16 Nov 2021
Luisa De Risio describes the approach to these cases – including establishing if patients are having a seizure, causes and treatment.

Image © #CRTVTY / Adobe Stock
The prevalence of epilepsy in cats has been estimated as 0.16% (one-year prevalence of recurrent seizures) in primary care in the UK1, and between 2.1% and 3.5% in referral hospital populations2,3.
Epilepsy is a neurological disorder that is defined by recurrent epileptic seizures (two or more at least 24 hours apart) that are not caused by toxin exposure or a metabolic disorder4.
A reactive seizure is a seizure occurring as a natural response from the normal brain to a transient disturbance in function (metabolic or toxic in nature), which is reversible when the disturbance is rectified4.
For brevity, in the following text, the term seizure will be used to refer to both epileptic seizure (for example, secondary to idiopathic, structural or unknown epilepsy) and reactive seizure.
Similarly, to the canine seizure patient, the approach to the feline seizure patient should be systematic and involve the following steps:
Knowledge of seizure phenomenology, and obtaining a detailed description of the event (including what the cat was doing before and after the episode), can help to discriminate between seizures and other paroxysms (such as vestibular attacks, episodes of pain and cardiovascular disorders).
Reviewing video recording of the episode can provide valuable semiological details that may be unrecognised and, therefore, unreported by the cat’s owner.
The phases associated with a seizure include:
The preictal phase is the time before the ictal phase, during which cats may display unusual behaviours that owners can identify as indicator of a forthcoming ictal phase. These behaviours may include hiding or attention seeking, or aggression and vomiting.
The preictal phase may last for seconds or hours and may go unrecognised, especially when it is characterised by hiding.
The ictal phase is characterised by one or more of the following signs:
Assessment of the presence or absence of consciousness during the ictal phase may be difficult, particularly in cats.
Focal seizures are characterised by lateralised and/or regional motor signs, such as rhythmic blinking, twitching of facial musculature (Video 1) or repeated rhythmic jerks of one extremity, and/or transient and stereotypic abnormal behaviours with or without concurrent autonomic signs and altered consciousness4.
Generalised seizures are characterised by involvement of both sides of the body, frequently with concurrent autonomic signs and altered consciousness (Video 2). Generalised seizures may evolve from a focal seizure or involve the entire body from the start of the ictus.
In cats (as in dogs) generalised seizures predominantly present as tonic, clonic or tonic‑clonic seizures.
Myoclonic seizures are characterised by sudden and brief involuntary contractions of a muscle or muscle group. Consciousness is often normal.
The ictal phenomenology is typically consistent between seizures, although it can evolve over time (for example, focal seizure may generalise).
Resolution of the ictus leads to the postictal phase, in which neuronal “resetting” occurs5. During this phase, the cat may be disoriented, have behavioural abnormalities such as repetitive vocalisation, compulsive locomotion, ataxia, be hungry or thirsty, express a need to urinate, defecate or appear exhausted, and sleep for a long period of time. Postictal blindness or aggression may also occur. The postictal phase may last seconds to days.
Seizures generally occur at rest or on waking up; however, sometimes seizures can occur after a specific stimulus.
Reflex seizures are defined as seizures that objectively and consistently occur immediately after a specific, identifiable stimulus4. Such stimuli may include visual (such as light flashes) or auditory (such as certain sounds) stimuli4,5.
A reflex seizure may manifest as a generalised or focal seizure. A particular type of reflex seizures, often occurring after high‑pitched sounds, has been reported in cats in the UK and have been referred to as feline audiogenic reflex seizures (FARS)6.
Sound stimuli identified to evoke FARS included:
Median age at FARS onset was 15 years.
Myoclonic seizures (generally affecting most of the body and without apparent loss of consciousness) have been reported as one of the characteristic signs of FARS, frequently occurring prior to generalised tonic‑clonic seizures6. Levetiracetam has been reported as effective and well‑tolerated treatment for FARS7.
Another peculiar seizure phenotype in cats are the so‑called “orofacial seizures” characterised by arrest in a sitting position, profuse salivation, facial twitches, vocalisation (most often howling and hissing) and mydriasis. These seizures can progress to generalised seizures with loss of consciousness and involuntary urination8,9.
These cats often present with bilateral lesions in the hippocampus and in the piriform lobe (Figure 1; visible on MRI and postmortem examination), hence the condition has been referred to as feline hippocampal necrosis or sclerosis8,9.
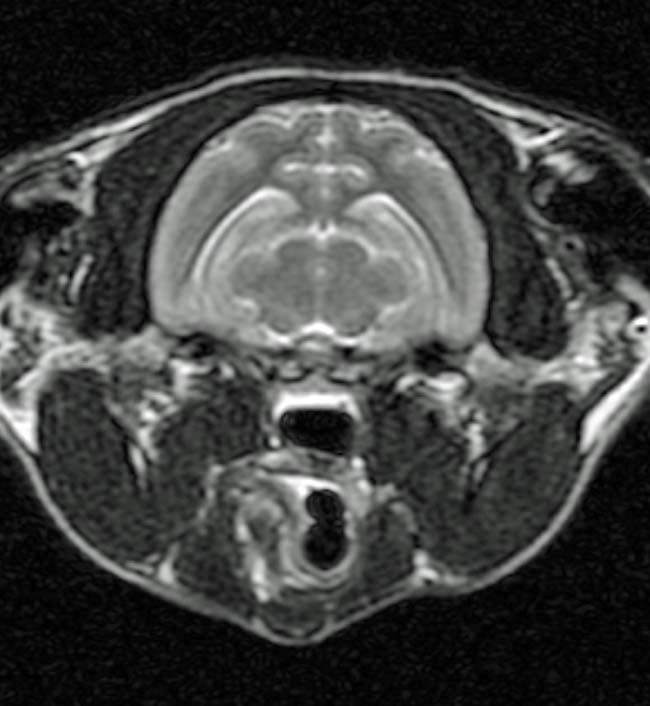
Debate is ongoing in the veterinary literature on whether the lesions in the hippocampus and in the piriform lobe are the cause of, or secondary to, this type of seizures in cats.
