23 Jul 2018
Jacqui Matthews takes a look at helminth infection in horses and advice to give to owners.

Lesion caused by pinworm. Image: Callum Blair
Helminth infections are important in horses. Various nematode (roundworm) species can cause disease, with ascarids being primary pathogens in young horses, and strongyles, particularly small strongyles, a threat in adolescent and some mature horses. Cestode (tapeworm) infections are also common.
Helminths can cause severe disease in individuals when infection levels are high.
Small strongyles, in particular, are ubiquitous, with prevalence rates approaching 90%. In these parasites and the ascarid Parascaris equorum, anthelmintic resistance is a considerable issue. As yet, drug resistance has not been reported in the tapeworm, Anoplocephala perfoliata or large strongyle species.
As no new equine anthelmintics are being developed for the market in the short to medium term, helminth control strategies must aim to preserve the efficacy of the current effective compounds.
In terms of control strategies, one size does not fit all and control plans should be approached on a yard-by-yard basis.
Strategies must take into account accurate knowledge of helminth biology and local epidemiology, a sound history of yard management, and be supported by diagnostic testing to inform the application of targeted treatments.
Therefore, such strategies require veterinary surgeons be closely involved in worm control programme design and implementation.
Of the helminths, cyathostomins are the most important. The adult stages are found in the caecum and colon. Most grazing horses are exposed to these worms at some stage and some animals can harbour substantial burdens.
This is a complex group of worms, with around 50 species described; however, in individuals, approximately 10 common species comprise most (more than 90%) of the burden. The same common species are reported globally, in particular Cylicostephanus longibursatus, Cyathostomum catinatum and Cylicocyclus nassatus. These three species regularly account for 70% to 80% of the total burden.
Horses are infected by ingesting third-stage larvae from pasture. The larvae penetrate the large intestinal wall, where they develop through several stages, known collectively as “encysted” larvae. Subsequently, fourth-stage larvae emerge to complete the life cycle in the intestinal lumen. Encysted larvae can persist for several weeks to many months and these stages are undetectable by conventional faecal egg count (FEC) methods (Panel 1).
Encysted larvae can comprise the majority of the burden, particularly in autumn and winter (in the UK), and are important in the pathogenesis of cyathostominosis. These developmental stages can accumulate in substantial numbers; we have enumerated several million larvae in individuals presented as fatal cases or in abattoir studies. Often, such individuals show negative or low (that is, less than 100 eggs per gram; EPG) FEC.
Horses with substantial encysted larval burdens can develop colitis (larval cyathostominosis), the signs of which range from mild weight loss and colic to severe hypoalbuminaemia, diarrhoea and death. This is associated with emergence of large numbers of larvae from the intestinal wall. Severe larval cyathostominosis can be fatal in up to 50% of cases.
Mechanisms underlying larval activation are unknown, but may involve waning of host immunity and/or high worm density in the gut wall. The syndrome does not seem to be associated with a particular species.
Horses vary in susceptibility to cyathostomin infection; most adult animals regulate these worms well and have low infection levels, reflected in their faecal egg shedding. Usually, less than 20% of animals within a group have sizeable burdens, with moderate to high egg shedding (less than 500 EPG). As a result, it is a relatively small number of individuals that contribute the bulk of pasture contamination and we use this feature in designing targeted control programmes.
It is thought each animal’s relative susceptibility to worms is maintained through life; this is supported by studies that demonstrate reasonable consistency in egg shedding in individuals over time.
Infection levels tend to be higher in younger horses, especially those grazed on permanent pastures. For treatment options for cyathostomins, refer to the control section of this article.
Similar to cyathostomins, large strongyles are found in the large intestine; however, in this case, the larval stages are migratory and travel beyond the large intestinal wall. Where they travel to depends on the species, otherwise, their life cycle and epidemiology are similar to cyathostomins.
The most important species is Strongylus vulgaris. Larval stages of this worm migrate to, and develop in, the cranial mesenteric arteries, where they can cause non-strangulating intestinal infarction, resulting in colic. All stages of large strongyle are susceptible to macrocyclic lactone anthelmintics (ivermectin, moxidectin), therefore clinical signs due to these worms are not common. Many horses are on deworming programmes that include regular applications of ivermectin or moxidectin.
Studies from Denmark indicate Strongylus species might “re-emerge” in circumstances where no macrocyclic lactone treatments are administered over a prolonged period. Once-yearly administration of moxidectin to target cyathostomin-encysted larvae should be sufficient to control large strongyle infections in most UK populations. As indicated, no published reports exist of anthelmintic resistance in these species.
Horses generally acquire immunity to the small intestinal nematode P equorum in the first 12 to 18 months of life, so this is only an issue in foals and yearlings.
