7 May 2012
James Harris takes a look at this condition, and outlines methods to get the most out of the treatment process for everyone involved in such cases.
James Harris takes a look at this condition, and outlines methods to get the most out of the treatment process for everyone involved in such cases
Diabetes mellitus is a commonly diagnosed condition in general practice. Diabetic clinics are considered best practice in the NHS for IDDM, led frequently by specialised nurses. This article discusses the role of the diabetic clinic in small animal medicine and the importance of the qualified veterinary nurse in the development of a strong relationship with the client. A suggested format is discussed for both the initial and longer-term maintenance visits, including discussion of home testing and quality of life assessments. Diabetic clinics are not only beneficial to the pet and client, but also to the veterinary team and business.
In general practice, diabetes mellitus (DM) is commonly diagnosed in dogs and cats.

Under the NHS, where the prevalence of DM is rapidly increasing, patients with insulin-dependent DM (IDDM) are encouraged to visit specialised diabetic clinics in an effort to help them manage their condition better. These visits are typically every three to six months with a nurse specialist and once yearly with a doctor, as well as a once yearly visit to a specialist optician.
Unfortunately, not all clients will commit to treatment for their pets, but for those who do, vets must understand the significant time, emotional and financial commitment they are making. It is essential that, as a progressive profession, we do more than simply teach the client the injection technique and how to store the insulin. In a recent assessment of the psychological and social impact of DM upon both client and pet, there were relatively frequent negative comments regarding the “support from the veterinary team” (Niessen et al, 2010).
Diabetic clinics in most practices are best run by a qualified veterinary nurse (Figure 1). This is particularly important in larger practices, where clients can struggle to see the same staff member repeatedly. The nurse can develop a strong relationship with the client who attends on a frequent basis, becoming more familiar with “normal” for that pet. In this way, trends can be identified more rapidly before they become problematic.
Unlike in the human field, where diabetic nurses undergo specialist training and rapidly develop experience by seeing a large and varied caseload, veterinary nurses have to bring to the clinic a more basic understanding.
However, good communication skills are essential, as well as an understanding of treatment options, appropriate monitoring regimes and knowledge of potential complications and problems in diabetic pets. In humans, treatment outcomes are similar for both practice nurse or GP-led follow up, and similar is expected in the veterinary field (Houweling et al, 2011).
Early introduction of the veterinary nurse into the pet’s care supports her or his value in the team and, with time, the involvement of the veterinary surgeon can be reduced. A number of issues need to be considered at this visit (Table 1) to ensure the client has a good basic understanding of his or her pet’s management from the start.
Frequently, misunderstanding at this early point can lead to longer-term problems, most of which are avoidable with good communication.
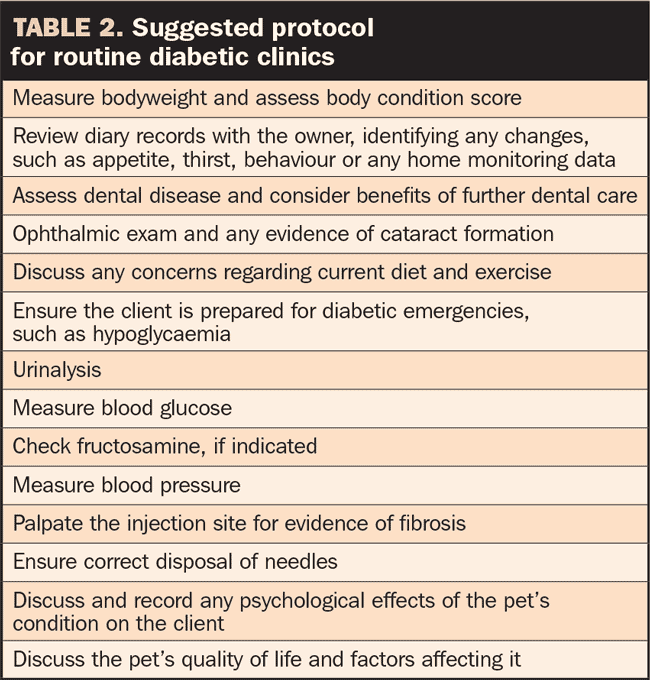
Once the pet’s diabetes is more stable, the nurse clinic focus can change to long-term management. These visits, conducted routinely every one to three months, should include a number of checks and discussion points (Table 2).
