2 Mar 2021
Ann Derham looks at musculoskeletal disorders, which cover a wide range of diseases and problems, in this article from the spring 2021 issue of Vet Times Equine.

Musculoskeletal disorders (MSDs) are common in horses. They not only affect their ability to move, but may impact day-to-day activities (for example, breathing, eating, swallowing or urinating).
These disorders often cause pain, and can lead to performance and financial loss.
The equine musculoskeletal system is complex, comprising of muscles, tendons, ligaments, nerves, bones, cartilage and other connective tissue. Each of these, or several of them, may be the source of injury, and it is important to remember that all organ systems are interrelated, and disorders elsewhere in the body may manifest in the musculoskeletal system. Bone disorders may be present at birth – for example, incomplete ossification of the cuboidal bones – or develop secondary to trauma, poor nutritional management, tendon/ligament injuries or infection.
Synovial disease/disorders may involve the synovial membrane alone or also involve associated ligaments/tendons, cartilage and bone. Trauma, developmental issues and infections may also lead to issues here.
Inflammation of the joint and associated bone is termed OA, and is a common cause of pain and poor performance due to the progressive deterioration of the affected joint or joints (Contino, 2018). Myopathies may be acquired or inherited and can affect the muscle fibre itself or the muscle membrane.
The pathogenesis of MSDs is complex and can be multifactorial. The following is a list of the more common causes of musculoskeletal disorders in the horse:

Conformational – toed-in/toed-out, poorly balanced feet, and broken hoof-pastern axis have been linked to musculoskeletal injury due to increased stress and overloading of the associated joints and soft tissue structures (Kobluk et al, 1990).

Depending on the area and type of tissue involved, the horse may be presented for mild to non-weight-bearing lameness, joint effusion, reluctance to move, muscle stiffness/atrophy/fasciculations, wound, altered gait, neurological deficits or general ill-thrift. The differentials list is long, so a thorough work-up is critical.
Can trauma or sudden increase/change in work be noted? Management (worming and vaccination history, change in farriery/diet)? Competing abroad?
Presenting complaints will vary immensely. Observe the horse at rest, followed by a clinical exam where you can assess the range of motion of the neck, back and limbs, and palpate for any effusion, focal/diffuse heat, or swelling, comparing left and right to assess for any asymmetry between the two. Hoof test all four feet – this also gives you an opportunity to assess, for example, the solar surface, contracted heels or abnormal hoof growth.
Depending on the presenting issue, all or some of the following may be required:
Rule in/out a myopathy, underlying inflammation, infection, hepatic disease, or specific tests such as adrenocorticotropic hormone or cardiac biomarkers.
Assess in a straight line on a hard surface in walk and trot; evaluate from the front, back and side; and follow by lunging in trot (on a hard and soft surface) and canter (soft surface) when possible. Some injuries have pathognomonic gaits – for example, fibrotic myopathy – while other disorders may require a specific surface/turn/flexion to elicit the lameness. Local analgesia may be used to localise the area of pain if safe to do so, but contraindicated if a fracture is suspected.

