10 Oct 2016
Lindsay Brazil discusses the use of and studies into this drug when treating lower airway conditions presenting in horses.

Figure 1. Tracheal mucopus in a horse affected with recurrent airway obstruction. Image: Tim Brazil.
Recurrent airway obstruction (RAO) and inflammatory airway disease (IAD) are commonly diagnosed equine diseases (Figure 1). Differences exist in signalment and clinical signs between them, but treatment protocols are similar for both. Treatment consists of environmental management, bronchodilation and reduction of inflammation. Bronchodilation is commonly achieved with clenbuterol, a potent β2-adrenoreceptor agonist. Clenbuterol has also been recognised as having anti-inflammatory properties.
Clenbuterol is still a popular choice for treating equine lower airway diseases. Stimulation of β2-adrenoreceptors on smooth muscle causes an increase in intracellular cyclic adenosine monophosphate concentration and subsequent smooth muscle relaxation. In addition to this well-known bronchodilatory effect, research has shown clenbuterol has other beneficial effects in horses. Activation of β2-adrenoreceptors on mast cells, macrophages and other cells in the inflammatory cascade has been shown to down regulate pro-inflammatory mediators, which, in turn, contributes to a clinical improvement in conditions such as RAO and IAD.
Clenbuterol has been used as a bronchodilator in horses since 1977 and is still a popular choice for treating equine lower airway diseases.
Recurrent airway obstruction and inflammatory airway disease
Recurrent airway obstruction (RAO) and inflammatory airway disease (IAD) are commonly diagnosed equine diseases (Figure 1). Differences exist in signalment and clinical signs between them, but treatment protocols are similar for both. Treatment consists of environmental management, bronchodilation and reduction of inflammation. Bronchodilation is commonly achieved with clenbuterol, a potent β2-adrenoreceptor agonist. It has also been recognised clenbuterol has anti-inflammatory properties.
Although the presence of β-adrenoreceptors was identified in 1948, it was not until 1967 that Lands et al divided them into three subtypes – β1 to β3. All are G-protein-linked and produce their effects by an intracellular signal cascade, which, ultimately, results in a rise of cyclic adenosine monophosphotase (cAMP) concentration.
The effect of each subtype is defined by its location in the body. The distinction between the location of β1 and β2 is an important one. β1 are found mainly on the heart and are responsible for positive ionotropic and chronotropic effects. β2 are more widespread, so have multiple actions, including smooth muscle relaxation, inhibition of histamine release and inhibition of inflammatory cytokine production. β3 are found on the bladder and adipose tissue. By using a receptor-specific drug, a targeted response can be achieved and systemic side effects can be avoided.
In 1977, Sasse and Hajer reported clinical observations suggesting NAB365 (later renamed clenbuterol) was a useful bronchodilator agent in horses with various respiratory diseases (Derksen, 1994).
Since then, clenbuterol has become an important drug in the treatment of respiratory disease in horses. It is part of the large family of β2-adrenoreceptor agonists, but has several advantages over other members. For instance, it is more lipid soluble than salbutamol, resulting in a high oral availability. This means, when administered orally, clenbuterol readily moves into plasma and so has effects throughout the body.
The predominant effect of clenbuterol is relaxation of smooth muscle, resulting in bronchodilation. Stimulation of β2-adrenoreceptors on smooth muscle causes an increase in intracellular cAMP concentration and subsequent smooth muscle relaxation.
Clinically, Robinson (2001) found this resulted in a decrease in pulmonary resistance, an increase in dynamic compliance (the ability of the lung to expand) and a decrease in the change in pleural pressure (indicating less respiratory effort).
Histamine is an important mediator in airway inflammation. Histamine’s release from mast cells is triggered by antigen activation of membrane receptors. As in smooth muscle, activation of mast cell β2-adrenoreceptors results in an increase in intracellular cAMP concentration, which stops histamine release. β2-adrenoreceptor agonists have also been shown to reduce the release of tumour necrosis factor-α (TNF-α), a key regulator of the immune system, from macrophages.
One effect of TNF-α release is to recruit neutrophils to the site of injury. Neutrophil content of the bronchial mucosa has been found to be reduced in asthmatic humans after treatment with β2-adrenoreceptor agonists. These changes were not found when corticosteroid was used as the sole treatment (Johnson, 2002). Th2-type cytokines are another group of immune system regulators that promote inflammation and are released by a range of cell types, including macrophages, neutrophils and epithelial cells. The release of cytokines is stimulated by lipopolysaccharide, which is found on the membrane of Gram-negative bacteria commonly found in mouldy hay.
In horses with lower respiratory inflammatory disease, production of receptors for Th2-cytokines is increased. Clenbuterol has been shown to prevent this increase in pulmonary epithelial lining fluid in horses challenged with LPS (van Hoven et al, 2004). This study showed clenbuterol modulates the communication between the different cell types in equine airways and reduces the presence of pro-inflammatory mediators, which, in turn, leads to a clinical improvement.
