20 Jul 2021
Sustaining management of OA
Stuart Carmichael looks at steps practices can take to provide lifelong care for these patients, as well as new developments to facilitate this.

Image © Life in Pixels / Adobe Stock
OA is a lifelong disease. Numerous reasons and strong evidence exists that patients with OA benefit from a sustained management programme that extends well beyond the first four to six weeks, and that pet owners value and appreciate such an approach.
When a joint is affected by OA, a sequence of inflammatory events produce clinical signs at the same time as a structural deterioration is taking place within and around the joint.
Successful management aims to understand the reason for clinical signs at the same time as understanding the structural changes in the joint at presentation, and use this information to create a strategic plan to deal with the problem.
The objective is to help the affected joint contain the problem for as long as possible. In turn, this allows the patient to cope with the clinical signs (Panel 1).
- Identifying episodes of pain quickly and acting to suppress.
- Identifying chronic pain, and developing strategies to modify, control and eventually abolish it.
- Adopt strategies to limit the structural progression of the disease.
- Encourage continued mobility of affected joints in a controlled and beneficial fashion.
- Preventing obesity and providing a good, balanced diet.
- Limit challenges provided by the environment that can cause unnecessary pain, avoidance and loss of confidence.
- Maintain facilities that are necessary for the patient to successfully compensate for some of the issues created by the disease, such as proprioceptive skills.
- Continually monitor the clinical situation to recognise early departures from normality or early evidence of pain.
- Provide continual support and encouragement for the owners.
A diseased joint can continue to function well if we optimise the other factors influencing the clinical impact of OA. Sustained management and monitoring can identify early shifts in clinical problem and adjust management appropriately.
Evidence already exists for benefits of long-term medical management from patients on NSAID treatment of longer than four weeks that showed improved outcomes compared to patients treated for less than four weeks1.
OA is also a lifestyle disease – and controlling factors such as bodyweight and exercise are key features of sustained management.
What makes this difficult to achieve?
Many reasons exist for why this approach is not commonplace.
One major barrier is based on a basic misunderstanding of OA and its progressive nature. A diagnosis of OA is often made without any differentiation of grade of OA, joint or joints involved and clinical problems identified, leading to a generic “one fits all” OA treatment package used in all patients.
We seem more engaged by the specifics of what we use to treat in the short term, rather than introducing and developing more fluid long‑term management solutions
Another major barrier is that even with a full understanding of what is needed and good intentions, it is difficult to actually deliver this type of programme.
Typically, the main arguments put forward against sustained management are commercial (“clients will not pay for this”) and operational, as this is perceived as being time‑consuming in a practice environment where time is in very short supply.
This ignores the basic reality, which most practices fail to appreciate or acknowledge, that they need to change their approach and system to achieve this – and that owners do really want sustained management2.
Currently, it is also difficult to establish if a patient is actually improving over the long timespan of the disease without having a planned and reliable measurement solution.
Convincing owners that their pet has a genuine painful problem can also be an issue. More accessible information for owners from the practice – and evidence of improvement – would increase demand for management and make long‑term management easier to implement.
So, where is the motivation for introducing an involved staged programme when no one can be sure if it is working or making a difference?
How do we change this? A different approach to OA
OA is the main cause of chronic pain and reduced quality of life in our pet population.
With such a high percentage of cases within a practice affected by OA and the increasing numbers of older dogs in the population that have a higher likelihood of having serious clinical problems, including persistent pain, it is difficult to understand why this is not a priority.
Add the change in attitude of owners who expect a more complete and consistent service, and it is difficult to understand why practices are resisting this change.
So, where do we start?
Taking simple steps
1. Change the approach – make OA more interesting:
Break down the presenting problem to understand the pain and the structural stage of the disease.
Use this information to target key objectives that will impact the problem.
View the progression as a journey where management targets will change over time, and plan for this.
Measure if preset objectives have been met before setting new targets.
Communicate this clearly to the owner.
Believe that this will really make a difference.
2. Change the practice system – make sustained management possible:
Have a vet-led approach, rather than a vet-centred approach, and develop a practice team to operate an OA clinic.
Have the same members of the practice dedicated to this area to give continuity.
Have dedicated slots set aside for OA clinics with appropriate length of consultations.
Have a clear method of recording clinical signs and management practices over time.
Have a method of proactively monitoring cases.
Adopt a system that brings all of these elements together.
Make use of OA support and resource sites that provide information and training about OA for practice members and clients, such as the Veterinary OA Alliance and Canine Arthritis Management.

