27 Mar 2017
Imogen Burrows discusses how to approach this subject with owners, how to carry out an assessment and diagnosing a pregnancy.

Figure 1. Safe rectal examination.
Concise, clear and consistent communication lies at the heart of any equine veterinary matter, and this is especially true regarding breeding.
Whether you are preparing to oversee the next entire stud season, or focusing on managing a single breeding cycle for one mare, it is inevitable many channels of communication will be required with a number of different personnel, including stud managers, equine handlers, veterinary colleagues and owners. Preparing the expectations of an owner, particularly an individual first-time breeder, should be top of the vet’s priority list from the very outset.
First opinion equine practice attracts a wide range of breeding stock, from elite performance horses to the treasured family pony; however, it falls at our feet to undertake best practice in every case, particularly surrounding preventive health measures, such as pre-breeding health testing.
Prior to creating a practice breeding protocol, it is vital to be familiar with the Horserace Betting Levy Board Codes of Practice for the Control of Contagious Equine Reproductive Diseases and understand your responsibilities – both to the client and welfare of his or her horse throughout the breeding process according to the RCVS Code of Professional Conduct Veterinary Surgeons.
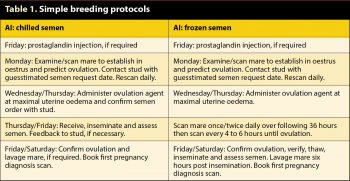
To create robust protocols, a good starting point is to consider each stage you will be involved in – addressing each individually (Table 1).
Stages requiring protocols:
Consultation time: 45 to 60 minutes
1. Consultation without horse: identify client needs, breeding requirements and detailed history. Advise on appropriate health testing and discuss procedures with client.
2. Physical and detailed reproductive examination: identify, record and highlight abnormalities to owner.
3. Consultation without horse: review potential problems and present clear action plan. Set expectations for test results (timing and result, if appropriate). Provide a task list for the owner, such as pay nomination fee, order frozen semen and book recipient mares. Book next appointment.
It is important to set aside a substantial consultation time for this process (Panel 1). Owners will usually have numerous questions and a vast amount of information will be delivered to them, even before clinical examination. This may be your first point of contact with the client and, with successful communication, will undoubtedly pave a smooth path for everyone.
Obtaining a thorough clinical history at this point is invaluable – from this you are better able to understand your client’s specific needs. At this point it is useful to reiterate the need for heath testing and explain which tests will be performed and how. Many studs require negative Streptococcus equi ELISA results prior to accepting visiting mares or stallions, in addition to the standard equine viral arteritis (EVA), equine infectious anaemia (EIA) and contagious equine metritis (CEM) results.
Make sure you are aware of individual stud requirements to avoid unnecessary repeat visits and sampling.
Salient points of the history include:
Clinical evaluation should be thorough, starting with identifying the animal against its passport, verifying vaccination status, including EVA and equine herpesvirus, and a general physical examination, paying attention to, and discussing, conformation concerns.
More detailed examination of the reproductive structures should follow, including speculum and ultrasonographic evaluation per rectum, discussing and recording any relevant abnormalities. Recording findings clearly is vital for future management – documenting or mapping of uterine cysts that could potentially later be confused for pregnancy; follicles more than 25mm and the presence of corpora lutea (CL) are all beneficial.
It is sensible to identify potential problems and signal where action may be required throughout the examination, documenting as you go, then using your notes to review a complete plan at the end of the consultation. This prevents the client being barraged with a list of his or her horse’s faults in one fell swoop, allowing for “signposting” within the consultation.
It is preferable to finish the consultation away from the horse, with a clear and concise recap of relevant findings and a focused plan of action. This may be as simple as discussing the expected date of test results, reassuring the owner all seems in order and booking the next appointment, or something far more complex.
Advising the owner time and finances are well spent, addressing clinical concerns early on, is important. Many clients are keen to brush such concerns under the carpet and just give the first cycle a go. In the author’s experience, more often than not, this approach results in a frustrated and dissatisfied client, often with an associated financial complaint.
Clients will expect to leave this consultation with an idea of when the actual breeding cycle will take place, which may not be possible; however, it is important to address this topic with them. This is often the best time to introduce what they should expect from your AI cycle/package or from taking their horse to stud.
In an ideal world, the pre-breeding assessment will open the door to planning and booking appointments to manipulate the breeding cycle, should this be required, or advise when the mare/stallion should be taken to stud. As most first opinion practitioners will be involved in AI rather than the nitty gritty of natural cover, and by this stage working most commonly with mares, this will be the focus for the remainder of the article.
