28 Nov 2022
Lotfi El Bahri MSc, PhD, DVM presents a unique case study that required both swift medical intervention as well as aggressive treatment.
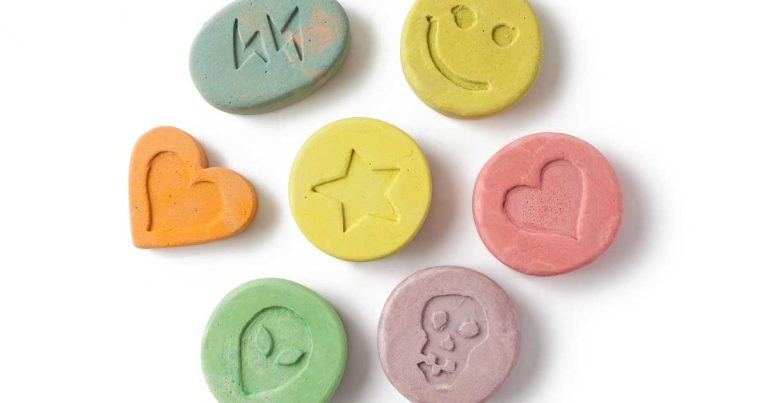
Image: © portokalis / Adobe Stock
You are presented with a three-year-old male pit bull weighing 22.9kg at your emergency veterinary clinic. The dog’s owner said it ingested some quantity of pills of “ecstasy” about a couple of hours previously. The owner noted extreme agitation, vomiting and muscle tremors.
Amphetamine is structurally related to ephedrine – a sympathomimetic alkaloid. The term amphetamines refers to a group including amphetamine and related derivatives by numerous substitutions on its aromatic ring with varying receptor affinities, belonging to a class of non-catechol (lack of two hydroxyl groups on a benzene ring) sympathomimetic amines.
Amphetamines are used medically to treat attention deficit hyperactivity disorder and hyperactivity in children, for appetite suppression and narcolepsy (excessive and uncontrollable daytime sleepiness). Amphetamine substances available by prescription include benzphetamine, dexfenfluramine, dextroamphetamine, lisdexamphetamine and phentermine.
Other types of amphetamines are easily produced and sold illegally for recreational uses such as methamphetamine (N-methylamphetamine, d-Desoxyephedrine), 3,4-methylenedioxy methamphetamine (MDMA, known as “ecstasy” or “ice”), and 4-methylthioamphetamine. These drugs are often used at nightclubs, “rave” parties and clubs “after hours”. Methamphetamine is the second-most used illicit drugs in the world, second only to marijuana.
Amphetamines – powerful, addictive drugs – have become widespread medically and recreationally, and are a significant public health problem; therefore, pets are exposed to increased risk of poisoning.
Intoxication is usually accidental, resulting from the careless handling by the owner of prescription or illicit amphetamines.
It can cause high acute oral toxicity. The oral median lethal doses (LD50s) for amphetamine sulfate and methamphetamine hydrochloride in dogs are 20mg/kg to 27mg/kg and 9mg/kg to 11mg/kg, respectively. Clinical signs are seen at as low as 1mg/kg of lisdexamphetamine dimesylate.
In humans, acute ingestion of more than 1mg/kg of dextroamphetamine should be considered potentially life threatening. The LD50 orally of amphetamine in mice is 22mg/kg. Young animals appear to be more susceptible than adults.
The amphetamines and related derivatives stimulate both the peripheral nervous system and CNS. They cause an increase in biogenic catecholamines, creating a hyperadrenergic state by several mechanisms:
Amphetamines induce cardiovascular toxicity through direct effects on cardiac and vascular tissue. Amphetamines can change the electrical activity of the heart by inhibiting several potassium channels, which tightly regulate cardiac repolarisation; therefore, ensuring stable and consistent action potential signalling.
Amphetamine particularly blocks the cardiac transient outward potassium current (Kto), both in the open and in the rested state.
The Kto is largely responsible for the action potential repolarisation and for the regional differences in action in ventricle. The reduction of the transient outward K-plus current (Kto) caused by amphetamine may facilitate the appearance of ventricular tachycardia and fibrillation, a reported cause of death in amphetamine users.
Methamphetamine directly and immediately inhibits L-type calcium channels by inhibiting calcium ion movements through voltage-gated L-type calcium channels (VGCCs: Cav1.2 and Cav1.3) in cardiac cells, which regulate calcium influx into excitable cells including, importantly, cardiac muscle.
Methamphetamine causes a dose-dependent increase in body temperature by promoting heat generation and suppressing responses that would facilitate heat dissipation.
Hyperthermia can lead to rhabdomyolysis, metabolic acidosis and disseminated intravascular coagulation (DIC).
Clinical manifestations of toxicosis usually develop within one to two hours after ingestion, and are specific, as those seen with sympathomimetic drugs (sympathomimetic toxidrome).
