2 Sept 2020
Pet obesity: an ongoing epidemic
Marge Chandler discusses the challenges of dealing with this issue in practice – including assessment, contributing factors, dietary management and owner communication.
Despite continuing research, the pet obesity epidemic continues. Overweight body condition is the most common nutritional disorder in companion animals in many countries, with an estimated 400% increase in the past 25 years in the UK.
Surveys have reported incidence rates of being overweight and obese up to 59% in adult dogs and 63% in adult cats, depending on the country and method of study enrolment1-4.
“Overweight” refers to having excess body fat, while obesity is a bodyweight of 15% to 20% or more above ideal.
Poor recognition of the condition by owners is common. Owners’ underestimation of a pet’s body condition can lead to both the development of obesity and difficulties in addressing it.
The veterinary health care team has a responsibility to help owners with their pet’s obesity, similar to informing them about other medical conditions.
Problems with obesity
Owners should be aware of the disorders that are linked to obesity. Obesity is associated with musculoskeletal problems, compromised immune function and, in cats, increased risk of developing type two diabetes mellitus.
Severely obese dogs or cats are also at greater risk for anaesthetic and surgical complications, heat or exercise intolerance, decreased pulmonary function, dermatological disease, neoplasias such as transitional cell carcinomas, and urogenital disorders such as feline lower urinary tract disease and calcium oxalate urolithiasis.
Obesity likely contributes to clinical signs of tracheal collapse and laryngeal paralysis in dogs, and worsens feline asthma signs.
A lifelong feeding trial in Labrador retrievers showed those on restricted feeding that remained lean lived as much as two-and-a-half years longer than those free-fed. The lean dogs also had a delay in the onset of signs of chronic diseases such as arthritis5.
Obese dogs that lost weight showed improvement in quality of life, including vitality, emotional disturbance and signs of pain6.
Assessing body condition
A number of techniques for assessing body condition exist, including deuterium oxide dilution, bioelectrical impedance, biometrics, ultrasound, dual‑energy x-ray absorptiometry (DEXA), and body condition scoring (BCS). Of these, BCS along with bodyweight – and changes in bodyweight – are the most useful in practice.
A BCS is a subjective assessment of body composition. The nine-point BCS system was validated for dogs and cats using DEXA, and provides a reasonable estimate of body fat7,8 (Figures 1 and 2).


Using BCS charts and showing the owner how to do a score can be useful in demonstrating his or her pet’s overweight condition. Ideal BCS in dogs is 4/9 to 5/9, depending on breed, and 5/9 for cats.
For some cats, especially older cats, a BCS of 6/9 is acceptable or preferable9.
The BCS systems can be used to estimate percentage of body fat (Table 1).
| Table 1. Estimated body fat percentages compared to body condition scores | |
|---|---|
| Nine-point scale | Percentage body fat |
| 1 | Lower than 5 |
| 2 | 6 to 9 |
| 3 | 10 to 14 |
| 4 | 15 to 19 |
| 5 | 20 to 24 |
| 6 | 25 to 29 |
| 7 | 30 to 34 |
| 8 | 35 to 39 |
| 9 | 40 to 45 |
Aetiology of obesity
The aetiology of pet obesity is multifactorial, and includes the pet’s physiology, diet and feeding behaviours of the owner.
While disorders such as hypothyroidism can contribute to weight gain, the underlying cause in most cases is an imbalance between energy intake and expenditure. This is a simplistic version as other factors contribute and the psychological aspects of feeding pets are substantial.
Factors that contribute to obesity can be classified as endogenous or exogenous.
Endogenous factors
Endogenous factors include breed, age, sex, neutering status and genetic predisposition. Neutering has been shown to increase risk of weight gain in dogs and cats7,10.
Many genes influence the tendency to gain weight, but relatively little is known regarding the degree of “gene-environment interactions”; the complex interplay between genetic make‑up and environmental factors, including diet.
A mutation in the proopiomelanocortin (POMC) gene has been found in some Labrador retrievers and flat-coated retrievers. The mutation in this gene causes these dogs to have an increased appetite and decreased satiety. For each copy of the mutation, a dog will be, on average, 1.9kg heavier than dogs without the POMC mutation.
About one in four (23%) of UK Labrador retrievers carries at least one copy of the mutation. The mutation is significantly more common in Labrador retrievers selected to become assistance dogs than pets, perhaps because their food motivation makes them easier to train.
This mutation is also present in flat-coated retrievers, where about two‑thirds carry at least one copy of this mutation. It could also occur in cross-bred dogs, with Labrador retrievers or flat‑coated retrievers in their genetic make-up11,12.