A holistic approach is to be encouraged, avoiding fixation on euglycaemia and normalising fructosamine levels. This is a good time to discuss the pet and owner’s quality of life and any specific issues arising from the pet’s medical condition. An online tool, DIAQoL-pet, is under research at the moment (www.rvc.ac.uk/diabetes) and may be available to practitioners in the future to help them identify specific client concerns (Niessen et al, 2010).
A discussion on diet is often best left until the pet has started treatment and the client is coping with the injection regime.
Many clients will have their own experience of managing type-II DM and will be aware of the importance of a fat-restricted, high complex carbohydrate diet, avoiding simple sugars.
The most suitable diet for the diabetic pet depends on numerous factors, in particular bodyweight and body condition score at diagnosis (Figure 2). Obesity is a common predisposing factor in developing DM and can be associated with insulin resistance and poor diabetic control. In obese dogs and cats, the targeted weight loss must be gradual and controlled, necessitating at least monthly visits until the initial targets are achieved.
In dogs, weight loss is best achieved with a high carbohydrate diet with calorie restriction. In cats, the ideal composition and level of carbohydrate is controversial (Kirk C, 2011). Diabetic cats fed on low-carb, high-protein diets are reported as three times more likely to discontinue insulin therapy compared to high-carb products. However, in those cats that continue to require insulin therapy, no significant difference was found between the two diabetic diets, with both types improving glycaemic control.

It appears there is individual variability in response to these diet types and, currently, no obvious clinical or biochemical indicators suggest which might be optimal for the individual diabetic cat.
Low-carb diets are probably not suitable for diabetic cats with concurrent pancreatitis, hepatic disease or renal disease. In general, dietary requirements for other medical conditions take precedence and any dietary change must be done carefully as to ensure no loss of appetite.
Semi-moist foods are best avoided, as they tend to have a greater hyperglycaemic effect due to higher levels of simple sugars and processing humectants.
In underweight dogs and cats, feeding a higher-calorie diet combined with early diabetic control can lead to rapid improvement, but again this needs regular monitoring to ensure the pet doesn’t become overweight.
An assessment of body condition score is a useful adjunct to weight recording and is a simple technique to teach the clients, allowing regular monitoring at home, especially in largebreed dogs.

Many owners are happy to keep a diabetic diary that, even in the most simple format, can be very useful for trend monitoring. Clients, in general, behave honestly and, unlike in teenagers diagnosed with IDDM, false recording is rare.
The diary can also be used to store home-testing data. Traditionally, this has been limited to urine glucose and ketone measurement on a dipstick, but more recently there is a growing interest in home blood glucose testing (Figure 3). In humans, this has been the most important development in managing DM in the past 40 years and has massively improved diabetic control, as well as preventing complications (Petrie G, 2011). The skin prick is well tolerated by the majority of pets and the technique can easily be taught in the clinic, and supported by videos on the internet via YouTube (Table 3).
However, most diabetic dogs and cats do not routinely have their blood glucose measured at home, mainly because of client concerns that it is too invasive and will affect the client-pet bond.
Fortunately, home blood glucose testing is not essential in the majority of diabetic pets, although in some cases, particularly dogs with pancreatitis or a history of diabetic ketoacidosis, it is extremely useful.
Clients doing home blood glucose measurements must understand that, with the exception of hypoglycaemia, changes in the insulin dose should not be performed more frequently than every three to five days.
For many owners, it is best to discuss the results first at the clinic, analysing serial measurements over several days, at different times of the day, before changing the dose or frequency of insulin injections.
Non-invasive blood glucose measuring devices are becoming available for dogs, and these offer an excellent alternative for home testing.
They are more expensive, but are invaluable in difficult-tomanage cases and offer the significant benefit of no discomfort to the pet.
Analysis of a fresh urine sample during the clinic can be very informative, although it may be worth contacting the client the day before the appointment to remind him or her to bring in the sample.
