8 Jul 2025
Vet nurses and pain management: insights from the Big Pain Survey
Matt Gurney BVSc, CertVA, PgCertVBM, DipECVAA, FRCVS discusses the results from the questionnaire, concentrating on three key areas where VNs have potential to influence.

Image: Snizhana / Adobe Stock
Following the celebration of vet nurses throughout Veterinary Nursing Awareness Month during May, we look at the role of the veterinary nurse in the provision of analgesia, both in the acute and chronic setting.
Each year, the team at Zero Pain Philosophy runs the Big Pain Survey to provide insight into the thoughts that our survey respondents have regarding pain management. Our most recent survey was split into one survey for vets and one for vet nurses – 263 vets and 103 nurses responded. The survey was reviewed by the ethics committee of the Association of Anaesthetists and ethical approval was obtained prior to launching the survey.
The Zero Pain Philosophy community is a global community and in the vast majority of regions in the world, vet nurses are unable to prescribe. We therefore phrased our questions in the survey around asking those nurses what the approach of the clinic they work in is – 78% of respondents work in small animal practice, with 68% working in the UK; 50% of respondents were more than 10 years qualified.
We focused on three key areas in pain management where we felt veterinary nurses have potential to influence, namely osteoarthritis (OA), dental pain and client education.
Licensed options for osteoarthritis
When we asked nurses to describe their clinic’s approach to the treatment of OA, 56% stated that NSAIDs were the first line of treatment; 5% stated that nutraceuticals were first line of treatment; and 18% said the vets in their practice consider other management strategies prior to moving to drug therapy.
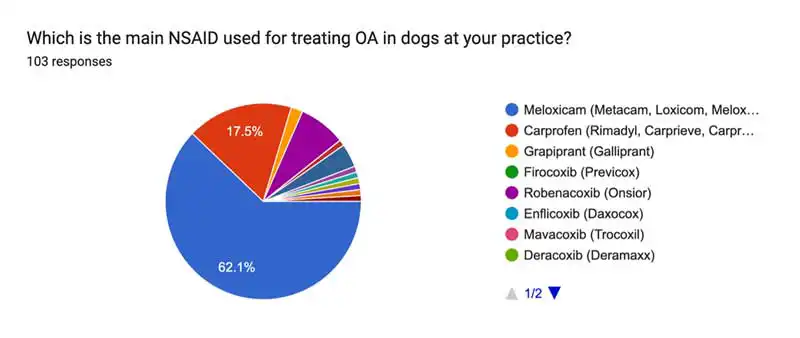
Looking specifically at the NSAIDs used for the treatment of OA in those practices, 62% of respondents stated that meloxicam was the main NSAID used (Figure 1).
A question that we asked to both vets and nurses was: “In your opinion, how effective are NSAIDs in managing the pain of OA?”
This question was answered using a rating system out of 10, with 0 being ineffective and 10 being very effective. The responses from vets and nurses were very similar. The majority of nurses rated NSAIDs having an efficacy of 7 out of 10, and the majority of vets rated NSAIDs as having an efficacy of 8 out of 10.
When asked, “Does the practice use bedinvetmab as a first line treatment for OA in dogs?”, 62% of respondents said no, and that NSAIDs were their first line choice; 23% responded yes and a small proportion (5%) stated that neither of these were first line.
Both NSAIDs and bedinvetmab are licensed for the treatment of the pain of OA. The third licensed class of drugs we have is called the piprants.
The majority of nurses rated the efficacy of gapriprant in managing the pain of OA just 5 out of 10 – overall lower than NSAIDs. Interestingly, no studies are available to compare the efficacy of grapiprant to traditional NSAIDs, so this represents a research opportunity to clarify this opinion.
When asked about their perceptions of the efficacy of bedinvetmab in cases of OA, the responses were more varied. However, the vast majority of nurses rated bedinvetmab 8 out of 10.
Work to compare meloxicam to bedinvetmab for the treatment of OA in dogs reported both products were equally effective in managing OA pain, with efficacy improving over time for both treatments.
Bedinvetmab was associated with fewer adverse effects, however (Innes et al, 2025).
VNs’ involvement
While veterinary nurses are not the prescribers of these drugs, they will be talking to clients in nurse clinics so will form their opinions based on client feedback. Furthermore, VNs have the ability to influence the client despite not being able to prescribe. It is, therefore, important that both pain management educators and pharmaceutical companies provide suitable education to VNs around the efficacy of licensed options for the treatment of OA in dogs and cats.