Epigenetic changes affect how genes are expressed, and some can be modified by diet (nutrigenomics) and exercise13. So, while DNA cannot be changed, the expression of genes and the effects they have can be modified.
Having “obesity genes” does not mean an individual is fated to be obese, but it does mean greater care will likely be needed to prevent obesity.
Exogenous factors
Exogenous obesity risk factors include diet composition and palatability, feeding management, activity level (for example, being an indoor‑only cat) and a fast growth rate4,14,15.
Pet food label feeding recommendations are based on energy requirements of an average animal in normal body condition; however, great variety exists in animals’ individual requirements.
The label directions also do not take into account extra food, treats, snacks and food given to administer medications. Feeding treats and human foods are a risk factor for obesity in many studies4.
Dietary management
Many pet foods are developed for palatability, which can lead to overconsumption. Owners often evaluate a food based on how enthusiastically their pet eats it.
High-fat diets, which are often very palatable and have an increased calorie density, contribute to excess calorie consumption. They may also provide less satiety than a higher‑protein, higher‑fibre diet.
A weight loss programme must include a good diet history, including the diet brand, type, flavour, frequency and timing of feeding, method of feeding (bowls versus feeding toys), as well as all extra types of food. A diet history sheet is useful and the owner can be asked to fill this in prior to the consultation; possibly at home where they may be better able to reflect on the feeding programme.
The nutritional assessment should also include a current weight (ideally compared to previous weights on a chart), BCS and muscle condition score. Be careful having an owner select a picture from a BCS chart as he or she will often choose a lower BCS than his or her pet has.
Several recommendations exist for calorie intake for weight loss, including feeding at resting energy requirements (RER) for the ideal weight (iRER), or feeding at 80% of iRER (RER = 70 × bodyweight in kg0.75).
Feeding at 80% of iRER can result in a drastic cut of food intake for some pets. A programme should sufficiently restrict calories to produce weight loss without being so severe that the pet is chronically hungry and the owner feels guilty about enforcing the diet.
Severe restriction and rapid weight loss may also be more likely to result in more loss of lean body mass and in regaining weight after calorie restriction.
Many owners request a programme of feeding less of the existing diet.
Therapeutic diets for weight loss have the advantage of lower calorie and fat intake with less decrease in food intake, as well as higher concentrations of other nutrients. Feeding less of a maintenance diet can result in nutrient deficiencies16.
Many therapeutic diets also include nutrients that benefit the pet’s satiety and maintenance of lean body mass, such as increased fibre, protein and L-carnitine. They may also include nutrients such as omega-3 fatty acids to support mobility.
While most commercial weight loss products can be used successfully, a large variability exists in caloric density. “Lite” diets contain only about 10% fewer calories than the “non‑lite” version of the same food and are often not useful for weight loss.
The veterinary health care team must provide information about how much to feed and how to measure the food, ideally weighing rather than using a cup (Figure 3).

Other topics to discuss include how to deal with treats and how much exercise the pet should get. The team should show compassion for setbacks – for example, a visiting relative gives the pet extra food.
Monitoring food intake at home – for example, a chart with what the pet has been fed when – can help, especially when multiple people in the household may be feeding the pet17.
Recommendations for treats and snacks vary from not allowing any (possibly impractical) to calculating about 10% of the calories allowed from low‑calorie treats. Putting the day’s treat allowance in a jar (in the fridge if necessary) can help limit the number given.
Using interactive pet feeders can provide some environmental enrichment and slow the rate of eating (Figure 4). Frequent feeding may also help in some pets – especially cats. Cats’ normal feeding pattern is multiple small meals per day.

Exercise is encouraged for most pets, although joint, heart or other disorders may limit the amount possible. Exercise – including walks, play and environmental enrichment – can help maintain lean body mass. It is difficult to lose weight with moderately increased exercise alone, although it does help maintain weight.
The goal for weight loss is 1% to 2% of bodyweight per week; however, a more realistic goal for many pets is as low as 0.5% to 0.8% per week.
Slow weight loss may help preserve lean body mass – especially in cats. Weighing should be done every two weeks initially and the diet adjusted as needed.