The presence of glucosuria indicates a blood glucose greater than 10mmol/L to 12mmol/L at the time when the bladder was filling. Ketones are indicative of persistent hyperglycaemia and poor diabetic control, and always necessitate further action. Urinary tract infections (UTI) are common in diabetic dogs and cats, suggested by proteinuria and haematuria, and urine culture is warranted when present. UTIs are an important cause of insulin resistance, and must be treated to effect bacterial cure, demonstrated by a negative culture at least one week after the antibiotic course.
Fructosamine is a plasma protein that provides an indication of the average blood glucose in the preceding one to two weeks.
It is a very useful tool in managing diabetic pets, particularly cats, where stress hyperglycaemia makes interpretation of blood glucose measurements in clinic more challenging.
However, as for urinalysis, it must be interpreted in context and, in an otherwise apparently well-controlled pet, the presence of a mildly increased fructosamine alone would not warrant a change in insulin dose.
Diabetic dogs and cats are less likely to become hypertensive or suffer from atherosclerosis than their diabetic owners.
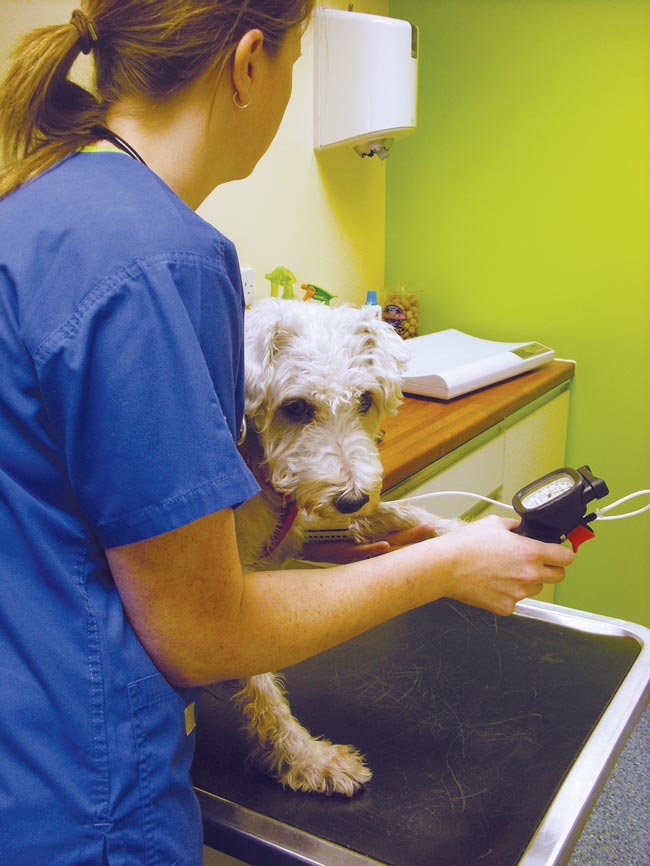
However, where available, blood pressure measurement is still an essential part of the diabetic clinic, due to the severity of the pathology caused and the difficulty in recognising hypertension on clinical examination. Diabetic pets have an increased incidence of renal disease, which may be the cause of hypertension or may result from it.
Pet owners in general are well aware of the importance of blood pressure monitoring in themselves and readily accept it as part of their pet’s treatment. To get useful and accurate blood pressure readings, the nurse must be confident and experienced (Figure 4). Any pets with evident hypertension in the clinic setting should not be started on medication until this has been verified with readings taken as an in-patient, or ideally at home to minimise any “white coat” effect.
A well-run diabetic clinic benefits the client, the pet, the veterinary team and the business as the veterinary staff’s attitude will largely determine the pet owner’s motivation and compliance with treatment.
The client will receive better support and improved communication will give owners a more realistic understanding of their pet’s condition. The dog or cat will have better treatment, reduced risk of complications and, hopefully, a better quality of life.
The veterinary practice also gains, with more satisfied nurses using their knowledge and skills to a higher level, more bonded clients and, potentially, improved financial remuneration. Finally, the hope is that by seeing the pet regularly when it is well, the vet will not be seeing it when it is sick.
The author would like to thank Lucy Davison (MA, VetMB, DSAM, PhD, DipECVIMCA, MRCVS) for her support and advice.