31 Oct 2016
Jonathon Dixon explains the importance and value of diagnostic imaging as a tool for managing joint issues in horses.
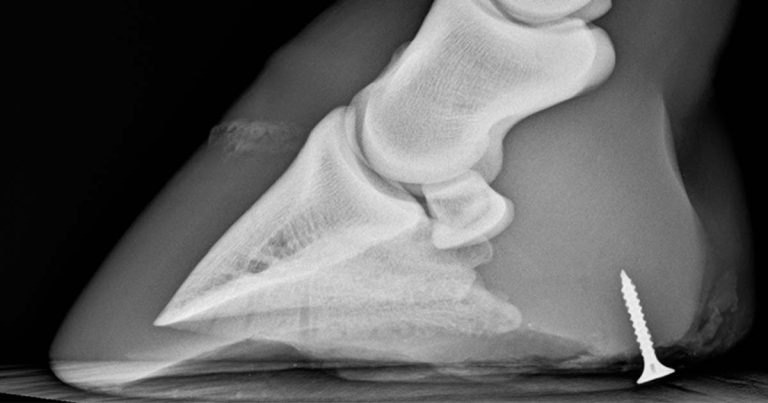
Figure 2. Lateromedial radiograph of the foot of a horse that has stood on a screw. Use of imaging prior to removal gives indication of the orientation and depth of the foreign material.
Orthopaedic emergencies in equine practice are common, with clinical examination one of the most important diagnostic tools. However, often diagnostic imaging can add vital information that cannot be obtained using other methods.
Orthopaedic emergencies are commonly encountered by vets in first opinion and referral practice.

When approaching an orthopaedic emergency, a clinician will need to base the initial assessment on the extent of lameness, stability of the limb, degree of pain shown by the horse and if immediate intervention or euthanasia is required. More frequently encountered equine orthopaedic emergencies include fractures, wounds, foot abscessation, synovial contamination, laminitis, foot penetrations and soft tissue lesions or lacerations – for example, superficial or deep digital flexor tendinopathy.
In many cases, thorough clinical evaluation is the most important tool practitioners have at their disposal and can often provide the required information to obtain an accurate diagnosis. Not all cases are straightforward and, in these circumstances, additional information may be useful.
Nowadays, in first opinion practice, availability of portable radiography – either computed radiography or digital radiography – and affordable portable ultrasonography provide excellent tools that can be transported to the patient side. More recently, battery powered radiography units mean imaging can be performed remotely, which may improve patient care that can be provided in the field – for example, should a horse or pony be unable to move.
When considering the use of imaging in the severely lame horse, it is important for a veterinary surgeon to act in a timely fashion. However, a clinician should not be pressured into rushing to a diagnosis, which can be a downside of the images being available immediately.
Many horses can be stabilised in the short term using bandaging, limb casting, splint application, movement restriction and analgesia, while interpretation can be performed. This also allows for time to consider obtaining a second opinion from a colleague or referral hospital, should this be required. Rushing to obtain a diagnosis can lead to misinterpretation of the findings or a lesion being overlooked.
An adjunct to this interpretation would include the environment within which images are viewed; bright sunlight reflecting on a monitor is not conducive to subtle lesion detection and a careful approach is needed (Puchalski, 2008). It may be required that image viewing takes place in a darkened environment to localise subtle radiographic abnormalities.

Once a decision to use imaging in the diagnostic workup of a case has been made, it is important to obtain the correct information – this requires acquisition of high-quality
images, no matter the modality chosen (Thrall, 2013). For radiography, this would constitute:

Appropriate use of limb markers to indicate laterality and radiographic projection, and often additional use of lesion markers – for example, to highlight the location of a wound.

