10 May 2017
Ruth Gostelow discusses the aetiology, treatment, management and monitoring with regards to diabetic feline patients.

Figure 1. An obese cat, which subsequently developed diabetes mellitus (DM).
Diabetes mellitus (DM) is a common feline endocrinopathy, which requires regular veterinary visits and can negatively impact the quality of life of both cats and their owners. Although most feline DM cases resemble human type-two DM, the exact pathogenesis of DM is likely to differ between individual cats, with some cats having forms of DM that resemble “other specific types” of DM in humans. These most commonly include DM secondary to other endocrinopathies or diabetogenic drug treatment.
Differences in the aetiology of feline DM can influence the ideal therapy and prognosis for individual cats. A variety of methods can be used to monitor the quality of glycaemic control in diabetic cats. Newly developed monitoring techniques include the use of clinical scoring systems, quality of life tools and smart device apps. The exact monitoring methods used are likely to differ between individual cats and owners, depending on which techniques are achievable without compromising owner and patient quality of life. This article reviews different methods for monitoring feline diabetics, and discusses how the aetiology of DM can influence treatment and prognosis in certain cats.
Diabetes mellitus (DM) is a common endocrinopathy among domestic cats estimated to affect 0.6% examined at UK primary care practices (O‘Neill et al, 2016).
Caring for a diabetic cat places significant emotional and financial obligations on owners (Niessen et al, 2010), so methods of monitoring a cat’s diabetic control should, ideally, be tailored to the individual pet and owner, to suit patient temperament and lifestyle.
Prognosis for feline DM is variable and likely depends on several factors, including owner dedication, presence of concurrent disease, and how easily good diabetic control is achieved. Some cats with DM can also achieve diabetic remission, which is associated with increased survival times (Callegari et al, 2013), and can greatly improve cat and owner quality of life.
Management practices that promote good diabetic control, while being achievable for individual pets and owners, are likely to decrease morbidity and mortality associated with feline DM. Understanding how the pathogenesis of DM might differ between individual cats can also allow diagnostic testing and treatment plans to be adapted for individual patients.
This article reviews methods for achieving good glycaemic control and monitoring in diabetic cats, and discusses how the aetiology of DM might influence individual cats’ treatment plans and prognosis.


It is increasingly recommended to classify DM in companion animals according to its aetiology, as is done in humans (Gilor et al, 2016a). Most cases of feline DM resemble type-two DM in humans, which results from various factors including genetic susceptibility, environmental risk factors, insulin resistance and eventual β-cell failure (Reusch, 2015).
Feline DM and human type-two DM share several predisposing factors, such as old age, obesity and an indoor, sedentary lifestyle (Slingerland et al, 2009; O‘Neill et al, 2016; Scarlett and Donoghue, 1998; Nguyen et al, 2015). Obesity predisposes cats and people to DM by inducing insulin resistance, although the mechanism by which this occurs in overweight cats has yet to be fully elucidated.
Although most feline diabetics have type-two-like DM, many have a form of DM that would be classified as “other specific types” of DM, using human classification guidelines. The most common of these are DM secondary to other endocrinopathies or diabetogenic drug administration. Approximately 25% of diabetic cats in the UK are estimated to have DM secondary to hypersomatotropism (HS; Niessen et al, 2015).
Feline HS usually results from excessive growth hormone secretion from a pituitary somatotrophinoma (Peterson et al, 1990). Growth hormone’s insulin-antagonistic effects mean most cats with HS are diabetic, and affected cats typically show insulin resistance and a poor response to routine diabetic management (Niessen et al, 2013). Glucocorticoids are likely the most commonly used diabetogenic drugs in veterinary medicine and glucocorticoid therapy is a risk factor for DM in cats (Slingerland et al, 2009). Glucocorticoids might induce DM by promoting insulin resistance, inhibiting insulin signalling and increasing hepatic gluconeogenesis (Rafacho et al, 2014).
Glucocorticoid excess also accounts for how approximately 90% cats with hyperadrenocorticism have secondary DM (Valentin et al, 2014).
Major aims in treating feline DM are to minimise diabetic clinical signs while avoiding complications, such as hypoglycaemia and ketoacidosis (Sparkes et al, 2015).
Some diabetic cats can discontinue medical diabetic therapy and enter a state of diabetic remission (Nelson et al, 1999). Remission is often attributed to improvements in the reversible components of glucotoxicity, which refers to the deleterious effects of persistent hyperglycaemia on β-cell survival and function (Bensellam et al, 2012). Achieving prompt, effective glycaemic control is, therefore, suggested to increase the chance of remission in diabetic cats (Marshall et al, 2009).
However, remission is also likely to be encouraged by management protocols that promote better insulin sensitivity, such as weight loss and discontinuation of diabetogenic drugs. Although remission is highly beneficial, it is unlikely all diabetic cats have the potential to enter remission, making it an infeasible treatment goal for many cats and owners.


There is some evidence dietary carbohydrate restriction improves glycaemic control in diabetic cats (Bennett et al, 2006). Recent guidelines on feline DM management, therefore, recommend feeding a high-protein, low-carbohydrate diet, unless prevented by other, concurrent diseases (Rucinsky et al, 2010; Sparkes et al, 2015).
Feeding a canned/wet diet is likely to offer more effective carbohydrate restriction than feeding a biscuit-based diet because dry foods typically contain a higher carbohydrate content than the equivalent canned/wet version.
Preventing DM-associated weight loss is an important goal in managing feline DM. However, controlled weight reduction is likely to aid diabetic control in overweight cats by reducing obesity-associated insulin resistance (Hoenig et al, 2007; Figure 1). Body condition and weight should be frequently monitored in all diabetic cats.
A 9-point scoring system has become widely used to assess body condition in feline patients (Bjornvad et al, 2011). Several morphometric formulae have also been developed to estimate percentage body fat (feline body mass index) from body measurements, which are easy to obtain in practice (Butterwick, 2000; Witzel et al, 2014). Figure 2 shows a cat having measurements taken for body mass index calculation using one of these formulae (Butterwick, 2000).
Unlike people with type-two DM, most diabetic cats cannot achieve good glycaemic control with dietary therapy alone (Nathan et al, 2009; Reusch, 2015).
Twice-daily insulin treatment provides the greatest potential for effective glycaemic control and guidelines recommend diabetic cats are treated with long-acting insulins, or insulin analogues, rather than intermediate-acting insulins, such as porcine lente insulin (Sparkes et al, 2015; Rucinsky et al, 2010).
The long-acting insulin protamine zinc insulin (PZI), and long-acting insulin analogues glargine and detemir, have longer duration of action than porcine lente insulin in healthy cats (Gilor et al, 2010; Marshall et al, 2008), so might offer superior glycaemic control in feline diabetics.
Between 2008-16, no veterinary-licensed long-acting insulin was available in the UK. However, a human-recombinant PZI has now launched for use in feline diabetics and should be considered the first-line choice of insulin therapy for newly diagnosed diabetic cats in the UK, based on current recommendations.
The sulphonylurea, glipizide, is the oral antihyperglycaemic agent most commonly used as a sole therapy for feline DM. Sulphonylureas decrease hyperglycaemia by promoting β-cell insulin secretion. Glipizide causes clinical improvement in up to 40% of treated cats, but a substantial proportion fail to respond to therapy or experience adverse effects (Gostelow et al, 2014). Oral antihyperglycaemic agents should, therefore, not be used in preference to insulin therapy and are only recommended when owners initially refuse insulin treatment (Sparkes et al, 2015).
Medications based on the incretin hormone glucagon-like peptide-1 (GLP-1) are widely used for type-two DM treatment in people and are generating interest for the treatment of type two-like DM in cats (Gilor et al, 2016b). Endogenous incretins are released from the gastrointestinal tract and potentiate insulin secretion following nutrient ingestion. GLP-1 is shown to enhance insulin release, inhibit glucagon secretion, inhibit gastric emptying, enhance satiety and might also encourage β-cell proliferation. These actions make it an attractive therapeutic in type-two diabetic patients, who would also frequently benefit from weight loss.
Exenatide is an injectable GLP-1 agonist that increases insulin secretion in healthy cats (Padrutt et al, 2015). A small pilot study examined whether adjunctive long-acting exenatide increased remission rates in newly diagnosed diabetic cats treated with insulin glargine and low-carbohydrate diet (Riederer et al, 2016). Although more exenatide-treated cats achieved remission or good diabetic control, differences between groups did not reach statistical significance, possibly due to small sample size. Further investigation into whether GLP-1 agonists are beneficial in feline DM appears warranted. The RVC is recruiting for a randomised trial examining whether adjunctive, long-acting exenatide therapy increases remission rates in recently diagnosed diabetic cats.
Other measures to improve insulin sensitivity are also likely to encourage good diabetic control and remission. Such measures include promotion of weight loss in overweight cats, as discussed above, and withdrawal or avoidance of diabetogenic drugs. Recent glucocorticoid therapy is associated with a greater likelihood of remission in diabetic cats (Roomp and Rand, 2009). This is likely to be because glucocorticoid-treated diabetic cats experience an improvement in their glucose tolerance once the effect of their steroid therapy wanes.
The presence of concurrent or underlying disease can also affect a diabetic cat’s response to management. Cats with HS-associated DM typically show a poor response to diabetic management, but can achieve improved diabetic control or remission when treated with therapies that successfully reduce their excess growth hormone production (Niessen et al, 2013). In total, 78% of cats with HS-associated DM achieve diabetic remission following hypophysectomy (surgical pituitary excision; Kenny et al, 2015), and improved diabetic control and remission can also occur after treatment with the somatostatin analogue, pasireotide (Gostelow et al, 2017).
Similarly, cats with DM secondary to hyperadrenocorticism can experience improved diabetic control when treated with trilostane (Mellett Keith et al, 2013), and diabetic remission when treated with radiotherapy or hypophysectomy (Meij et al, 2001; Valentin et al, 2014). The specific therapy required in these cases means affected cats should, ideally, be identified promptly, so appropriate treatment can be implemented. The RVC is conducting a trial into a novel therapy for cats with HS-associated DM.
Quality of diabetic control is best assessed via various methods, including in-clinic blood glucose curves, serum fructosamine measurement, home blood glucose monitoring (HBGM), monitoring of bodyweight and body condition (aforementioned), and severity of clinical signs. The most appropriate monitoring techniques may differ between individual cats and owners.
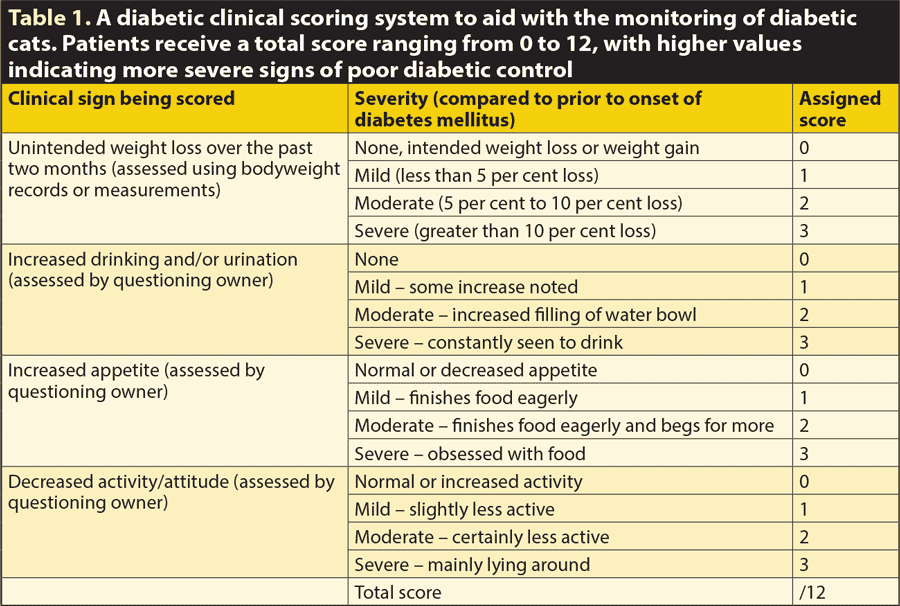
Owner-reported clinical signs, and perceived quality of life, are important measures of treatment success. A clinical scoring system (diabetic clinical score) has been validated for use in diabetic cats (Venzon Varela et al, 2016; Table 1), and using such scoring systems can help standardise history-taking in diabetic patients. Quality of life tools are frequently used when monitoring diabetic people, and a quality of life tool is also available for use in diabetic cats and dogs (Niessen et al, 2010).
Incorporating these scoring systems into a diabetic cat’s monitoring programme can help to quantify changes in both clinical signs and quality of life, which are usually only judged subjectively.
HBGM can be successfully introduced to many diabetic cats (Kley et al, 2004). The above video demonstrating HBGM technique, produced by the RVC’s diabetic remission clinic, can be shown to cat owners:
Home-monitoring might improve diabetic control and recognition of hypoglycaemia. Avoiding in-clinic curves is likely to decrease patient stress and curves performed at home might be less affected by stress hyperglycaemia (Rand et al, 2002). Diabetic cats monitored with HBGM might also be more likely to achieve remission (Kley et al, 2004), although it is unclear whether this is due to improved diabetic control or better recognition a cat is persistently normoglycaemic.
Many owners desire a greater sense of control over their cat’s DM (Niessen et al, 2010) and several smart device apps are now available to aid owners and vets in the management of canine and feline diabetics (Figure 3). Apps also allow owners to record HBGM data and can generate data reports, which can be discussed at veterinary re-examinations.

DM is likely to differ in aetiology between individual cats. Recognising these differences can aid vets in advising owners on the optimum treatment protocol and prognosis for their cat. Ensuring monitoring protocols are achievable for individual cats and owners is likely to improve long-term outcome by optimising patient and owner quality of life.
For details on the RVC‘s trials into long-acting exenatide or hypersomatotropism, email [email protected] or telephone 01707 666 605.