Eggs are ingested from pasture, then hatch in the intestine, and the larvae undergo a migratory phase involving the liver and lungs. The prepatent period is approximately 10 weeks and patent infections can be detected by the observation of round, thick-shelled eggs by FEC testing. These eggs are environmentally resistant.
P equorum infections are relatively common, especially on large breeding establishments that graze youngsters on permanent pastures. Removal of dung from pasture and proper composting are especially important on such premises.
P equorum infection can lead to clinical signs (respiratory signs, poor condition, colic) when infection intensity is high. The associated colic has a poor prognosis. Like cyathostomins, anthelmintic resistance is an issue. Treatment failures against P equorum have been reported for ivermectin, moxidectin and pyrantel embonate.

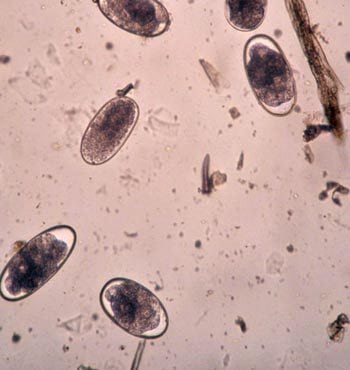
Reports of pinworm infection have been increasing in the UK in the past decade. The reason for this is not known, but could be associated with anthelmintic resistance, low efficacy of products selected to treat infections, and an increase in environmental conditions conducive to the survival and development of the pre-parasitic egg stage.
In most cases, infection produces few/no clinical signs, but persistent infection in some individuals can lead to damage around the perineum and tail head. Environmentally resistant eggs are ingested from the environment (for example, gates, fences, stable doors and troughs). The intra-host stages are found in the terminal large intestine and female worms migrate to the perineal area to lay eggs, which are transferred to the environment when the horse rubs.
Anthelmintics that have licensed efficacy against larval and adult Oxyuris equi include ivermectin, moxidectin and fenbendazole, although not all brands have a licence for this activity. Pyrantel embonate has licensed efficacy against adult stages only. Anecdotal reports indicate O equi populations are becoming increasingly refractory to anthelmintic treatment and, in the author’s experience, “lack of effectiveness” has been observed with all anthelmintic classes.
It is critical exemplary hygiene is practised to reduce egg infection levels in the environment. Thorough cleaning with a strong (horse-friendly) disinfectant, after removal of all bedding, will reduce the risk of infection from the environment. Areas to be cleaned include anywhere animals might rub against and dislodge pinworm eggs – for example, stable doors and walls, mangers, troughs, gates and fences.
Thorough daily cleaning of the perineal area and tail-head of infected individuals (egg shedding can be detected by “tape testing”) must be undertaken. Plaiting the tail and applying petroleum jelly in the area to help dislodge female worms can help make the environment less supportive of the worm’s preferred habitat. Post-treatment monitoring for infection by tape testing is important in assessing effectiveness of the products used, as well as the management measures applied.
A perfoliata infection is relatively common in horses of all ages in temperate regions.
Although reports of clinical disease associated with this parasite are relatively rare, horses with high burdens can develop spasmodic and impaction colic. A perfoliata has an indirect life cycle involving an oribatid mite. Horses are infected by ingesting mites containing tapeworm cysts. All parasitic stages live at the ileocaecocolic junction.
Standard FEC analysis is insensitive in detecting tapeworm eggs, especially as the egg shedding is inconsistent. Well-validated blood and saliva tests, based on the detection of A perfoliata-specific antibody, are available in the UK. These can be used to inform the application of one or two anti-tapeworm treatments each year (spring and autumn).
Anthelmintics with licensed efficacy against A perfoliata include praziquantel and pyrantel embonate (at twice the dose used for control of roundworm infections). Unless otherwise specified (for example, when applying a strategic or FEC-informed application for nematode infection), anthelmintic products with a narrow spectrum should be used for tapeworm treatments. This will become an issue in the UK due to the impending removal of the single praziquantel-only product from the market.
Fluke mainly affects sheep and cattle, but it has a broad host range. Horses exposed to infective metacercariae on pasture can be infected. This parasite is an emerging problem in UK horses, perhaps because of an increase in prevalence of the pathogen in ruminants and, possibly, due to an increase in co-grazing management practices. The pre-parasitic stages thrive in wet, marshy areas in which the intermediate host mud snail proliferates.
Adult flukes are found in the bile ducts and migrating larvae in liver tissue. Overt clinical signs are not usually observed in infected horses, but raised liver enzymes in serum may be noted, along with non-specific signs, such as weight loss and malaise. Eggs are excreted via dung, but are not detectable by standard FEC tests because they are heavier than nematode eggs. For this reason, faecal sedimentation counting methods are required to pick up patent infection and several samples may need to be tested before eggs are detected. A serum-based diagnostic test is available at the University of Liverpool (www.liverpool.ac.uk/testapet/test). If infection is detected, flukicidal products must be prescribed by a vet under the cascade, as no flukicides are licensed for use in equids in the UK.