New developments to facilitate long‑term care
Therapeutic new wave
New pharmacological options offering longer‑term pain relief from a single administration make longer‑term treatment plans more accessible by making things simpler for the owner – and, therefore, encourage better compliance.
New developments – such as anti-nerve growth factor injection3, which is delivered monthly – offer options when assembling a multimodal plan.
Similarly, the increasing numbers of new intra-articular therapies have, as one of their main attractions, claims for longer‑term suppression of signs over prolonged periods after a single treatment.
These developments can encourage longer‑term management by making key components of the package plan much simpler to deliver, allowing focus on the other support and lifestyle elements of the plan. It is important that these other elements are not neglected.
Measuring, monitoring and educating
Clinical metrology instruments4-7 are very useful methods of assessing chronic OA by capturing the owners’ perception of problems over an entire period of care, rather than just at the time of consultation. They can also act to guide owners to understand what things are important in the clinical development and, therefore, grant a level of owner control.
Owner involvement and empowerment is an essential component of effective long‑term care, with pet owners working with – and as part of – the OA care team. They can be educated to better understand the problem, to react when they see deterioration and to appreciate genuine improvement. They can also be instructed on how to manage mobility and exercise better, and understand the importance of diet.
This empowerment – coupled with improved knowledge delivered from the practice team, plus improved measurement and communication – builds trust in the plans essential for compliance over the course of the disease.
Repeated assessments can be used to monitor longer‑term progress.
Digital health care
A key component in achieving this whole objective is the delivery of information, communication and having a good monitoring or measurement system that is transparent to the owner. Aim OA8 is one example of a digital management system designed for OA.
Introducing reliable measurement of the impact of the disease over time encourages longer‑term commitment, and has been missing for both owners and the care team up until now.
Digital health care affords a solution to assist these aims. Digital systems are perfect for storing the results of repeat examinations and assessments. They can also analyse and display key measurements in a manner that helps identify the true progression of the clinical problem and the impact of interventions (Panel 2; Figure 1).
- Digital recording and planning system.
- Remote consultation/monitoring facility.
- Video capture system.
- Push text messages to owners as reminders.
- Assessment system that owners can perform at home.
- Asynchronous text message communication facility.
- Care team digital communication system and shared clinical record (including conference and video capture system).
- Instructional webinars for owners.
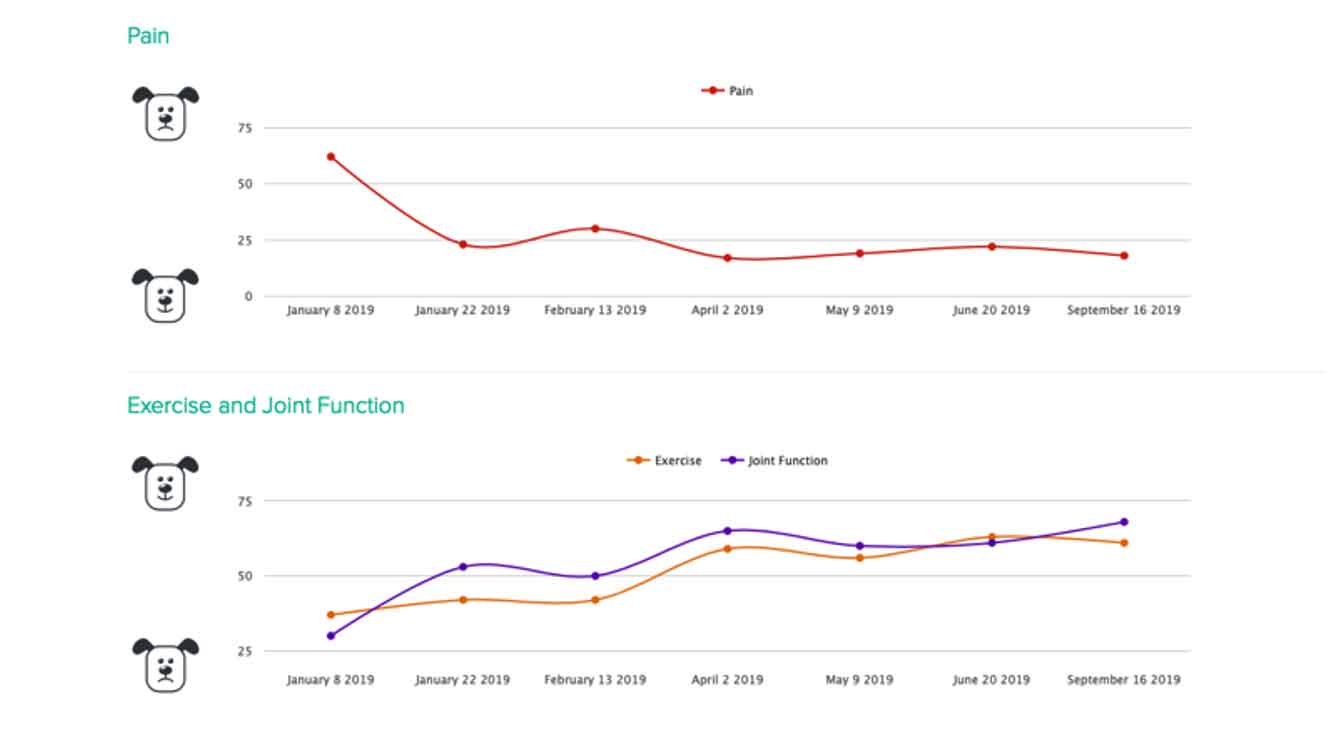
This helps to better understand progress over a longer time period and gives care teams more confidence in using much more long‑term management.