Seizures can occur as single events or as cluster seizures (two or more seizures within a 24-hour period with full recovery of consciousness between seizures) or status epilepticus (a seizure lasting longer than five minutes, or two or more discrete epileptic seizures between which incomplete recovery of consciousness occurs).
Transient neurogenic urinary retention has been reported in four cats following severe cluster seizures10. Optimisation of antiepileptic treatment helped to prevent further cluster seizures. All cats recovered normal micturition (following adequate bladder management) within four weeks of the final cluster of seizures.
Urinary retention should be considered a potential postictal deficit requiring prompt recognition, and treatment to avoid urinary tract infection and detrusor muscle atony.
As part of the investigation of the seizure patient, it is important to establish the time of seizure onset. This can be particularly challenging in cats.
An outdoor cat, or a cat that spends most of the day unsupervised and/or tends to hide in the preictal phase, may have suffered unwitnessed seizures in addition to the most recent one/s that resulted in the veterinary consultation. Specific questions have to be asked to identify possible toxin exposure (acute and chronic).
Based on the cat’s age at seizure onset, a detailed medical history and description of the seizure phenomenology, and a thorough physical and neurological examination, the clinician can develop the differential diagnosis list. Detailed information on how to perform and interpret the neurological examination in the seizure patient can be found elsewhere11.
Diagnostic investigations should include haematology, comprehensive serum biochemistry (including electrolytes and bile acids) and urinalysis. Depending on the index of suspicion (based on signalment, medical history and clinical examination), infectious disease and thyroid function testing may be indicated.
MRI scans of the brain should be considered in any cat presenting with a history of seizures following exclusion of toxin exposure and metabolic abnormalities as the underlying seizure aetiology. MRI is superior to CT for optimal visualisation of intracranial structures.
CSF collection and analysis should be performed following the MRI any time infectious diseases and certain neoplasia (such as lymphoma) are suspected.
Imaging of the thorax and abdomen (such as radiography, ultrasound or CT) should be performed when systemic infectious or neoplastic disease is suspected. Abdominal ultrasound is also indicated when a portosystemic shunt, hepatic or renal disease is suspected as the underlying seizure aetiology.
Commonly reported aetiologies of feline reactive seizures include hepatic encephalopathy, severe uraemia with end‑stage renal disease, hypoglycaemia (generally secondary to insulin overdose), hypertension, polycythaemia, and intoxication with permethrin or inhibitors of acetylcholinesterase. Systemic and neurological signs are often present in cats with reactive seizures.
Structural epilepsy refers to epileptic seizures that are provoked by intracranial/cerebral pathology4 and may be caused by neoplastic (such as meningioma; Figure 2 and lymphoma), inflammatory, infectious, traumatic, vascular or neurodegenerative disorders.
In a recent study, pedigree status (being a pedigree cat versus non-pedigree), older age at seizure onset (older than seven years of age), abnormal neurological examination and ictal vocalisation were associated with a diagnosis of structural epilepsy rather than idiopathic epilepsy12.
A multicentre cross‑sectional study – which included 188 cats with normal interictal physical and neurological examinations, and without significant abnormalities on haematology and serum biochemistry analysis – found significant MRI abnormalities (for example, structural epilepsy) were detected significantly more often in cats six years of age at seizure onset than in cats aged one to six years13. The risk of structural epilepsy increased by 14% per additional year of age at seizure onset13.
No consensus currently exists on the diagnostic criteria, including age range at seizure onset, for idiopathic epilepsy in cats.
Feline idiopathic epilepsy (also known as epilepsy of unknown origin) could be defined as two or more epileptic seizures at least 24 hours apart in which the nature of the underlying cause is as yet unknown and with no indication of structural epilepsy or reactive seizures4.
The diagnosis is based on an unremarkable neurological examination and exclusion of other seizure aetiologies by extensive diagnostic investigations (for example, haematology, comprehensive serum biochemistry, urinalysis, MRI of the brain and CSF analysis).
Treatment depends on seizure aetiology. Any time an underlying aetiology is suspected, this should be identified and treated (whenever this is possible).
In cats with idiopathic and structural epilepsy, long‑term antiepileptic drugs are often indicated. No consensus exists on optimal time for antiepileptic drugs (AED) treatment initiation in cats. In dogs with idiopathic epilepsy, AED treatment is recommended when a dog has had two or more epileptic seizures within a six‑month period, status epilepticus or cluster seizures, or severe postictal signs. AED treatment is also recommended in dogs with structural epilepsy and post-traumatic epilepsy.
These guidelines for dogs could be implemented in cats at least until feline epilepsy-specific guidelines are published.
An evidence-based assessment of the published data on AEDs’ efficacy and safety for feline epilepsy suggests that, currently, phenobarbital is the first-choice AED for epileptic cats, followed by levetiracetam and imepitoin14.
The starting dosage for phenobarbital is 1.5mg/kg to 2.5mg/kg every 12 hours. The oral dosage is subsequently tailored to the individual patient’s needs based on an accurate epileptic seizure diary, serum phenobarbital concentration monitoring, as well as occurrence and degree of antiepileptics.
The levetiracetam starting dose is 20mg/kg every 12 hours.
Additional information on AED dosage, adverse effects and treatment monitoring can be found elsewhere11,14,15.