24 May 2023
Recruitment and retention issues, and unprecedented demand for services have created a perfect storm that is stretching many practice teams to the limit. With a sizeable number of VNs leaving because they feel undervalued, underpaid and underused, one solution to increasing profits may be staring us in the face…

Image © Tom Jackson

The veterinary profession has been struggling to recruit professionals – both veterinary surgeons and registered veterinary nurses (RVNs). The combined pressures of recruitment and retention, plus the increased demand for veterinary care – due to the post-COVID increase in pet ownership – has created a perfect storm of burnout and attrition.
Unfortunately, no magic wand will improve the situation in the short term, but changes in working patterns and attitudes can improve the situation in many practices (Figure 1).

Nurses face a different set of recruitment issues from vets. Too many are leaving the profession because they feel undervalued, underpaid and underused. Research demonstrates that RVNs can and want to do more in practice (www.rcvs.org.uk), but are not being allowed to do so due to outdated business structures, management and mindset in the veterinary profession.
The traditional hierarchy of veterinary practices piles on to vets activities that could legitimately be carried out by other trained team members, usually RVNs. This vet primacy effectively denies RVNs the opportunity to use their skills and training.
Nurses are also often asked to take on duties because of a reluctance to “add to the wage bill” by employing additional student VNs or non-clinical team members. This short-sighted view limits the potential of practices and contributes significantly to the problems being experienced by both vets and qualified nurses.
Through some considered workforce planning, leverage and a skills-mix audit, nursing staff can be used better. Although the situation is slowly improving, the profession still has a way to go to fully use our RVNs and other team members. The experience of COVID-19 lockdowns and furloughs forced practices to change and use teams better.
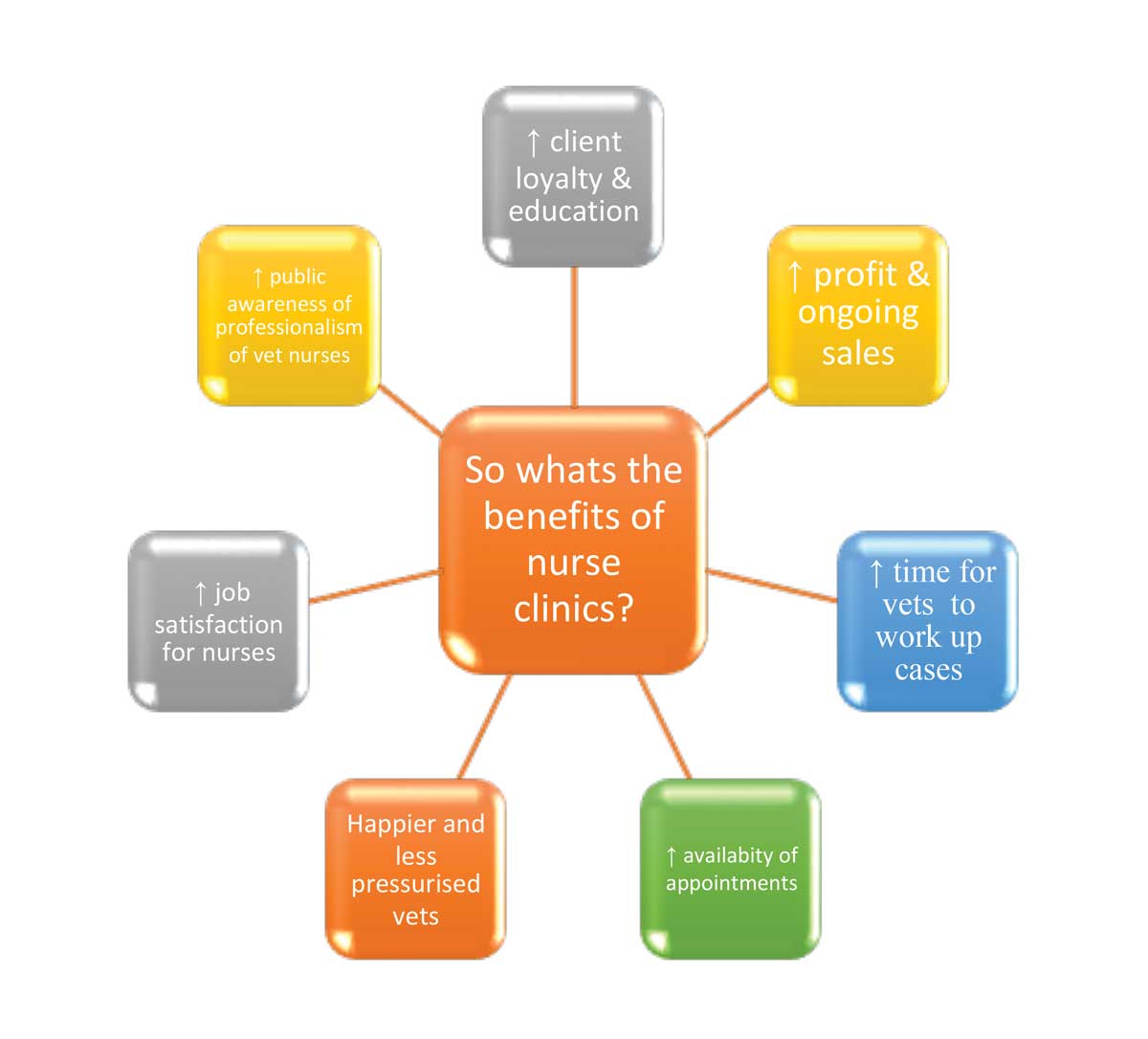
Results can be huge for the practice, teams and clients. Nurses can often give more time to the client to explain health matters, pre and postoperative care, and treatment maintenance. Most patients attending for preventive health appointments have comorbidity – for instance, obesity – which RVNs are perfectly capable of picking up and then referring to a vet if necessary.