AI cycles are frequently performed at home or the vet’s clinic; however, safety for both the vet and horse must be at the forefront when deciding on the location. All reproductive work is safest being performed in stocks (Figure 1), which can be a persuading point should these not be available on site. Appropriate restraint is also required and owners should be well informed of the risks of undertaking breeding work (repeated rectal and vaginal examinations) and the associated need for, and costs of, sedation and/or drugs to reduce rectal pressure, such as hyoscine butylbromide.
The vast majority of mares will have prostaglandin administered to facilitate breeding cycle manipulation. This benefits vets and clients by increasing convenience and reducing costs, keeping most examinations within normal working hours. Accurate timing of prostaglandin is essential and examination confirming mid-late dioestrus is strongly advised. The key to successful AI is regular assessment by the same practitioner in a suitably restrained patient. Ensure you allow time to evaluate the mare thoroughly and contact the stud in a timely manner.
Cervical examination per vagina to confirm oestrus is a simple, but underused, technique and may clarify equivocal ultrasonographic findings. Map and record all cysts, follicles more than 25mm and CLs, along with the grade of uterine oedema and presence, quality and depth of uterine fluid. Presence of uterine fluid more than 2cm deep requires action. Cervical examination may highlight a tightly closed cervix despite oestrus – common in the older, maiden sports horse or pony, requiring gentle dilation along with ecbolic treatment (10 IU to 20 IU oxytocin two to four times daily IM; 37.5mg cloprostenol IM more than four hours away from ovulation). It is prudent to perform endometrial swabs, employing appropriate treatment based on cytology and culture where necessary.
Ovulation prediction can be easier said than done, with indicators other than follicle size to look out for. Other changes preceding ovulation include increased echogenicity of the follicle wall, small echogenic particles appearing in the follicular fluid or follicle shape changes other than flattening along with a decline in the uterine oedema score. However, uterine oedema may not decline on foal heat, or when deslorelin is used as an ovulation induction agent.
An unexpected increase in echogenicity with speckling of the follicular fluid, along with an absence of uterine oedema throughout the follicular phase, are all indicators of potential ovulation problems. It is useful to open dialogue with the owner as to whether to avoid inseminating during this cycle, or forewarn of a failed conception.
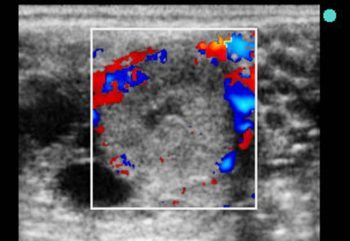
Absence of, or poor, uterine oedema in the true follicular phase is abnormal and warrants assessment, looking for a CL in particular. If found, low levels of circulating progesterone may be present, resulting in a “flat” oestrous cycle. Colour doppler ultrasonography may help to assess CL functionality (Figure 2); minimal blood flow is noted with inactivity. Some mares may respond to teasing; however, 7.5mg to 15mg cloprostenol IM may help recover the cycle. The cycle is unlikely to be successful if no oedema develops.
Should AI be performed using semen shipped from outside the UK, it must be accompanied by the correct, original export and health papers. If this is not the case, the semen must not be used. To do so breaches the RCVS Code of Professional Conduct for Veterinary Surgeons and EU law. While no similar legal requirement exists associated with semen being shipped within the UK, it is our role to encourage best practice at this level and carefully consider the ramifications to the client and horse under your care should unverified and/or infected semen be inseminated.
Paperwork should accompany semen identifying the stallion, time and date of collection, and dates and status of CEM at the very least – ideally, alongside EVA and EIA results, sperm concentration after extending, insemination dose and estimated total and progressive motility after collect before shipping (Horserace Betting Levy Board, 2017).
It is standard practice to advise two ultrasonographic examinations, usually performed at 14 to 16 days and 28 to 30 days post-ovulation to confirm the presence of a single, viable pregnancy. This is particularly important if the mare is not observed to return to oestrus. It is critical to examine the entire uterus, including the length of the body, down to the cervix to perform a complete pregnancy diagnosis.
Following deslorelin use, unobserved ovulations may occur from smaller follicles. By recording any follicle more than 25mm throughout the oestrous cycle, the risk of a second ovulation can easily be ascertained. If there are any concerns a second ovulation may occur, an additional examination should be advised at 18 days post-confirmed ovulation.