28 Mar 2016
Antonia Mavropoulou summarises the clinical signs of this condition in cats and dogs before outlining common treatment medications and an approximate dosage for each.

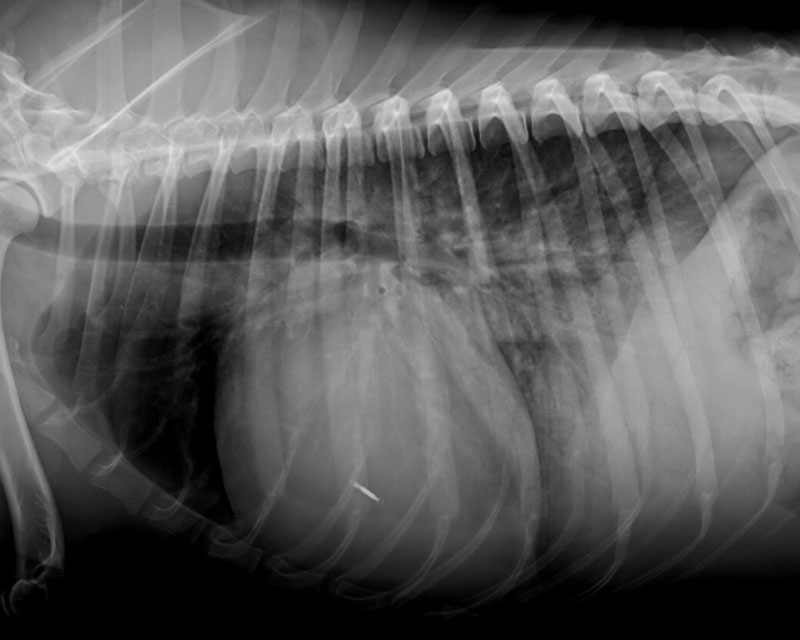
Figure 1a. Lateral radiograph of a dog with generalised cardiomegaly, vessel enlargement and diffuse lung opacity, particularly in the more caudal and ventral lung fields where air bronchograms are visible. These radiographic signs suggest heart disease and cardiogenic pulmonary oedema.
Congestive heart failure (CHF) is a common consequence of severe heart disease and is frequently encountered in clinical practice. Depending on the severity of clinical signs, treatment may require acute (hospital-based) or chronic (home-based) management.
This article focuses on the various cardiac medications available and commonly used to treat CHF in dogs and cats. Drug dosages are included as a guideline only. The reader is strongly encouraged to consult and follow the manufacturer instructions and the drug formulary indications.
Congestive heart failure (CHF) is a complex clinical syndrome triggered by any structural or functional cardiac disease that impairs the ability of the heart to receive or eject blood (diastolic and systolic dysfunction, respectively).
Compensatory mechanisms to help maintain cardiac output, adequate arterial blood pressure and perfusion of critical organs (for example, brain, heart or lungs) are mediated by neural and hormonal messengers, such as catecholamines, renin, angiotensin and aldosterone.
These neurohormonal mechanisms have beneficial short-term effects and result in increased heart rate and cardiac contractility, peripheral vasoconstriction and fluid and sodium retention by the kidneys. However, in the long-term, they result in excessive fluid retention, elevated pressure within the venous circulation and accumulation of fluid in the extracellular space (pulmonary oedema with or without pleural effusion [in cats] in case of left-sided CHF or pleural/peritoneal/pericardial effusion in case of right-sided CHF)1.
Clinical signs depend on the site of fluid accumulation and may include compromised respiratory function (dyspnoea, tachypnoea or increased respiratory effort), exercise intolerance, lethargy, weakness or collapse, abdominal distension, anorexia and diarrhoea2,3. A presumptive diagnosis is usually made on the patient’s clinical signs, signalment, history and physical examination findings.
Thoracic radiography is a readily available confirmatory test and usually shows cardiomegaly, venous congestion and pleural effusion or pulmonary oedema3 (Figure 1).

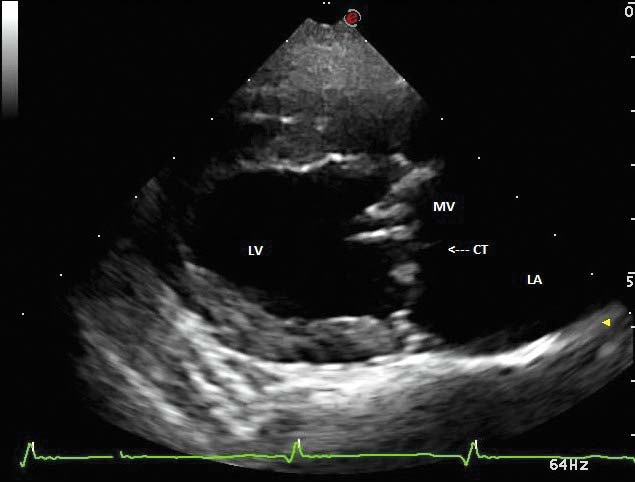
In cases where thoracic radiography does not provide a clear answer, a quick echocardiographic examination allowing visualisation of the cardiac chambers and pericardial space, evaluation of the left atrial size and cardiac contractility may help diagnosis4 (Figure 2).
