19 Nov 2018
Bob Partridge considers the causes of bad breath – with dental disease the most common.

Different authors cite halitosis in pets as being a rare or common presenting complaint to veterinary surgeons. In the author’s experience it is rare as a presenting complaint, but commonly discovered in the history-taking process.
My most memorable case of halitosis as a presenting complaint was a bichon frise, whose owner’s primary reason for seeing me was because friends no longer visited her house, owing to the level of her pet’s halitosis. I felt this was understandable as I turned up the ventilation to “gale force” to continue the consultation. While this was an extreme example, we do tend to regard halitosis as something of a laughing matter, but should we?
In humans, the cause of more than 90% of halitosis cases is dental disease. We infer the same is true of our veterinary patients (despite their many differences in oral pathology), so I shall only briefly consider other causes at the end of this article.
The major agents producing halitosis in people and pets are volatile sulphur compounds (VSCs), such as hydrogen sulphide (H2S) and methyl mercaptan (CH3SH). The levels of these agents can be measured using a portable sulphide monitor and, in a paper, good correlation was demonstrated between those results and those of organoleptic assessment (Hennet et al, 1995). If you are looking for a job to avoid, organoleptic assessment is performed by a panel of experts sniffing dog’s breath. The highest levels of VSCs were found to occur in the morning – probably linked to a reduced overnight salivary flow and increased bacterial loading following stagnation overnight.
VSCs are produced from the breakdown of protein material originating from blood, gingival crevicular fluid, saliva, food, exfoliated cells and plaque. The total VSC and relative methyl mercaptan levels were highest when gingival pockets were deepest or when bleeding occurred on probing.
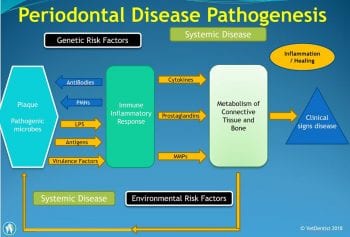
Rather than VSC levels increasing as a result of the development of periodontal disease, they may play an active part in its pathogenesis. Periodontal disease is recognised to be the result of a complex interaction between pathogenic microbes and, importantly, the host’s response, which may be more destructive. Figure 1 illustrates some of the factors involved.
VSCs have been shown to increase the permeability of both oral mucosa and, specifically, gingival crevicular epithelium (the tissue lining the gingival pocket) by affecting the basal membrane, the intercellular matrices and damaging disulphide protein bonds. These reactions are base-catalysed, being encouraged in a more alkali environment. Salivary pH of dogs is around 8.5 – significantly higher than in humans.
The increased permeability of the tissues can allow penetration of lipopolysaccharides, prostaglandins and even bacteria through the tissues. VSCs also induce interleukins – escalating the production of prostaglandins and other inflammatory mediators.
VSCs can cause cell death of both epithelial and fibroblast cells – also affecting protein metabolism and cell migration. A net decrease in collagen levels of 70% has been reported – this may be a significant factor in the development of periodontitis.

VSCs also have an effect on alveolar bone. Differentiation of macrophages into osteoclasts is encouraged and, conversely, apoptosis is induced in osteoblasts. The net result of this is to encourage periodontal bone loss – a key feature of periodontal disease, with the loosening and displacement of teeth (Figure 2).
VSCs are primarily responsible for dental halitosis. Halitosis should not be ignored, as the high levels of VSCs may not be just symptomatic of dental disease, but be actively responsible for deteriorating periodontal health.
The core treatment is effective oral hygiene. This must begin with a full professional oral assessment under anaesthesia, radiographic evaluation of periodontal bone structures, probing periodontal pockets, charting, removing both supragingival and subgingival calculus, and plaque. This may require gingival flap surgery to permit effective exposure. The tongue may need to be cleansed to remove plaque and VSCs from the crypts. Extractions, where required, polishing then establishing prevention. This might begin with the application of a veterinary dental sealant to the periodontal pockets during the procedure.

Oral mouthwashes using Zn++ have been shown to be effective at blocking some of the damage caused by VSCs. Chlorhexidine products remain the standard oral antiseptic, although beware of some containing xylitol. Daily tooth brushing is the essential backbone of any treatment and should be encouraged for all patients. Prescription dental diets, chews and water supplements should be assessed for effectiveness, and the Veterinary Oral Health Council’s website (www.VOHC.org) is a useful resource for this.
Fractures that expose the pulp canal are referred to as “complicated”. In these cases, pulpal death will occur in most cases with necrosis of the pulpal tissues. While bovine cleansing represents a far greater volume of necrotic material, a necrotic tooth in a confined space can produce similar olfactory responses.
In the author’s dental referral practice a “sniff test” has been developed to determine the degree of necrosis of the pulp contents. An unsuspecting student is requested to sniff the extracted pulp contents and the degree of necrosis is measured by the distance in metres of the resultant recoil (Figure 3).
The most common trapped foreign body is a piece of wood stuck on the roof of the mouth between the upper carnassials. Owners may be unaware of the problem until the resultant tissue damage and necrosis leads to severe halitosis (Figure 4).
Increases in blood uric acids levels – as a result of kidney disease – produce ammonium-like breath, or a “bad fish” odour.
Liver disease can result in an increase in raised ammonium levels that can be excreted into expired breath. End-stage liver disease can be associated with foetor hepaticus – a sweet odour of “dead mice” linked to the build-up of volatile aromatic compounds from decreased metabolism.
The pooling of food and saliva, due to megaoesophagus, can result in a fetid smell to the breath.
Dilation of the bronchi, and stagnant pooling of mucus and debris in the airways – often as a result of chronic bronchitis – can lead to halitosis.
Eructation can result in transient halitosis. Halitosis has also been linked to Helicobacter pylori infections and gastroesophageal reflux. In cases of haemorrhagic gastroenteritis the breath is characteristic in its odour of changed blood – if it can be isolated from the smell of any faeces.
Ulcerating tonsillar tumours, especially melanomas, can create fetid halitosis.
Lip fold pyoderma can often be presented as halitosis (Figure 5).
While human problems of the previous night’s curry or an overindulgence of garlic should not be an issue for our veterinary patients, many dog owners will have experienced the “delights” of their pet having indulged in coprophagia.
Many vets will have experienced the dying dog or cat smell of a patient at the end stage of systemic tumour growth. At a far earlier stage, specific odours appear to allow medical detection dogs to alert our colleagues in human medicine to potential problems.