The multiple anti-inflammatory effects of clenbuterol previously described may allow for a reduction in the use of glucocorticoids, which have, in themselves, potential systemic side effects, such as immunosuppression and polyuria-polydipsia. Certain glucocorticoids are also contraindicated in horses at risk of laminitis. In these cases, clenbuterol could be used alone to provide bronchodilation and to reduce inflammation.
Change in quality and quantity of mucus is a common finding in RAO-affected horses (Robinson, 2001). The airways become filled with large quantities of thick sticky-appearing mucus. In addition, the cilia can be phagocytosed by macrophages, which leads to a cessation of the mucociliary escalator. Clenbuterol is an effective mucokinetic agent in horses (Dixon, 1992). The likely mechanism through which it improves mucokinesis is a stretching and thinning of the mucus layer, thus allowing more effective ciliary action.
Clenbuterol has been widely used in the treatment of RAO for 35 years. Used alone in a blinded randomised trial with RAO-affected horses, five out of six given clenbuterol for three weeks showed improvement, compared with those in the control group (Genetzky and Loparco, 1985). Horses showed an improvement in respiratory performance, as well as a decrease in mucus volume. Treatment for these horses was continued at home after the experiment. In all but one, the owner noticed a clinical improvement.
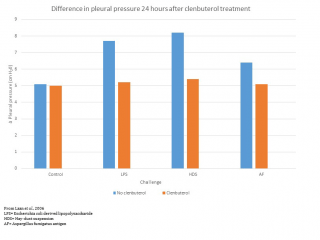
In another study, RAO-susceptible horses were given clenbuterol 0.75µg/kg IV twice daily, or a placebo, and then challenged with inhaled allergens. Those treated with clenbuterol showed a reduced concentration of neutrophil and pro-inflammatory mediators on bronchoalveolar lavage cytology (Laan et al, 2006). In the same study, the difference in pleural pressure was measured 6 and 24 hours after allergen challenge. An increase in the difference indicates an increase in respiratory work.
Figure 2 shows how respiratory work was significantly increased after inhalation of lipopolysaccharide and hay dust suspension in untreated horses. However, it remained at baseline values when treatment with clenbuterol preceded the challenge.
Untreated RAO can lead to irreversible airway remodelling. Fibroblast activity associated with airway inflammation causes thickening of the airway wall. Fibroblast concentration increases in RAO-affected horses. Clenbuterol reduces fibroblast proliferation, thereby reducing the risk of irreversible airway remodelling and maintaining normal structure of the respiratory tree (Franke and Abraham, 2014). Therefore, early treatment with clenbuterol of horses predisposed to RAO should be considered (Laan et al, 2006).
Read et al (2012) showed in IAD-affected horses, treatment with oral clenbuterol resulted in a significant broncho-protective effect. Eight horses were given 0.8µg/kg orally twice a day for 21 days. The concentration of inhaled histamine required to increase airway impedance significantly increased during treatment with clenbuterol, compared to the placebo treatment.
Read et al also found tachyphylaxis (a decrease in response to a drug after repeated administration) was evident after 21 days of treatment. This reflects work carried out in humans that showed the broncho-protective effect of β2-adrenoreceptor agonists wanes over time. In the case of clenbuterol, the tachyphylaxis is a result of a decrease in receptor numbers and a decrease in sensitivity of the remaining receptors.
Corticosteroid treatment reverses the down regulation and promotes up regulation of β2-adrenoreceptors (Adcock et al, 2002). For this reason, it is now recommended in humans daily administration of β2-adrenoreceptor agonists should only be used in conjunction with inhaled corticosteroids. Read et al (2012) concluded extended use of clenbuterol in horses should be combined with inhaled corticosteroids and administration of clenbuterol for more than 14 consecutive days without inhaled corticosteroids should be avoided.
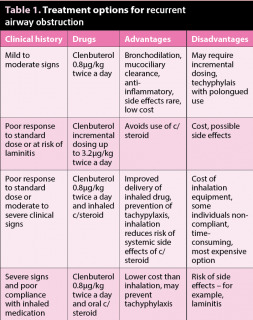
The recommended dose is 0.8µg/kg orally twice a day. However, a study by Erichsen et al (1994) showed doses up to 3.2µg/kg can increase the clinical effect of clenbuterol with no detrimental effects. In an editorial of Erichsen’s paper, Derksen (1994) advised clenbuterol should be administered “to effect”, beginning at 0.8µg/kg. Starting at any higher dose may result in side effects, such as tachycardia and sweating. A suggested dosing regime is shown in Table 1.
Commercial preparations are available in syrup or granule form. Syrup is preferred as it produces no dust, so helps avoid accidental contamination of feed for horses that may be racing or competing within the detection time for clenbuterol. The British Horseracing Authority’s published detection time for clenbuterol, given as an oral syrup at 1.6µg/kg for 10 days, is 312 hours (13 days).
Clenbuterol has a long history of being used as a bronchodilator and remains popular with clients – in part, due to its minimal side effects. As this article describes, research demonstrates it has anti-inflammatory, as well as bronchodilatory, actions. Clenbuterol should always be considered in the treatment plan for equine lower respiratory tract disease.