25 Jun 2024
Genaro Vargas and Guillaume Albertini advise on why this complication can occur, what to treat it with and how the object can be surgically removed.

Image © VictoriaEmerson / Adobe Stock
Microchip insertion into the vertebral canal is a rare, but reported, complication from microchip implantation. Clinical signs are often peracute in nature, with most owners reporting paresis and ataxia immediately after microchip implantation. Following a physical and neurological exam, once the microchip is believed to have penetrated the vertebral canal, radiographs and computed tomography are used to confirm diagnosis and identify the precise location of the lesion as well as assess the surrounding structures.
Surgical removal is usually attempted, but medical management can also be implemented if it is deemed detrimental to remove the microchip. With both treatment options, patients experience an improvement of clinical signs as time progresses. However, neurological deficits rarely completely resolve. Despite this, patients can continue to have a good quality of life.
A one-month female shih-tzu that presented for further investigations following a peracute onset of tetraparesis, general proprioceptive ataxia, and proprioceptive deficits immediately after microchip implantation by a non-veterinary professional. Initial physical exam was unremarkable.
On neurological examination, the patient had a normal mental status. She also had a wide-based posture, and, on gait assessment, she was ambulatory tetraparetic with generalised proprioceptive ataxia. Postural reactions were delayed to absent in both the left thoracic and pelvic limbs, but were normal in both right thoracic and pelvic limbs. Spinal reflexes were normal in all four limbs. Assessment of the cranial nerves was unremarkable.
On palpation of the head and spine, no obvious discomfort was perceived. The lesion was localised to C1-C5 spinal cord segments lateralised to the left. Based on the history, the main differential diagnosis was traumatic disease secondary to microchip implantation.
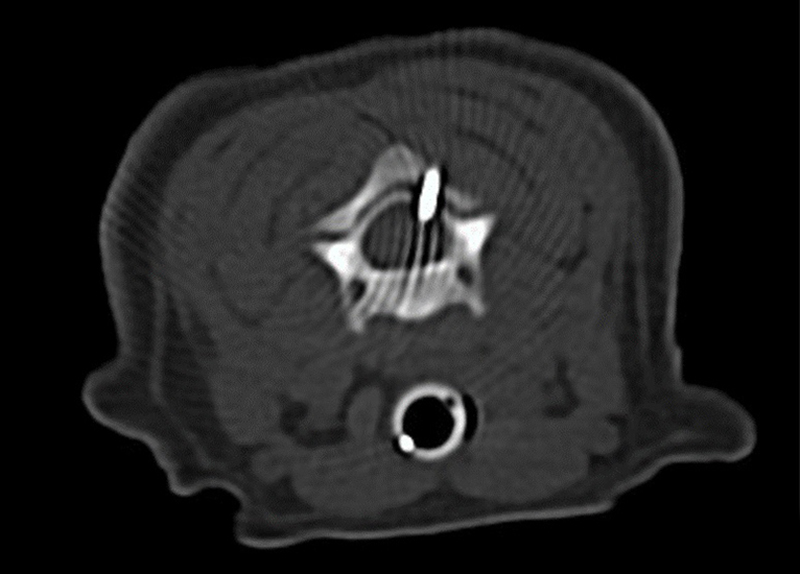
At presentation, PCV was 35% and total solids was 6.0g/dL. No further bloodwork was performed. Pre-referral left lateral, right lateral and ventrodorsal full body radiographs localised the microchip at the level of C2-C3 vertebrae. CT imaging from C1 to T2 vertebrae was used to identify the exact position of the microchip, and confirmed the location at C2-C3 interarcural space, entering from the left dorsal aspect (Figure 1).
The patient was premedicated with methadone (0.2mg/kg IV; Comfortan, Dechra) and medetomidine (3μg/kg IV; Sedator, Dechra) followed by induction with alfaxalone (1ml IV; Alfaxan, Jurox). Perioperatively, the patient received cefuroxime (20mg/kg IV; Zinacef, Sandoz). No local blocks were performed. Blood glucose was carefully monitored due to the signalment of the patient. Removal of the microchip was performed via dorsal exposure of the C2-C3 vertebrae. The skin and superficial fascia were incised to reveal the aponeurosis of the trapezius and rhomboideus muscles, which were then divided in the midline. To prevent a haematoma, the bleeding was controlled with bipolar cautery. The nuchal ligament was retracted and the rhomboideus and splenius muscles were incised. The microchip was found within the ligamentum flavum and was removed without complications. The microchip was then reimplanted subcutaneously.