Clinical features may persist for 24 to 48 hours. They include:
Gastrointestinal signs include the following:
CNS signs include:
Cardiovascular signs include:
Death may be caused by ventricular fibrillation.
Laboratory values indicate:
Severe seizures cause rhabdomyolysis, resulting in marked increase in serum creatine kinase levels (reference range in dogs is 0 IU/L to 190 IU/L). Rhabdomyolysis also induces a rapid rise in potassium associated with the development of cardiac conduction disturbances. The released myoglobin caused by muscle damage results in acute renal failure.
Troponin I, biomarkers of myocardial damage, is increased (reference range in dogs less than 0.03ng/ml to 0.07ng/ml).
Hyperkalaemia occurs when serum potassium concentrations exceed 5.5mEq/L. At concentrations greater than 7.5mEq/L, hyperkalaemia is considered life threatening.
Regarding hypoglycaemia, the reference range for blood glucose concentration in dogs is 3.9mmol/L to 6.7mmol/L.
Regarding hyperlactaemia, the reference range for blood lactate levels in dogs is 0.42mmol/L to 3.58mmol/L.
Thrombocytopenia (reference range plaquettes 148.000µL to 484.000µL), prolonged prothrombin time (PT; reference range in dogs is 11 to 14 seconds) and activated partial thromboplastin time (APTT; reference range 60 seconds to 93 seconds) are in relation with DIC.
The ECG of a poisoned patient shows ventricular arrhythmias with QT interval prolongation (normal QT criteria in dogs is 0.15 seconds to 0.25 seconds). Prolongation of the QT interval is associated with high risk of ventricular arrhythmias and sudden cardiac death.
Amphetamine intoxication is a potentially life-threatening emergency and requires immediate intervention. Veterinarians should be aware of the high toxicity of these compounds. No specific antidote exists. Treatment is aggressive, supportive care.
The patient should be managed in an area capable of cardiorespiratory monitoring and resuscitation.
Attention to airway and breathing is paramount. Intubate affected animals and provide artificial respiration with oxygen during convulsions (8L/mn to 12L/mn oxygen concentrations of 50% to 60%). Monitor ECG of the patient.
Convulsions should be controlled and may require attention for more than 24 hours. An IV catheter should be placed.
To control seizures, diazepam (0.5mg/kg to 2mg/kg IV bolus) should be administered and repeated if necessary within 20 minutes (serum half-life in dogs is 2.5 to 3.2 hours) up to three times in a 24-hour period, or 1mg/kg to 2mg/kg rectally.
Do not give diazepam by IM. This is contraindicated in patients with severe liver disease, however.
Alternatively, administer lorazepam (long-acting benzodiazepine 0.2mg/kg IV bolus, because of its high affinity for benzodiazepine receptors in the CNS), or midazolam 0.2mg/kg to 0.4mg/kg IV may be repeated once. When IV access is not available, midazolam can be administered by IM because it is rapidly absorbed by this route.
Ketamine used alone causes muscle rigidity and could potentially exacerbate seizures and tachyarrhythmias, while valproic acid is not recommended (serum half-life in dogs is between 1.5 and 2 hours). Barbiturates and phenytoin are also contraindicated.
If seizures persist or recur, alternatively, administer propofol (3mg/kg to 6mg/kg IV initial bolus) followed by 0.1/kg/min to 0.6mg/kg/min constant rate infusion (CRI). Alternatively, 2% to 2.5% concentrations of isoflurane alone with oxygen can also be used.
For maintenance, use 1.5% to 1.8% concentrations of isoflurane in oxygen.
Severe hyperkalaemia with the ECG changes or symptoms requires rapid correction to prevent significant cardiovascular complications. The treatment of hyperkalaemia requires a combined treatment approach.
Calcium gluconate 10% 0.5ml/kg to 1.5ml/kg slow IV over 10 minutes antagonises the effect of hyperkalaemia on the heart without lowering serum potassium concentrations and may be effective in rhythm disturbances.
It usually starts working within minutes and should last about 30 to 60 minutes. Repeat doses (0.5ml/kg to 1.5ml/kg IV over 5 to 10 minutes) can be administered until a desired effect is noted. The heart rate should be monitored via ECG to ensure rapid administration does not cause bradycardia. If bradycardia develops, halt infusion.
Insulin and glucose shift the intracellular potassium from the blood into cell.
Administer rapid insulin zinc 0.25 unit/kg to 0.5 unit/kg (withdraw with an insulin syringe) slow IV injection always with 2g of glucose per unit of insulin, followed by a CRI of 2.5% glucose at maintenance rates for six to eight hours.
The onset of the hypokalaemic action occurs within 15 minutes and lasts at least four to six hours. Monitor blood glucose and potassium levels.
Glucose at 2.5% may be administered alone to treat hyperkalaemia.
Its mechanism of action is to stimulate endogenous insulin release, which ultimately drives potassium intracellularly. Sole administration of glucose is inconsistent for managing severe hyperkalaemia and is not generally recommended.