It’s worth considering existing workload before asking your RVNs to “do more”. They are very likely already working extremely hard. It’s more about working more selectively – using their skills and knowledge – and freeing them from the work they don’t need to do. This will increase use of their knowledge and skills, increase job satisfaction and likely increase retention.
As a practice owner, it’s also worth considering the probable increased revenue that would come with better using your RVNs for income generation.
The first step to a better future is to ensure you are using all members of the practice team to optimal effectiveness. This means balancing staff “demand” with “supply” to ensure the right number of appropriately trained personnel are available in the right place, at the right time, to match client and patient demand in your practice. It sounds like common sense, but you’d be amazed at how often it doesn’t happen.
By looking at your practice hours, and analysing your busy times by making a “heat map” showing how busy the practice is throughout the day, you can check areas for high and low demand, and ensure the correct ratio of team members is available when needed.
A skills-mix audit examines every aspect of who currently does what, as well as understanding what training your team has undertaken and what roles members are equipped to fulfil.
The important criteria is who could do this task while still being “legal, competent and cost-effective”? It is obvious the practice will use people more effectively if they carry out tasks they are competent and confident in, and don’t carry out tasks they are untrained for, or don’t need to. For commonly occurring duties, it is important to consider the most appropriate person.
RCVS (2017) suggests considering:
Breaking down all the roles in your practice into their individual elements can help instigate a discussion with the team to ensure you allocate the right person and training to the task.
You may find you can move particular elements between individuals to create a more appropriate and balanced allocation of work. For instance, if you look at a “full-time” nursing role – if that nurse wants to work part‑time, you may be able to strip away non-nursing elements and allocate to another member of the team. This could enable them to work part-time.
The responsibility for preventive health advice often falls to the vet. Many of the preventive procedures could easily be allocated to an RVN. If you review your vet consults and see how many could be referred to RVNs for further advice or treatment, you may be surprised this amounts to 20% to 25% of vet-run consultations.
Although many practices provide nurse clinics, they are often in unsuitable times due to availability of consultation space or nurse consults getting cancelled when practices are busy, despite their importance for client care and patient health.