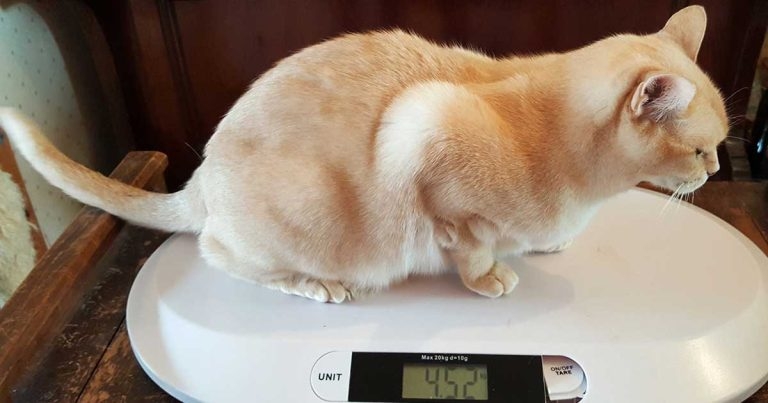
Monitoring the bodyweight and BCS in the clinic is helpful as it provides a chance to discuss any problems the owner is having with the weight loss programme, although telephone calls can be used where clinic visits aren’t possible or practical. A (human) baby scale (for cats and small dogs) or pet scale can provide home monitoring (Figure 5).

Communicating with owners
A recent report showed veterinarians and veterinary students felt more blame, frustration and disgust towards obese dogs and obese owners compared to lean dogs and lean owners18.
Obese owners of overweight dogs were perceived as causing their dog’s obesity, while lean owners were thought to be responsible for their dogs being lean.
In human medicine, the bias against obese people results in poorer provision of health care.
The attitude of the veterinary health care team towards owners of overweight pets – and the pets themselves – needs to be supportive, rather than judgemental, to gain trust and cooperation. It has been recommended to avoid the use of negative terms – such as “fat”, “plump”, “chubby”, or “chunky” – and to treat the condition as a disease19, although minimising the problem (she’s “not that bad” or is “just cuddly”) should also be avoided.
It is also important to differentiate between the pet’s “lovableness” and having the disease of obesity. Many owners of overweight pets anthropomorphise or “humanise” them so that feeding and giving treats is a way of bonding and showing love. The approach should be a shared concern for the pet’s health and happiness, and a joint approach to the solution20.
Three steps to effectively managing obese patients are:
- the owner’s recognition of obesity and establishing client commitment
- the development of a programme that meets the needs of the pet and owner
- communication and follow-up with the practitioner
Components usually included in weight loss programmes are diet, exercise and behaviour modification.
Owners may not recognise or acknowledge that their pet is overweight and resist trying a weight loss programme. This stage of lack of awareness is sometimes termed “pre‑contemplation”. For these owners, continue to tactfully discuss the pet’s weight gain, and the risks to health and happiness. Use the BCS and weight charts at each appointment. Charting weight may provide a better graphic demonstration of changes than numbers. This may transition the owner to a stage of awareness, which is the step before definitively deciding to make a change.
Once the owner has decided to try a weight management programme, the next step is setting defined, measurable goals with the owner for behaviour changes – for example, three walks instead of two, changing to a specific number of low-calorie treats and for weight loss outcomes, such as 0.5% bodyweight loss per week.
Weight loss programmes can be very difficult for the owner. It is important to have the owner identify where problems or challenges may occur – for example, a neighbour who feeds extra food or a lean cat and a fat one in the same household.
The owner may have concerns about making the pet unhappy or hungry, or about the costs of the diet. These problems should be discussed at the initial and subsequent appointments, and solutions worked out with the owner.
What goes wrong with weight loss programmes?
Losing weight is much more difficult than avoiding being overweight. The homeostatic regulation of bodyweight and appetite are generally geared more to “protecting” animals and people from weight loss than from weight gain.
Diet-induced weight loss results in physiological changes that encourage weight regain, such as alterations in energy expenditure and appetite regulation.
A long-term study in dogs enrolled in a weight management clinic incorporating follow-up strategies showed about half of them regained weight21. Dogs and cats in less structured programmes are probably more likely to regain lost weight.
After weight loss, maintenance energy requirements (MERs) decrease to less than they were prior to weight gain. In research beagles that gained, lost then subsequently gained weight, less time and fewer calories were required to reinduce the same degree of obesity compared with the initial obesity induction22. Food efficiency was increased during the second weight gain period.
Pet-owned dogs, in another study, also showed a post‑weight loss MER of only 10% more than that required for the weight loss. Calorie restriction during weight loss in cats results in a decrease in energy expenditure that is maintained after weight regain23.
To date, the only intervention proven to improve quality of life and concurrently extend lifespan is caloric restriction and maintenance of a lean BCS. Weight and body condition should be discussed at every appointment to stop unwanted weight gain early.
The development of obesity has numerous adverse effects on a pet’s health and longevity, but implementation of a weight loss programme, and maintenance of a good body condition in dogs and cats, has continued to be a challenge for veterinary surgeons, pets and owners.
A primary goal of the veterinary profession should be to prevent pet obesity – as prevention is definitely easier than cure.