In all cases, it is important to remember patients in CHF are often critical and can rapidly deteriorate with handling, so stress should be minimised. Diagnostic tests – particularly in severe cases – may need to be performed after initial stabilisation of the patient.
Treatment recommendations vary depending on the severity of clinical signs. Emergency management of CHF often includes oxygen therapy, thoracocentesis in case of pleural effusion, limitation of stress – which may include the use of sedatives – and adequate pharmacologic treatment5.
Recommendations by the American College of Veterinary Internal Medicine (Speciality Cardiology; ACVIM Cardiology) consensus statement for the chronic management of CHF include furosemide, angiotensin-converting enzyme (ACE) inhibitors and pimobendan in symptomatic patients (stage C)5. Spironolactone is also routinely used by most cardiologists in stage C5 and is recommended in refractory cases of CHF (stage D; Table 1).
| Table 1. Treatment recommendations for congestive heart failure treatment (modified from the American College of Veterinary Internal Medicine [Speciality Cardiology] consensus statement)5 | ||
|---|---|---|
| Stage B – asymptomatic patients | ||
| No treatment at this stage. Pimobendan in Dobermanns with dilated cardiomyopathy. |
||
| Stage C – symptomatic patients | ||
| Consensus | No consensus | |
| Acute (hospital-based) | • oxygen • sedation (if animal is stressed) • centesis to remove effusions if they impair • breathing • furosemide • pimobendan (use in cats in case of systolic dysfunction and azotaemia) • nitroprusside, hydralazine (in severe cases) |
• ACE inhibitors • nitroglycerin ointment |
| Chronic (home-based) | • furosemide • ACE inhibitors • pimobendan (use in cats in case of systolic dysfunction and azotaemia) |
• spironolactone • antiarrhythmics (digoxin, diltiazem and beta blockers) • cough suppressants and bronchodilators |
| Stage D – symptomatic patients refractory to treatment | ||
| Consensus | No consensus | |
| Acute (hospital-based) | • as stage C • nitroprusside and hydralazine (more vigorous vasodilation compared to stage C in cases that tolerate it) |
• pimobendan (increased off-label dose) • dobutamine • sildenafil • bronchodilators |
| Chronic (home-based) | • as stage C • spironolactone |
• other diuretics • pimobendan (increased off-label dose) • sildenafil • antiarrhythmics (digoxin, diltiazem and beta blockers) • cough suppressants and bronchodilators |
Loop diuretics act on the thick ascending loop of Henle and are the most effective and potent diuretics. By reducing the intravascular hydrostatic pressure, they decrease the formation of oedema and cavitary effusions representing the mainstay of CHF treatment5,6.
Furosemide has been commonly used in CHF patients in the past and still represents the first line diuretic in veterinary medicine5. Torasemide is a newer diuretic similar to furosemide, but is more potent, with a longer diuretic action (12 hours versus 6 hours) and some potassium-sparing activity due to aldosterone antagonism7-9.
The dose of furosemide required by a dog or cat in CHF may be difficult to determine. Guidelines for management of acute pulmonary oedema in dogs recommend the use of 1mg/kg to 4mg/kg as IV boluses every one hour to six hours, or constant rate infusion (1mg/kg/h) for refractory cases, depending on the severity of clinical signs. Once the respiratory rate decreases, the dose is rapidly tapered to a lower dose5. Cats are more sensitive than dogs to dehydration and azotaemia10, and lower doses are usually used (1mg/kg to 2mg/kg every one to eight hours).
Once the acute phase has been managed, oral furosemide is continued commonly at a dose of 2mg/kg every 12 hours. The dose is then titrated to meet the patient’s needs5. Owners are often asked to keep a chart of the respiratory rate at rest/sleep and, based on this, the lowest most effective dose is used11. In fact, the dosage may vary between 1mg/kg to 2mg/kg PO every 12 hours and 4mg/kg to 6mg/kg PO every 8 hours. Kidney function and electrolytes are monitored to promptly detect abnormalities5.