Triclabendazole is the anthelmintic of choice due to its wider spectrum of activity against different developmental stages and its lower toxicity profile, compared to other flukicides. However, a number of reports of triclabendazole resistance in liver fluke in sheep exist, so it is possible Fasciola hepatica populations, to which horses are exposed, are resistant to this compound. Therefore, post-treatment monitoring for fluke eggs in dung (approximately six weeks after treatment) and observation for concomitant reductions in clinical signs and serum liver enzyme levels should be undertaken.
Where triclabendazole is shown to be ineffective, closantel may be considered. This is only effective against adult fluke, so a second application is required 8 to 10 weeks later to target larval stages that had matured in the intervening period. Symptoms of overdosing include blindness, anorexia and ataxia, and care should be taken with the dose administered. Control must address the exclusion of snail habitats by fencing or drainage, which will help break the parasite’s life cycle.
Other helminths infect horses include the nematodes, Dictyocaulus arnfieldi (lungworm) and Strongyloides westeri, but are not discussed here as they are relatively rare compared to those already described and tend to be seen in specific circumstances, namely when horses co-graze with donkeys (lungworm) and young foals are raised in unhygienic conditions (S westeri).
Percentage of FEC reduction (FECR) = ([mean day 0 FEC – mean day 14-17 FEC]/ mean day 0 FEC) × 100.
Three classes of broad-spectrum anthelmintic are available for the treatment and control of nematode infections in horses. These are, in order of when they were licensed:
When each anthelmintic class was introduced, these products were shown to have excellent (more than 90% or more than 95%, depending on the class) efficacy against adult strongyles and P equorum, as well as against the other nematode species mentioned.
Some products have licensed efficacy against immature strongyles (ivermectin and moxidectin against large strongyle larvae, and moxidectin against small strongyle larvae); however, anthelmintic resistance is now widespread in populations of cyathostomins and P equorum.
Resistance is an inheritable characteristic passed from one generation of worms to the next. In the presence of resistance-conferring gene mutations, each time a treatment is applied, the majority of worms that survive treatment are resistant. Following repeated treatments with the same compound, resistant worms eventually constitute a large proportion of the population and, eventually, the drug ceases to be effective, identified as a failed efficacy test or the observation of continuing clinical signs following treatment.
Horse movements (for example, between stud farms) encourages gene flow ensuring, in the absence of appropriate quarantine procedures, inherited resistance traits are moved from one population to another.
Worryingly, multi-class resistance is an emerging issue and has been detected in cyathostomins and P equorum on a number of premises in the UK. Unfortunately, reversion of a resistant worm population to anthelmintic sensitivity does not occur, even when a population of worms remains free from a particular anthelmintic for several years.
In terms of the individual classes, benzimidazole resistance is very widespread in cyathostomins worldwide. The benzimidazole, fenbendazole, when administered as five consecutive daily treatments, has licensed efficacy against all stages of cyathostomin encysted larvae. However, levels of resistance are such that use of fenbendazole for this purpose is not recommended, unless the nematode population’s sensitivity to the compound is known. Anthelmintic sensitivity can be tested by performing a FEC reduction test (FECRT; Panel 2).
Reports of pyrantel resistance in cyathostomins have become relatively commonplace, and resistance to both benzimidazole and pyrantel compounds in single cyathostomin populations is not unusual. For this reason, the impact of pyrantel embonate treatment on egg shedding should be investigated by efficacy testing, especially where there has been a history of regular use of the compound.
Few reports exist of macrocyclic lactone resistance in cyathostomins as measured by FECRT, although a reduction in strongyle egg reappearance period after treatment (taken as an early sign of resistance) has been reported in several regions for both ivermectin and moxidectin.
The high levels of benzimidazole and pyrantel resistance reported in cyathostomins, combined with early indications of resistance against macrocyclic lactones, is very concerning given no new compounds are on the horizon and it emphasises that judicious use of these medicines should be a priority in all equine worm control programmes. Added to this are the many reports of macrocyclic lactone resistance in P equorum in several regions. In some cases, multi-drug resistance has been reported, with lack of effectiveness of macrocyclic lactones, pyrantel and fenbendazole recorded in the same population, leaving no licensed options left for effective chemical control of these potentially pathogenic worms.
Control programmes should aim to balance the avoidance of disease with maintaining anthelmintic efficacy. This can be done by stopping regular all-group treatments (“interval dosing”).