Many vets have a lack of understanding regarding RVNs performing “health checks” or physical examinations within preventive health consults, and a differing opinion within teams on what RVNs should be expected to check.
It’s important to have clear communication with the whole team and agree expectations. One way to aid clear communication is in the procedure name.
“Clinical examination” can be allocated as a full examination by a vet. For nurses, it can be useful to nominate them as “nurse consultations”, “nurse nail clip/anal glands”, or something similar.
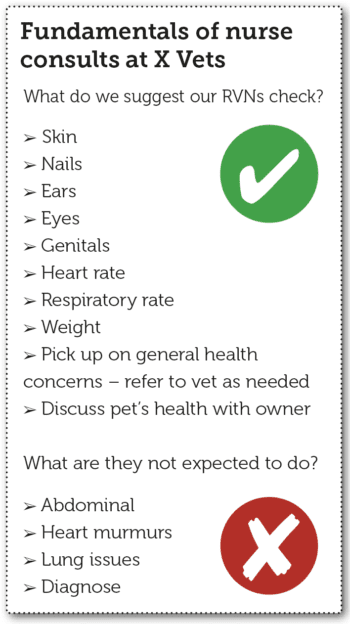
To make it clear, RVNs should not be expected to perform a full physical examination. Diagnosis is a clear area of responsibility RVNs are not expected to fulfil. Figure 2 shows a simple guideline for RVN consultations.
A total of 72% of preventive health consultations have at least one non-presenting specific health problem discussed (co-existing disease; Robinson et al, 2015). It is important RVNs feel confident when – and how – to refer patients for vet advice, and that vets feel happy RVNs will detect and advise appropriately, or refer back to a surgeon as appropriate.
This can be aided with training and practice discussions around delegation, and having a clear process for referring cases for veterinary attention (Figure 3).
Nursing staff can have a huge contribution to inpatient care and forward work-up of clinical cases. For instance, a patient post-veterinary procedure that requires IV line, fluids, bloods, x-ray, blood pressure and ECG could take one hour of work.
An average three-vet practice may have two of these (or similar) cases a day, five days a week, which amounts to 520 hours a year. By delegating (if appropriate) to a suitable RVN/SVN/patient care assistant (PCA) team, you could free up vet appointments or time for other procedures, but also better use RVNs’ skills and knowledge.
When it comes to general roles– such as cleaning theatres, instruments, packing kits and other auxiliary work – it’s worth considering PCAs.
This could free up nurses to carry out the higher-value veterinary work they are trained for. Infection control is an important role for nurses, but general cleaning of practices can be performed perfectly well by trained cleaners or PCAs.
When practices say they can’t afford cleaners or PCAs, our answer is usually “you can’t afford not to”.
On our analysis of many independent practices through our work at Vet Dynamics, often historic associations prevent progression of the RVN role within practice. Positive open communications around delegation can aid this, and having an insightful knowledge of training and experience is really useful.
Discussions around capability and where more confidence, skills or knowledge is needed will aid the way forward. Training and experience can then be tailored to the individual. Having regular, positive, one-to-one reviews with a proactive line manager can help to road mark progression and confidence.
Appraisals can be a useful time to make and review personal development plans for CPD, which can include areas of development such as Schedule 3 and nurse consults. When reviewing individuals, it is worth also reviewing as a team, to ensure the correct skills and training are in place.
The RVN role in practice is often partially hidden from owners. When an owner’s pet has an operation, would the owner know to the extent RVNs are involved in the whole process?
We hope for a future where RVN time is listed on invoices. Increasing numbers of practices are charging for nursing time, services and consultations, and so they should. RVNs are offering a professional service, expect professional salaries, and should be proud to charge their worth.
Once you have a clear view of the roles you need and have allocated work most cost-effectively among those who are qualified to do it, the result is likely to be a resourcing plan that spreads work fairly, is motivating for all members of the team, and creates opportunities – particularly for nurses – to spend more time nursing and generating income for the practice.