Torasemide was not licensed for veterinary use until recently and has been typically used as an adjunctive treatment for CHF – especially in cases that develop furosemide resistance – with good results. The licensed formulation has a reported potency of 20 times that of furosemide and the recommended dosage is 0.1mg/kg to 0.6mg/kg once daily. As for other diuretics, monitoring of renal function and electrolytes is recommended during treatment6,8.
ACE inhibitors represent a cornerstone in the chronic management of CHF. They are used in veterinary practice to counteract the renin-angiotensin-aldosterone system (RAAS) by blocking the conversion of angiotensin I to angiotensin II, with consequent reduction of its deleterious chronic effects (vasoconstriction, water and sodium retention and myocardial remodelling)1.
In dogs with CHF, several studies have shown ACE inhibitors improve quality of life and survival12-16 and, among cardiologists, there is consensus on their use in chronic CHF management, while there is no agreement regarding their use in the acute phase5. In fact, they are withheld by some specialists during acute severe CHF because of the possibility of reducing renal perfusion and glomerular filtration rate17.
In cats, ACE inhibitors are not licensed for treatment of CHF and studies regarding their efficacy are lacking. Despite this lack of data, cardiologists use them in chronic CHF as adjunctive treatment.
Generally, renal parameters and electrolytes are monitored over time for an earlier detection of drug adverse effects.
ACE inhibitors used include benazepril, enalapril, ramipril and imidapril, with the following dosages:
Inodilators are a class of drugs characterised by a combination of positive inotropic (increased contractility) and vasodilatory effects. Various agents with different mechanisms of action belong to this class, but pimobendan is the most commonly used in veterinary medicine20.
Pimobendan has a dual mechanism of action – it is a phosphodiesterase III inhibitor leading to arterial and venous dilation, and a calcium sensitiser that results in positive inotropy20.
Several studies have shown the benefit of oral pimobendan treatment in dogs with CHF (PITCH study, VetSCOPE and QUEST)21-24 both in terms of survival and quality of life, making this inodilator a first-line drug to use in CHF, together with loop diuretics and ACE inhibitors. In fact, the ACVIM (Cardiology) consensus statement recommends the use of pimobendan in both the acute and chronic management of CHF due to mitral valve disease, while off-label high dosage is used by some cardiologists in refractory cases5. An IV formulation is available in the UK, allowing an alternative route of administration that may prove useful in acute cases.
Although pimobendan is not licensed for use in cats, retrospective studies have suggested it is well tolerated and shown some benefits in various forms of cardiac disease25-27. It is usually added to classic CHF treatment when systolic dysfunction, refractory heart failure or azotaemia are present3, but studies are required to evaluate its efficacy in these clinical settings.
Dosages of pimobendan are:
Spironolactone has received increased interest after it was shown aldosterone receptor blockage in human patients with advanced CHF reduces morbidity and mortality29. Aldosterone concentration is known to increase in CHF as a result of the activation of RAAS1 and chronic treatment with ACE inhibitors appears to be insufficient to completely block the production of angiotensin II and aldosterone – known as aldosterone escape or breakthrough30.
In veterinary medicine, a study conducted in dogs with CHF due to degenerative mitral valve disease showed spironolactone, when added to conventional treatment, decreased the risk of cardiac death, euthanasia or CHF worsening31. However, some cardiologists raised concerns about the study’s design and disputed a survival benefit could be proved32.
Nonetheless, most cardiologists, including the author, use spironolactone routinely in dogs with CHF and the ACVIM (Cardiology) consensus recommends its use in refractory cases5.
Spironolactone has the following dosage:
One potential adverse effect to note is severe ulcerative facial dermatitis reported in a study regarding Maine coon cats that were receiving a higher-than-recommended dose (2mg/kg every 12 hours)35. Regular monitoring of renal function and serum potassium levels is recommended in dogs with renal impairment, as they may have increased risk of hyperkalaemia during treatment.
Vasodilators act on arteriolar or venous smooth muscle and cause vasodilation. They can be classified as venodilators, arteriolar or balanced (arteriolar and venous) dilators and are generally used for treatment of severe or refractory cases of CHF5,18. By reducing the peripheral vascular resistance, they reduce the pressure against which the heart must pump (afterload), allowing an increased cardiac output with the same force of myocardial contraction.
Nitroprusside is a potent balanced vasodilator for IV administration that has to be used with extreme caution and requires continuous monitoring of the systemic arterial blood pressure.
Nitroglycerine is a venodilator generally used as a transdermal formulation (patches or ointment). It is safer to use and does not require constant blood pressure monitoring, but its efficacy is debatable.
Hydralazine is a very potent arteriolar dilator for oral use.
Dosages of the aforementioned vasodilators are: