20 Feb 2017
Ben Garland describes surgery to remove a foreign body from the oesophagus, looking at alternative methods, potential complications and recovery.

A 16-week-old male Labrador retriever presented with a suspected oesophageal foreign body after being observed to swallow part of a child’s toy (Figure 1).

The owner reported finding the remains of the child’s toy in the puppy’s kennel – the windmill “blades” and proximal handle were recovered, but the majority was unaccounted for.
On arrival to the clinic, the patient was able to be carried in by the owner. He displayed mild discomfort with extension of the neck, ptyalism and a palpable protrusion of the cranioventral neck just caudal to the larynx.
Physical examination was otherwise unremarkable, with thoracic auscultation, peripheral perfusion, abdominal palpation and mentation all normal.
A pain response was elicited on gentle palpation of the ventral neck and a fixed SC protrusion was noted with lateral tracheal deviation. Oesophageal foreign body was highly suspected and further differential diagnoses at this stage included oesophageal trauma, foreign body, laryngeal trauma, infection, inflammation (for example, insect sting), neoplasia or mucocele (Radlinsky, 2012; Waddell, 2015).
The patient was admitted for radiography under sedation and an IV catheter was placed in the right cephalic vein. Butorphanol (0.1mg/kg IV) and medetomidine (15ug/kg IV) were administered and oxygen delivered via a face mask. IV sedation provided chemical restraint to aid maintenance of the neck position and relieve patient anxiety (Dugdale, 2010).
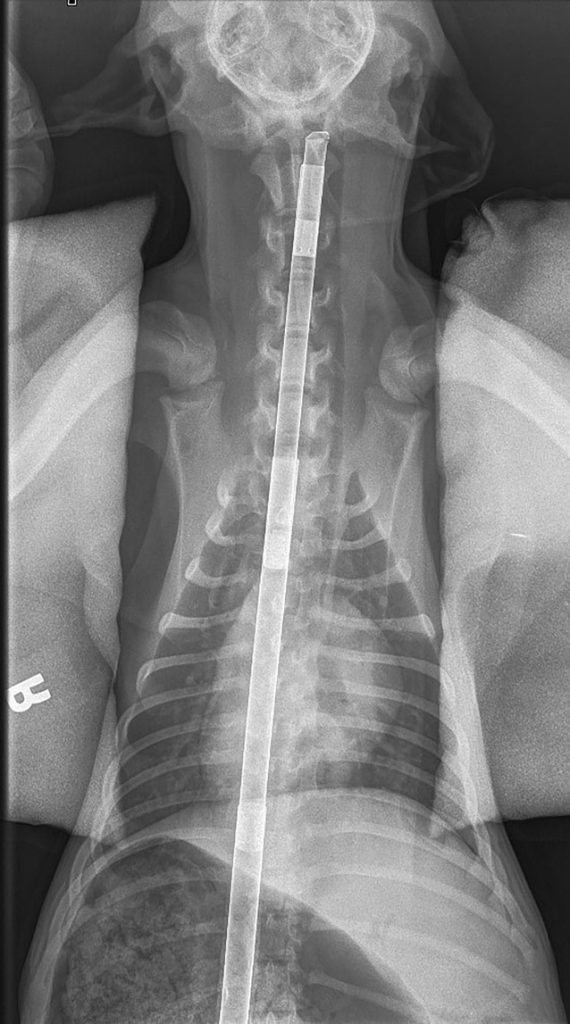
Once sedated, the patient was moved to the radiography suite and positioned in right lateral recumbency. The neck was supported away from the table with foam pads and plain radiographs were taken of the abdomen, thorax and neck (Figure 2).
The patient was rotated into dorsal recumbency, with the neck held fixed and supported with a cradle and sand bags before ventrodorsal thoracic and abdominal plain radiographs were acquired (Figure 3).
The images revealed a radio-opaque, rigid and linear foreign body approximately 1cm in diameter and 46cm in length, originating aboral to the larynx, extending through the oesophagus into the stomach. Contrast views were not required; however, for radiolucent foreign bodies, contrast may be used (Kealy, 1987).

A secondary gastric dilation, presumed due to blockage of the cardia by the object, was also noted. No evidence of other thoracic or abdominal pathology was evident. The use of orthogonal views confirmed the foreign body travelled in the oesophagus, remaining central and dorsal in the thorax. The aboral aspect of the object was rounded and blunt, with the oral aspect sharp. Distension of the oesophagus aboral to the pharynx/larynx was evident and the hyoid apparatus appeared normal on lateral radiographs. Oesophageal perforation was not suspected and oesophageal foreign body with secondary gastric dilation was diagnosed.
Oesophageal foreign bodies are a common finding in cats and dogs (Washabau, 2005). The majority of oesophageal foreign bodies (60%) are caudally located between the heart base and diaphragm due to anatomically limited dilation in this region (Aertsens et al, 2016). West Highland white terriers, Yorkshire terriers and Bernese mountain dogs are over-represented breeds (Gianella et al, 2009; Juvet et al, 2010).
Due to the high motility of the oesophagus and its close association with major blood vessels, access is difficult and complications can be high. Major complications associated with oesophageal surgery are directly related to dehiscence of the surgical wound or injury from the foreign body.
Small perforations may heal well without intervention (Radlinsky, 2012), but lacerations require surgical apposition. Damage, either direct or iatrogenic to the associated large vessels, is of major concern when considering manipulating the object (Aertsens et al, 2016). In this patient, pre-existing intrathoracic damage was considered unlikely due to the blunt nature of the distal end. Most concern was focused on proximal extrathoracic oesophageal damage from the sharp tip ofthe object.
Surgical intervention was immediately planned as the patient was stable and otherwise healthy. Oesophageal mucosal irritation with subsequent ulceration and perforation can readily occur with indwelling foreign objects and prognosis worsens as duration increases (Juvet et al, 2010; Radlinsky, 2012; Washabau, 2005).
Endoscopy was not available, with endoscopic retrieval considered the preferred first option (Aertsens et al, 2016; Radlinsky, 2012; Juvet et al, 2010; Seim, 1988; Washabau, 2005).
Blind retrieval was considered, but inability to visually explore the oesophagus and risk of iatrogenic damage precluded this approach. Discussion was held regarding surgical intervention, considering removal via gastrotomy or oesophagostomy.
Oesophagostomy was chosen, given the risk of iatrogenic damage to the oesophagus and intrathoracic structures by the sharp end of the foreign object if removed via gastrotomy. Risk of contamination from gastric contents was also deemed less likely via this approach. The risk of emesis was considered a potential complication of this approach.
Options were discussed with the owner and informed consent for surgery was given. Potential complications discussed included pneumothorax, haemothorax, postoperative dehiscence, aspiration pneumonia, damage to adjacent structures in the neck, stricture formation, fistulation or diverticula formation (Radlinsky, 2012; Washabau, 2005).
Sedation was converted to general anaesthesia with isoflurane in oxygen induction and maintenance via face mask.
The use of an endotracheal tube (ETT) was strongly considered, providing secure airway management in light of the risk of emesis. However, placement of the ETT was felt to have increased risk of iatrogenic damage to cervical neck structures. Instead, control of the oesophagus after foreign body removal was planned, with ETT placement subsequently. IV fluid therapy was initiated with compound sodium lactate 10ml/kg/hr surgical rate.
Perioperative analgesia was achieved with buprenorphine (0.02mg/kg IV), with full mu-agonists avoided due to increased risk of vomiting and constriction of the cardiac sphincter (Dugdale, 2010). Butorphanol, previously administered, provides OP3 (formerly mu) receptor antagonism and can reduce some of the effects of other opioids where desired (Dugdale, 2010); its use in combination with buprenorphine has been described in dogs (Claude, 2015) and cats (Johnson et al, 2007). Lidocaine (1mg/kg) local anaesthesia was provided SC to the skin of the surgical site, diluted in 0.9% sodium chloride. A clean-contaminated procedure was planned and perioperative antibiosis with amoxicillin-clavulanate (8.75mg/kg IV) was given (Ramsey, 2014).

The surgical site was prepared with the patient in dorsal recumbency. A wide clip from the mandibular ramus to the thoracic inlet was performed before 4% chlorhexidine solution skin cleansing, followed by isopropyl alcohol application (Hutchinson, 2012).
Anatomy, surgical approach and technique were revised from Small Animal Surgery (Radlinsky, 2012) prior to moving to the operating theatre.
The patient was positioned in dorsal recumbency with forelimbs tied caudally and a rolled towel placed under the neck. An impervious disposable drape was placed after a second skin preparation (Hutchinson, 2012) and approach to the cervical neck, as described previously, was performed (Radlinsky, 2012). A 5cm linear skin incision was created over the mid-ventral neck, blunt dissection to the sternohyoideus muscle completed and the muscle bellies separated with further blunt dissection. Gelpi retractors were placed at each end of the incision and the oesophagus was immediately visible, displaced ventrolaterally to the right of the trachea. The thyroid gland, recurrent laryngeal nerve and carotid sheath were also identified in the surgical field.
The oesophagus was visually inspected for trauma on all aspects, as far orally as the laryngeal apparatus. No external evidence of perforation or ischaemia was evident; however, mucosal assessment by this route is not possible. The absence of visually evident oesophageal damage allowed for surgical access over the tip of the object; where compromise is present, incisions should be placed caudally (Radlinsky, 2012).
If required, damaged sections of oesophagus can be debrided, provided no more than one quarter of diameter is removed and culture samples should be obtained (Radlinsky, 2012). Full thickness three-metric polyamide stay sutures were placed oral and aboral to the proposed surgical site prior to isolation with moistened sterile laparotomy swabs.
A stab incision was created over the object on the ventral aspect and lengthened in an oral-aboral direction to approximately 1cm (Figure 4).

Suction of the oesophagus can be performed prior to incision if risk of contamination from oesophageal contents exists. Carmalt forceps were used to grasp the object and gentle traction applied to remove it with minimal resistance (Figure 5).
Minimal gross contamination was noted and gentle lavage of the surgical site with 0.9% sodium chloride solution was performed. Gloves and kit where changed before oesophagostomy closure.
Full thickness simple interrupted sutures of one-metric monofilament polydioxanone suture material were placed, with 2mm spacing and knots placed extralumenally. Simple interrupted patterns are preferred to prevent stricture formation or suture line failure (Radlinsky, 2012; Oakes et al, 1993). In preference, a two-layered simple interrupted pattern would have been performed for superior healing and apposition; however, bursting strength remains highest in a simple interrupted full thickness pattern (Oakes et al, 1993). Manipulation of the oesophagostomy site to facilitate layered closure was difficult, and risk of iatrogenic trauma was considered too high. The option to place full thickness sutures was chosen as a second alternative in this patient and good apposition with watertight closure was achieved. Occlusion and pressure testing with 0.9% sodium chloride solution was used to confirm closure.
Oesophageal support techniques are described (Radlinsky, 2012), including muscular pedicle flaps and patching with omentum, pericardium and gastric wall. These can be used to aid in drainage and revascularisation during healing. Due to the apparent health of the oesophagus and minimal oedema or ischaemia at the level of the oesophagostomy site, this was not performed.
Stay sutures were removed and the sternohyoideus muscles apposed with a simple continuous pattern, followed by SC and skin closure. A light dressing was placed, before recovery in a padded kennel.
Placement of a feeding tube was considered for provision of nutrition, while protecting the surgical site. Options included an oesophageal tube to protect from stretching and direct contact with ingesta or a gastrotomy tube to bypass the oesophagus. Both require further surgery and carry associated risks for placement and management postoperatively. It has been shown withholding food before providing a liquid diet in the well patient leads to full recovery (Washabau, 2005; Seim, 1988) and, in this instance, no tube was placed.
Postoperative management with parenteral drugs was used and an inflatable neck collar was placed to protect the wound from self-trauma.
Antibiosis was continued beyond the perioperative period with amoxicillin-clavulanate (8.75mg/kg SC) every 24 hours for 5 days, buprenorphine (0.02mg/kg IV) 6-hourly for the first 24 hours, and ranitidine HCL (2mg/kg IV) 12-hourly for 24 hours. Fluid intake was maintained via IV fluid therapy and the patient was starved for 24 hours before instigating a strict liquid diet (Washabau, 2005). A convalescence food was used, with the patient’s resting energy requirement calculated as 451kcal (Brooks et al, 2014); 70 × (ideal bodyweight; kg) ^0.75.
Aliquots of 65ml were given on an hourly basis during waking hours and the patient was closely monitored for signs of pneumothorax and other complications over the following 24 hours. The patient was discharged 48 hours after surgery on strict cage rest and food to be provided as a thin gruel in multiple small meals to start the evening. The inflatable collar was to be worn at all times and no neck leads used.
At days 3, 5 and 10, physical exams were unremarkable and the patient had tolerated transition to soaked, then hard food. Comfort levels were good, as assessed by the owner, and on day 10, normal feeding resumed. The owner was advised to monitor for any change in deglutition, demeanour or swelling of the cervical neck region. At two months, the patient was considered to be fully recovered.
This case shows successful management of an oesophageal foreign body removed via oesophagostomy. Alternative options could have been used, if available, and, where possible, the author would recommend endoscopic removal if appropriate.
Oesophageal foreign bodies pose a variety of risks to the patient, based on the nature and location of the foreign body. Careful planning and adherence to good surgical principals is required where surgical intervention is planned.