Evaluating images obtained can then be performed. This should take the format of a systematic review of each image, taking care to evaluate soft tissues and osseous structures. With each lesion identified, it is important to determine if this finding is likely to be related to the existing concern – does it fit the clinical picture?
The presence of a small, rounded bone fragment within a joint of a horse that has a wound overlying the region may not represent a fracture fragment – it is absolutely reasonable this could be an incidental osteochondritis dissecans lesion.
The fragment’s appearance will often help with this assessment. Acute fracture fragments are typically sharply demarcated, angular, often associated with soft tissue swelling and should have a similar appearance to the fragment bed. Long-standing intra-articular osseous structures are more often rounded and smoothly outlined.
It is important to remember some lesions are not necessarily visible immediately – in particular, this applies to detection of fractures and sequestration of bone. If a fracture is suspected, a clinician should deviate from the standard views of the region if these should not allow identification of the lesion (Figure 3).
In this scenario, one should obtain additional views at varying angulations around the limb. An incomplete or short fracture within a bone may only be visible when a radiograph is obtained with the path of the x-rays orientated parallel to the fracture plane. Some fractures – especially incomplete cyclical loading (or “stress”) fractures – may never be visible radiographically and may require use of other modalities, such as nuclear scintigraphy, for detection. Suspected fissure fractures of long bones, even if not visible on initial radiographs, should be treated as such and radiographed again in 10 to 14 days when bone lysis/osteoclastic activity may make the fracture more evident.
Wounds on radiography appear as skin defects with or without evidence of SC and tracking gas lucencies in the underlying tissues (Figure 4).
Whenever wounds are in close proximity to synovial structures then synovial contamination or communication must be considered. Involvement of a synovial structure constitutes a surgical emergency and, should this be suspected or confirmed, the referral to a surgical facility is advised.
Evaluation of wounds around a joint, tendon sheath or bursa can be aided with the use of radiography – in particular to assess for the presence of gas that may extend into a synovial structure and foreign material. Where possible, radiographs should be obtained prior to synoviocentesis, thus any presence of gas in a synovial structure should be further investigated (Figure 5).
Contrast radiography can also be used to assess for leakage from a synovial structure through a wound when injected at a site remote from any skin wound or contamination (Barker, 2015). It is, of course, recommended a needle should not be passed through a wound into a synovial structure to avoid iatrogenic contamination.
It is important to remember not all foreign material is radiopaque – objects such as wood can be radiolucent compared to bone and soft tissues.
Occasionally, vets will encounter lesions in an emergency that may be unfamiliar. In this scenario, comparison to the contralateral limb is a useful adjunct technique, which may aid recognition of anatomic variation in an individual versus pathological findings. This principle applies equally to all imaging modalities and is easily obtained with radiography and ultrasonography.
Ultrasonography is a vital tool in the practitioner’s arsenal to evaluate soft tissue and bone lesions – in particular, for tendon and ligament lesions. Ultrasonography requires careful preparation of the patient, often removal of the hair coat, application of a soap-based skin cleanser, followed by surgical spirit and use of an ultrasound contact gel.
Images should be obtained of soft tissue structures in two planes (typically transverse and longitudinal) and potentially comparison images of the contralateral limb. Ultrasonography is critical in the assessment of tendon or ligament lesions and lacerations, where assessment of the extent of damage from palpation alone may not be possible (Figures 6 and 7).
In some circumstances, it is prudent to consider early use of advanced imaging, such as CT, for complex fractures prior to surgical repair, or MRI in cases of foot penetrations (Urraca del Junco et al, 2012). In this scenario, the ability to identify tendon or ligament damage, in addition to involvement of osseous structures, is critical to an accurate diagnosis (Figures 8 and 9). Significant potential benefits exist to MRI over CT here, in that MRI can be performed in the standing horse, avoiding the risks of general anaesthesia.
Imaging has a clear place in the diagnostic workup of equine orthopaedic emergencies, but should not replace a thorough clinical examination, nor unduly delay required intervention to the detriment of patients. The increasing availability of affordable digital imaging systems will continue to improve patient care possible in the field and result in the benefit of being able to send images to referral hospitals, providing useful information to clinicians prior to patient arrival.