This leads on to our second question: “If a dog is being treated with NSAIDs for OA and the pain progresses, which second-line analgesic do you see used by the vets in your practice in this situation?”
The response to this question was understandably varied. The majority (29%) stated that bedinvetmab was used as a second line analgesic; 25% said it depends on the specific case and 21% stated that gabapentin was that second-line option. The next most popular response was paracetamol at 11%
It stands to reason that bedinvetmab is a second-line analgesic to use in this situation, given that it is licensed. If we use the vet responses to validate the answers given by VNs, the majority of vets (32%) said that the second-line analgesic depends on the specific case, followed by 22% saying bedinvetmab would be their second-line choice – 19% said paracetamol and 12% chose gabapentin as their preferred next step.
An option that featured lower down in responses from both groups was amantadine. This is interesting when considering unlicensed options, because amantadine is the one drug that has some evidence for it regarding its use as an adjunct analgesic alongside NSAIDs (Lascelles et al, 2008), whereas that evidence does not exist for either gabapentin or paracetamol. There appeared to be little familiarity with the N-methyl-D-aspartic acid (NMDA) receptor antagonists, such as amantadine, which represents a further educational opportunity for pain education providers.
Considering the role of the veterinary nurse in OA clinics, it is important nurses are equipped with the correct tools in order to gather information from caregivers that can be reported back to the veterinary surgeon. The use of pain scales, which are validated in OA, are usually important here. Examples of these include the Liverpool OA in Dogs Score (LOAD) and the Canine Brief Pain Inventory (CBPI). Both of these are completed by the client and provide a useful tool for monitoring the efficacy of our analgesics.
In those cases where OA is diagnosed and the pet has been treated with a licensed option, it is important that veterinary nurses undertake education around second-line options for OA in order to further their own understanding of management of the disease.
An appreciation of the options available in those difficult cases should facilitate booking a consultation with the vet to discuss those options with the client.
CBD
An option that is increasingly popular with clients is the use of CBD. Evidence is increasing in the literature that CBD is effective in dogs with OA, and we expect to see further developments in this field of pain management. In total, 70% of nurses said that CBD was never prescribed routinely for pain management in dogs at their practice, but 5% responded that they saw good results with CBD, whereas 10% of vets said they had seen good results; 31% of vets said they would consider prescribing CBD if there was more evidence; and 26% said the availability of a reliable product would increase their prescribing.
Our view is that the evidence base is growing for CBD and a reliable prescription-only product where CBD content has been verified is essential for future use.
Intra-articular therapies
As pain specialists, we feel there is a role for intra-articular therapies in the management of OA, which could be more widely used in practice. The results of our survey give an interesting understanding of how widely these treatments are used and are a useful benchmark, given the 2023 launch of a licensed stem cell product for dogs (Punzon et al, 2022). A total of 43% of nurses said that intra-articular therapies were not used at their practice; 59% of vets said they did not currently use intra-articular injections, but would like to know more.
Looking further into intra-articular options, it would appear a variety of products are being used by those considering intra-articular therapies, such as stem cells, hydrogels, corticosteroids, platelet-rich plasma and hyaluronic acid.
It is clear from these survey results that further work is required to document the benefits of intra-articular treatments and to share those results with the veterinary community. Our view is that these treatments represent a much-needed targeted option for OA, given that the evidence shows 23% of dogs under the age of four years have radiographic and clinical evidence of OA (Enomoto et al, 2024).
Nutraceuticals
Only 5% of veterinary nurses said nutraceuticals were not recommended for OA management in their practice. Three most common products recommended were glucosamine and chondroitin, green-lipped mussel extract and other omega-3 supplements.
Of the most common supplements used, glucosamine and chondroitin featured highly, despite a clear lack of evidence existing for its use and some authors even stating that glucosamine and chondroitin products should not be used for the management of OA (Barbeau-Grégoire et al, 2022).
Based on our review of the literature, the supplements that we would recommend are omega-3 containing supplements (Barbeau-Grégoire et al, 2022). Evidence is good for specific omega-3 supplementation, such as the specific types of green-lipped muscle extract and supplements containing krill oil (Kampa et al, 2023).
Feline OA
Most nurses rated their confidence in the ability for feline OA pain to be controlled at 8 out of 10; 50% of nurses said that frunevetmab was a first-line treatment for arthritic cats in their practice.
