus in dogs without patellar luxation (Dudley et al, 2006). In the Roch and Gemmill report, four dogs (five stifles) were described. All dogs had undergone previous (failed) patellar luxation surgeries, and femoral varus angles ranged from 16° to 28°.
A larger retrospective study was published in 2017, covering 55 dogs (66 stifles), which had undergone laterally based femoral closing wedge ostectomies as part of patellar luxation surgery from 2000 to 2012 at three separate centres (Brower et al, 2017).
By the time of publication of this study, methods for measuring femoral varus had changed, following the publication of another paper documenting the normal distribution of various femoral angles in four breeds of dog (Tomlinson et al, 2007). In that study, and thereafter, the term “femoral varus angle” was replaced with a term derived from human limb deformity correction technique, the “anatomical lateral distal femoral angle” (aLDFA).
For Labrador retrievers, golden retrievers, German shepherd dogs and Rottweilers with no stifle pathology, the aLDFA was between 94° and 98°. In other words, normal dogs, at least in these breeds, demonstrated a mild distal femoral varus, so correction of femoral varus angle to 0° (as in the previous case series) would be excessive. As a result of the Tomlinson data, dogs in the Brower study had been selected for distal femoral varus correction by the various surgeons involved if they had an aLDFA greater than 100°-102° (until 2007) or greater than 8°-10° more than the reported breed normal of 94° (after 2007).
The reason for discussing these angles at such length is that it would be convenient to document a cut-off aLDFA above which deformity correction is indicated as part of patellar luxation surgery. More on this later. First, the complicating factor of a study published in 2017 (the same year as the Brower study) documenting successful patellar luxation surgery in a large number of dogs without femoral deformity correction in one single case.
A retrospective study documented 87 canine stifles that underwent surgery for patellar luxation (Perry et al, 2017). Surgeries performed were surgeon-dependent combinations of the standard techniques reported by Arthurs and Langley-Hobbs in 2005 (groove deepening, tibial tuberosity transposition and soft tissue procedures, including release of tissues medial to the patella and tightening of tissues to the lateral aspect).
The outcome parameters were complications. It was shown that there was no correlation between measures of femoral varus angle and any complications. The authors concluded that femoral varus deformity correction is unnecessary to restore patellar stability in dogs.
While transposition of the tibial tuberosity carries complications of its own, femoral deformity correction is more involved and therefore carries a greater risk of complications, not to mention increased cost. Therefore, some reassurance that femoral deformity correction is not necessary might be appealing.
The study by Perry et al revealed success in terms of avoidance of complications where femoral straightening was not performed in any cases, but it did not document the success of surgery in terms of clinical outcome. In fact, there are no assessments using objective outcome measures (kinetics and kinematics) of clinical function for dogs following patellar luxation surgery.
It is pure conjecture, and the author recognises this (and is suitably ashamed), but it is possible that lateralisation of the tibial tuberosity in a case in which distal femoral varus is not corrected may produce a situation in which the direction of travel of the patella is not parallel to the trochlear groove.
Correction of distal femoral varus may theoretically give superior patella-femoral comfort by aligning the direction of travel of the patella and the orientation of the trochlear groove. A study to investigate the functional outcomes for dogs with distal femoral varus that have their varus corrected as a component of their patellar luxation surgery versus those that do not is lacking.
Following the 2007 Tomlinson et al study we know that, for the four breeds of dog in the study at least, the aLDFA for dogs unaffected by patellar luxation ranges from 94° to 98°. The case studies reporting femoral varus deformity correction as a component of patellar luxation surgery indicate an aLDFA greater than 100°-104° has been used (according to anecdote, mostly) to select cases for varus correction (Swiderski and Palmer, 2007; Roch and Gemmill, 2008; Brower et al, 2017).
In a biomechanical study employing a computer model to investigate the influence of femoral varus angle on patellar location, patellar luxation was apparent above an aLDFA of 103° (Lee et al, 2020). So, there appears to be a consensus that femoral deformity correction should be considered where the aLDFA is above 100°-104°. However, things are not so simple. Within their discussion, Brower et al (2017) documented complicating factors such as femoral torsion angle, which can also influence the orientation of the quadriceps mechanism relative to the femoral trochlear groove. Thus, it seems unlikely one specific cut-off aLDFA above which distal femoral deformity correction is always indicated will be established.
As we learn more about hindlimb anatomy in future we may be in a position to establish guidelines more accurately, but these will have to take into account all features with an influence on the quadriceps function. These include femoral neck anteversion angle, femoral torsion, distal femoral varus, trochlear groove depth, femoro-tibial rotation, tibial tuberosity location and more. For each anatomical feature we will need to establish methods for their repeatable quantification, the normal and abnormal ranges for a number of breed types and an understanding of their influence on patellar luxation individually and in combination with the other features. Perhaps it is time the veterinary profession stopped considering patellar luxation the simplest of canine orthopaedic disease. Sometimes it is, but often it is not.
It is intuitive that distal femoral varus effectively medialises the tibial tuberosity with respect to the trochlear groove and therefore has an influence on the likelihood of medial patellar luxation.
This theory is borne out by a biomechanical computer study. Some surgeons employ distal femoral varus correction as a component of patellar luxation surgery where aLDFA measures greater than 100°-104°. Nevertheless, controversy remains regarding whether varus correction is actually required.
Until evidence is available to guide decisions regarding femoral varus correction, surgeons will need to make their own decisions, perhaps taking into account other features of hindlimb anatomy that may influence patellar stability.
The absence of an evidence base is not a situation with which the orthopaedic veterinary community should be satisfied and better understanding of the anatomy is required to develop a definitive algorithm for decision making.