Selective beta-2 agonists (such as terbutaline and salbutamol) can be administered as an adjunct therapy for the treatment of hyperkalaemia.
Terbutaline binds to beta-2 receptors in erythrocytes, liver and muscle cells, stimulating adenylate cyclase that converts adenosine triphosphatase (ATP) to 3’5’-cyclic adenosine monophosphate. This stimulates the sodium-potassium ATP pumps, resulting in intracellular K+ uptake.
Terbutaline sulphate can be administered at 0.01mg/kg IV slowly. The onset of action is about 30 minutes following administration, with a duration of action of about two hours.
Many studies show that sodium bicarbonate fails to lower the serum potassium.
Severe hyperthermia can be corrected by external cooling every two to four hours (ice baths should be avoided as these may create hypothermia). This should be stopped when the rectal temperature reaches 39.4°C.
IV infusion is the preferred means of delivering fluids to severely dehydrated animals.
Aggressive fluid therapy with IV sterile sodium chloride 0.9% should always be the first-line management. The volume of fluid needed to correct dehydration is calculated from the following formula: volume (ml) of fluid needed = percentage of dehydration × body weight (kg) × 1,000.
It is recommended that one-fourth to one-half of the estimated dehydration deficit be replaced over the first two to four hours, with the remaining dehydration deficit and maintenance isotonic volumes administered over the subsequent 20 to 22-hour period. Adequate hydration and urine output (1ml/kg/hour to 2ml/kg/hour) should be ensured.
Correction of metabolic acidosis (normal values in dogs is pH less than 7.33; standardised base excess less than −4mmol/L) by sodium bicarbonate 8.4% solution of 1ml/lb to 2.5ml/lb bodyweight CRI, depending on the severity of the acidosis, over a four-hour-period.
Hypoglycaemia can be corrected using 5% dextrose: 40mg/kg IV every 24 hours; blood glucose should be monitored every eight hours.
Administer a potent arterial dilator: nitroprusside sodium: 1 microgram/kg/min to 10 micrograms/kg/min CRI via an IV catheter with fluid pump with continuous blood pressure monitoring. Nitroprusside should only be used for 48 hours because of the build-up of its toxic metabolite, cyanide.
Administer esmolol hydrochloride – a short-acting, IV cardioselective beta-1 – and alpha blockers for rapid control of ventricular arrhythmia: an initial loading dose of 0.25mg/kg to 0.5mg/kg (250 micrograms/kg to 500 micrograms/kg) administered IV as slow bolus over one to two minutes, then followed by a CRI of 10 micrograms/kg/minute to 200 micrograms/kg/minute (dilute before IV injection with 5% dextrose).
Esmolol produces peak effects within 2 to 10 minutes of administration. It is rapidly hydrolysed by red blood cell esterases, with an elimination half-life of nine minutes.
Monitor bradycardia. Selective beta-blockers (such as propranolol, carvedilol and metoprolol) are contraindicated as unopposed, alpha-receptors; mediated vasoconstriction stimulation could result in increased blood pressure and tachycardia.
Cyproheptadine – a non-specific serotonin antagonist – antagonises excessive stimulation of 5-HT CNS receptors and may be useful as adjunctive treatment with severe serotonin syndrome. Administer 1.1mg/kg orally.
Doses may be repeated every four to six hours as needed until signs have resolved. In cases where orally dosing is not possible (severe vomiting), the tablets may be crushed, mixed with saline and given rectally.
Administer canine platelet concentrates lyophilised, or coagulation factors (fresh frozen plasma: 10ml/kg to 15ml/kg) and canine cryoprecipitate lyophilised (one vial for every 12kg of bodyweight).
Emetics are contraindicated as they stimulate seizures. Activated charcoal is not advised (peak absorption occurs within 1.5 hours). Urinary acidification by ammonium chloride is of little value.
Because MDMA is a highly lipid soluble (log P values of 2.15), consider lipid emulsion therapy – an initial IV lipid emulsion (ILE) of 20% 1.5ml/kg IV bolus over one minute, followed by a CRI of 0.25ml/kg/min for the next 30 to 60 minutes.
In non-responsive patients, an additional intermittent bolus can be given IV slowly, up to 7ml/kg. If clinical signs do not improve after 24 hours, discontinue ILE.
ILE 20% preparations are isotonic and can be given by a peripheral vein, or in a central catheter using aseptic techniques.
Enhanced elimination of amphetamines is not recommended. They are lipid soluble weak bases and have large volumes of distribution. The patient should be observed for a minimum of three days (long elimination half-life of MDMA).
Owners should be advised that fruits (such as banana, papaya and prune), orange juice and some biscuits or potatoes (150g potato contains approximatively 620mg of potassium) should be avoided.
Amphetamines have been recognised as emerging aquatic pollutants due to their presence in aquatic ecosystems up to 1µg/L level.