Radiographs and ultrasound are available in most practices. A 7.5MHz linear probe with or without a stand-off can be used for most disorders involving the limbs; a 5.0MHz to 2.0MHz curvilinear probe is needed for deeper structures (Denoix, 1999), while a microconvex probe is best for assessing the articular process joints of the cervical vertebrae (Johnson et al, 2017). Practitioners should familiarise themselves with the common images required.
Some lesions may be incidental, so always compare to the contralateral side where possible and remember to treat the horse not the images. Advanced imaging (MRI, CT, nuclear scintigraphy) may be required in horses where an obvious sign of lameness cannot be found on radiographs/ultrasound – for example, suspected stress fractures. Thermography, if available, may indicate inflammatory, vascular or physiological responses, and should be symmetrical between left and right (Fonseca et al, 2006).
Electromyography (EMG) provides an insight into the state of innervation and pathology within a muscle. Surface EMG can assess superficial muscles, relating their activity to changes in gait (Peham et al, 2001; Wijnberg et al, 2010). Needle EMG is required for suspected neurogenic or primary myopathic diseases, and can evaluate very specific areas and individual muscle fibres (Wijnberg et al, 2010).
Synoviocentesis should be performed in all cases where a wound is close to a synovial structure, or where the history indicates a previous joint medication/wound in the area. In abnormal joints, synovial fluid may appear normal yellow to dark orange/red. Septic synovitis is likely with nucleated cell counts greater than 20,000/µl – especially if total protein is greater than 3.5g/dl to 4g/dl (Smith et al, 2019). However, lower counts don’t exclude infection, as fibrin may sequester cells leading to a falsely low cell number. Cytology further aids diagnosis with greater than 90 per cent degenerate neutrophils with or without intracellular bacteria supportive of septic arthritis.
Rule out any dental or oral issues that may be resulting in reduced feed intake.
Muscle biopsy can aid differentiation between muscle atrophy and disuse atrophy (Aleman, 2011), and between inflammatory (infectious, immune-mediated) and non-inflammatory (nutritional myodegeneration, polysaccharide storage myopathy) myopathies (Aleman et al, 2018).
Management should be based around prevention, through routine vaccination and deworming programmes, providing a well-balanced diet (based on growth rate, use, pregnancy and health status), regular farrier and dental check-ups, and removal of hazardous/toxic plants/substances (such as sycamore seeds or ragwort).
This is indicated during acute soft tissue inflammation, as it provides both anti-inflammatory and analgesic effects, and should be for a maximum of 20 to 30 minutes at a time to avoid reflex vasodilation and oedema. Equine spas are an effective way of providing both cold therapy and compression.
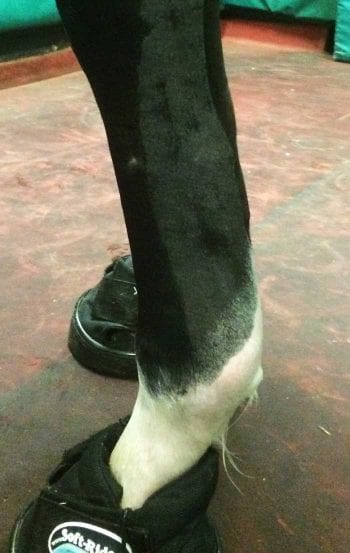
Compression and coaptation reduce inflammation and oedema in the area. In most cases, a modified Robert Jones bandage is suitable, as it provides the pressure and support critical in emergency management of severe soft tissue injuries and fractures. Commercial, specially designed support boots are available and are used routinely in practice.
Any underlying medical conditions, such as infection or PPID, should be managed with systemic therapies (for example, anti-inflammatories or antimicrobials). Fluid therapy should be administered in cases of myopathies; slings may also be required in some cases (Figure 4).
Tendons and ligaments are slow to heal, and can require considerable time and patience. The use of intralesional regenerative medicines (mesenchymal stem cells [MSCs], platelet-rich plasma, autologous conditioned serum) has, therefore, become popular in such injuries to try to reduce convalescence time and maximise healing potential. Polysulphated glycosaminoglycans and hyaluronic acid have conflicting evidence around their efficacy at reducing re-injury rates, and their use has become less popular. Promising results have been seen in the management of OA using allogeneic neonatal umbilical cord-derived MSCs and allogeneic chondrogenic-induced MSCs (Broeckx et al, 2019; Magri et al, 2019).
Physiotherapy and controlled exercise are integral parts of the management of musculoskeletal injuries, and should be tailored to the horse, its use, and the lesion type and severity. Underwater treadmills should also be considered during this time as they aid musculoskeletal conditioning with minimal concussive forces. Serial radiographs and/or ultrasound can help guide timing of increased workloads in the case of tendon injuries or fracture repairs, while serial bloods can be used in myopathies.
Extracorporeal shock wave therapy’s (ESWT) mechanism of action is still unclear, but assumed to produce analgesia through its effect on sensory nerves. ESWT has shown some promising results in alleviating back pain in horses (Trager et al, 2019).
Surgery should mostly be used for debridement of osteochondritis dissecans lesions, repair of traumatic bone injuries, removal of septic processes (curettage of infected bone, lavage of septic synovia structure) and correction of angular limb deformities.
MSDs are common in horses, covering a wide array of injuries and diseases. They require a thorough clinical examination and history taking to narrow down the differentials list. Advances in diagnostic techniques (electromyography, specific biomarkers or advanced imagery) have resulted in earlier diagnosis and treatments.
The use of regenerative medicines in MSDs is very promising in tendon/ligament injuries and OA, but costs still remain prohibitive to most clients.