Anthelmintics should be administered on the basis of:
Strategic treatments should be applied in autumn/winter to target cyathostomin encysted larvae, as well as large strongyle larvae. Moxidectin is recommended for this purpose. Some animals, for example groups of yearlings grazed outside over the winter, may require a second strategic treatment with moxidectin in late winter/early spring to target developing larvae from infections ingested over winter.
Regular FEC analysis has the advantage that it identifies horses likely to be more susceptible to infection and, therefore, at risk of potential disease.
FEC tests do not give an accurate estimation of total burden within an individual and do not assess levels of immature worms, such as P equorum larvae, cyathostomin encysted larvae or S vulgaris larvae. When undertaking FEC tests, keep in mind the strongyle egg reappearance period for each compound (pyrantel and benzimidazole – 4 to 6 weeks; ivermectin – 8 weeks; moxidectin – 13 weeks). This determines how soon after the last treatment FEC tests should be performed. If many positive FEC are observed in a population before or around the standard egg reappearance period, this is indicative of resistance, and a FECRT (Panel 2) should be performed using the compound in question. Note nematode eggs can reappear faster post-treatment in younger animals, which should be taken into account when deciding how soon after treatment to perform the next FEC test.
No evidence-based published guidelines exist on the cut-off EPG value on which to base anthelmintic treatment. Between 200 EPG and 500 EPG is a good starting point, and the threshold selected should depend on grazing management and other factors identified on site. For example, adult horse populations on clean pasture at a low stocking density are likely to require a higher cut-off threshold than a group of yearlings grazed at a higher stocking density on paddocks where pasture hygiene methods are not in place. Vets need to work closely with clients in customising thresholds to suit the requirements of individual establishments.
Tapeworm control is best applied on the basis of diagnostic testing. Well validated saliva and serum-based tests are available from EquiSal (http://equisal.co.uk) and the University of Liverpool (www.liverpool.ac.uk/diagnosteq), respectively. These tests can be applied in spring and autumn.
A key component of control programmes is to ensure targeted and strategic anthelmintic treatments are supported by good management (Panel 3). Paddocks should not be overstocked and dung removed from pastures (this is especially important when horses are intensively grazed).
Removal of dung twice per week has been shown to significantly decrease the number of worm eggs shed by resident equids, and so the frequency of anthelmintic treatment is lowered.
A study by the author indicated horses on premises where no dung removal was performed were more likely to have shorter strongyle egg reappearance periods after moxidectin treatment than horses where dung removal was practised. The former group required more frequent anthelmintic treatments, increasing selection pressure for resistance.
Dung should be properly composted if it is to be spread on to grazing land. It is recommended it be composted for at least six weeks with regular turning. A minimum temperature of 50°C to 70°C is suggested to kill helminth eggs.
Co-grazing with ruminants can be practised as most worms do not cross the species barrier, but care should be taken where mud snail habitats are present as horses can be infected by liver fluke. In these cases, drainage of grazing land and treatment and monitoring of other livestock for liver fluke is recommended.
In addition to good pasture hygiene, best practice must be applied in administering anthelmintics; dose rate should be based on an accurate assessment of weight (using weigh scales or a good quality girth tape), and all anthelmintic products stored and applied in accordance with the summary of product characteristics. Annual efficacy testing should be undertaken to ensure the products being used continue to be effective (Panel 2).
In terms of reducing the spread of resistant worms from one site to another, all new arrivals should be stabled and treated with moxidectin, combined with praziquantel to target as many species and stages of nematode and cestode as possible. Horses should be kept off grazing for three days after treatment and a follow-up FEC test performed 14 days after treatment to check the product has been effective against nematode adult worms.
With the extent of benzimidazole and pyrantel resistance in cyathostomins, it is difficult to “rotate” anthelmintic classes between treatments or years.
For nematode control, ivermectin may be used for treatments based on FEC testing (spring to autumn), in combination with a strategic treatment with moxidectin in the autumn/early winter to target encysted stages. Where pyrantel efficacy has been established by FECRT, this compound could be used for FEC-directed treatments, along with the larvicidal (moxidectin) autumn treatment. Praziquantel or pyrantel (at twice the dose used for nematode treatment) are recommended for tapeworm treatment on the basis of diagnostic testing as already indicated.
By using a diagnostic-led approach, selection pressure for anthelmintic resistance should be reduced because fewer treatments are applied in the population as a whole.
FEC tests cannot detect immature stages and are a poor correlate of total worm burden.
For cyathostomins, a test is being developed to a commercial assay that shows promise for detecting infection.
Going forward, increasing levels of anthelmintic resistance will provide a challenge to vets in practice. Therefore, more evidence-based control methods, based on a sound knowledge of the biology and epidemiology of infections, combined with diagnostic tests, should be applied.
The author thanks The Horse Trust, the Horserace Betting Levy Board, The Thoroughbred Breeders Association and The Donkey Sanctuary for their support.