Long‑term management guidelines – the four Cs
When developing a strategy for effective long-term management of OA cases – and assembling the team, resources and system to deliver this successfully – it is important to consider the four Cs as guidelines (Table 1).
| Table 1. Four Cs for long-term management | |
|---|---|
| Collaboration | Using different skill sets within the practice – and between the practice members and therapists – will broaden and enhance the care that can be delivered. It is mandatory that all members agree to cooperate and work together on a common plan. |
| Coordination | Someone needs to coordinate all these elements and effectively lead the management plan, ensuring the objectives of the common plan are being delivered. |
| Consistency | If the elements described above are achieved then the management plan will demonstrate consistency, which will build owner trust as well as deliver better care. |
| Communication | This is the oil that ensures the whole machine can work. Cloud-based digital management systems can improve communication and deliver consistency by allowing sharing of the management plan instantly between the different members of the care team. This ensures common targets are set, and that they are constantly being measured and monitored for success. |
A vet-led team should involve other members of the practice and include therapists that the practice has developed a relationship with, as well as the pet owners themselves. Suddenly, a very important team management demand exists to deliver great patient management and customer service.
Using some kind of digital hub that all team members have access to, and can contribute to, seems like the best way the remove many of the operational barriers to long‑term coordinated care of OA – allowing the team’s energy to be focused on improving the life of the patient.
References
- Innes JF, Clayton J and Lascelles BDX (2010). Review of the safety and efficacy of long-term NSAID use in the treatment of canine osteoarthritis, Vet Rec 168(8): 226-230.
- Belshaw Z, Robinson NJ, Dean RS and Brennan ML (2018). “I always feel as if I have to rush…” pet owner and small animal veterinary surgeons’ reflections on time during preventative healthcare consultations in the United Kingdom, Vet Sci 5(1): 20.
- Enomoto M, Mantyh PW, Murrell J, Innes JF and Lascelles BDX (2018). Anti-nerve growth factor monoclonal antibodies for the control of pain in dogs and cats, Vet Rec 184(1): 23.
- Brown DC, Boston RC, Coyne JC and Farrar JT (2008). Ability of the Canine Brief Pain Inventory to detect response to treatment in dogs with osteoarthritis, J Am Vet Med Assoc 233(8): 1,278-1,283.
- Hielm-Björkman AK, Kuusela E, Liman A, Markkola A, Saarto E, Huttunen P, Leppäluoto J, Tulamo R‑M and Raekallio M (2003). Evaluation of methods for assessment of pain associated with chronic osteoarthritis in dogs, J Am Vet Med Assoc 222(11): 1,552-1,558.
- Reid J, Wright A, Gober M, Nolan AM, Noble C and Scott EM (2018). Measuring chronic pain in osteoarthritic dogs treated long‑term with carprofen, through its impact on health-related quality of life, Vet Comp Orthop Traumatol 31(S 01): A1-A6
- Walton MB, Cowderoy E, Lascelles D and Innes JF (2013). Evaluation of construct and criterion validity for the ‘Liverpool Osteoarthritis in Dogs’ (LOAD) clinical metrology instrument and comparison to two other instruments, PLOS One 8(3): e58125.
- Aim OA Veterinary Monitoring (www.aim-oa.com).