When asked how effective frunevetmab is for managing the pain of OA, the vast majority scored it at 8 out of 10. The responses regarding perceived efficacy of NSAIDs for managing the pain of OA in cats were more varied, ranging from 5 out of 10 to 8 out of 10.
If a cat is treated with NSAIDs and in the scenario of pain progression following treatment with NSAIDs, 32% said the preferred second-line analgesic would depend on the specific case. In 30% of cases, frunevetmab is that second analgesic, and in 27% of cases it is gabapentin. This echoes the responses given for dogs. It shows that vets are using other licensed options first, which is a correct approach according to the cascade. For cats, there are three similar studies looking at the efficacy of amantadine, gabapentin or tramadol in that situation where the cat requires further analgesia. All of these studies are small and therefore underpowered to give definitive outcomes, but a positive benefit was seen in cats with each of those treatments.
Client understanding
The vast majority of nurses rate a client’s understanding and recognition of pain as low and suggested that the following resources would be most useful in assisting client education:
- Web resources for clients to help them understand pain
- Specific resources such as leaflets and videos created by pharmaceutical companies
- Videos featuring key opinion leaders
- Videos from our own practice team demonstrating the benefits of analgesia and conditions that require pain management.

Dental pain
Dental disease is underdiagnosed and nurses agree that dental pain is a leading welfare issue in dogs and cats.
For the respondents of this survey, NSAIDs are the most common first choice for the treatment of dental pain.
Of survey respondents, 10% say that their practice doesn’t use local anaesthesia for dentals. The most common reason given for this was lack of experience with techniques. As the population responding to this survey are subscribers to Zero Pain Philosophy and therefore have a specific interest in pain management, this figure may be lower across all practices.
Barriers
Client understanding and financial restraints were some of the most commonly cited barriers to optimal pain management. Other answers were limited assessment tools and knowledge gaps.
Conclusion
These survey results provide useful insights into pain management practices in primary care practice and the role of the veterinary nurse. Nurses have a key role to play in pain management, and upskilling RVNs in this field is essential to the continued advancement of analgesic excellence.
- Appeared in VN Times (2025), Volume 25, Issue 7/9 (July/August), Pages 12-15.
References
- Barbeau-Grégoire M, Otis C, Cournoyer A, Moreau M, Lussier B and Troncy E (2022). A 2022 systematic review and meta-analysis of enriched therapeutic diets and nutraceuticals in canine and feline OA, International Journal of Molecular Sciences 23(18): 10384.
- Enomoto M, de Castro N, Hash J, Thomson A, Nakanishi-Hester A, Perry E, Aker S, Haupt E, Opperman L, Roe S, Cole T, Archer Thompson N, Innes JF and Lascelles BDX (2024). Prevalence of radiographic appendicular OA and associated clinical signs in young dogs, Scientific Reports 14(1): 2,827.
- Innes JF, Lascelles BDX, Bell D, Tulloch R, McVey A, Northcott C, Welbourn M, Higgins K, Horakova V and Maddox TW (2025). A randomised, parallel-group clinical trial comparing bedinvetmab to meloxicam for the management of canine OA, Frontiers in Veterinary Science 12: 1502218.
- Kampa N, Kaenkangploo D, Jitpean S, Srithunyarat T, Seesupa S, Hoisang S, Yongvanit K, Kamlangchai P, Tuchpramuk P and Lascelles BDX (2023). Study of the effectiveness of glucosamine and chondroitin sulfate, marine based fatty acid compounds (PCSO-524 and EAB-277), and carprofen for the treatment of dogs with hip OA: a prospective, block-randomized, double-blinded, placebo-controlled clinical trial, Frontiers in Veterinary Science 10: 1033188.
- Lascelles BDX, Gaynor JS, Smith ES, Roe SC, Marcellin-Little DJ, Davidson G, Boland E and Carr J (2008). Amantadine in a multimodal analgesic regimen for alleviation of refractory OA pain in dogs, Journal of Veterinary Internal Medicine 22(1): 53–59.
- Punzón E, Salguero R, Totusaus X, Mesa-Sánchez C, Badiella L, García-Castillo M and Pradera A (2022). Equine umbilical cord mesenchymal stem cells demonstrate safety and efficacy in the treatment of canine OA: a randomized placebo-controlled trial, Journal of the American Veterinary Medical Association 260(15): 1,721–1,729.