Postoperatively, the patient received a constant rate infusion of ketamine (2μg/kg/min IV) as well as a single dose of meloxicam (0.1mg/kg IV; Metacam, Boehringer Ingelheim), which was continued orally at home for seven days. Antibiotics were not continued postoperatively.
The patient recovered from the general anaesthetic without complications. On neurological examination 12 hours postsurgery, the patient remained tetraparetic with lateralisation to the left, but as ambulatory and able to urinate and defecate consciously. As the patient was comfortable on oral treatment, she was discharged the following day.
The patient returned for a follow-up consultation four-and-a-half weeks after initial presentation. The owner described the patient as more active, but still had weakness on the left thoracic and pelvic limbs and occasionally fell over.
On neurological examination, the patient was mildly ataxic when turning and continued to have a wide-based stance. Postural reactions were mildly delayed in the left thoracic and pelvic limbs. The cervical spine was not painful on palpation or manipulation. The rest of the neurological examination was normal.
This case describes surgical management of microchip misplacement in a puppy. The purpose of this review is to highlight the consequences of iatrogenic spinal cord injury secondary to microchip misplacement, as well as outline current investigation methods and management.
In the UK, microchipping has been compulsory for dogs since 2015. For cats, it became compulsory from 10 June 20249. The microchip is implanted subcutaneously in the dorsal midline of the animal between the shoulder blades to minimise the risk of migration1.
Complications of microchip placement include inflammatory reactions, and even tumours such as liposarcomas or fibrosarcomas2,18, but when the microchip is placed within the spinal canal it can manifest as neurological deficits1.
Insertion of the microchip into the spinal canal is a rare complication as it has only been reported in a small number of cases4,6,7,8,11,13,15,16. Although it can happen to any animal, small dog breeds or lightweight animals seem to be more predisposed4, as was the case with this patient.
Clinical signs attributed to aberrant microchip insertion include pain, proprioceptive deficits, ataxia, paresis, and plegia with or without intact nociception and, in extreme cases, death12,17. Proprioceptive deficits were reported in all cases, and in most lateralisation of the proprioceptive deficits was seen, which would be associated with the relative location of the microchip.
The clinical signs manifest almost immediately after insertion in the majority of cases4,6,8,11,13,15,16, but they can also manifest years after the microchip has been implanted6. In one case regarding an alpaca, death was reported from suspected neurogenic shock from microchip insertion into the spinal cord17.
A basic profile, including complete blood count, serum biochemistry and urinalysis, can be performed, but in many of the cases, blood work was excluded. In the cases where a basic profile was performed, significant changes were not reported and any deviations from normal limits were determined to be due to the young age11,13,15. Because paediatric patients have an underdeveloped liver as well as poor glycogen, blood glucose needs to be carefully monitored10.
The modality of choice for initial investigations regarding a misplaced microchip are radiographs4,6,7,8,11,13,15,16. With cervical radiographs, the microchip can be easily identified and the surrounding structures can be immediately assessed. However, for exact location and a more thorough examination of surrounding structures, advanced imaging such as computed tomography is preferred and has been widely used4,7,11,15.
Recently, fluoroscopy has successfully been used perioperatively in aiding with the localisation and removal of the microchip8.
In these cases, MRI would be inappropriate as the metallic microchips can produce susceptibility artefacts in the surrounding areas, potentially interfering with interpretation of the image5,13,14.
Furthermore, the MRI has the potential to cause thermal and kinetic damage to the surrounding structures from the microchip being subjected to a strong magnetic field16.

Currently, no preferred method of management for aberrant microchips exists11,15, but most cases undergo surgical management in an attempt to resolve the clinical signs. A dorsal approach is usually implemented after localising the lesion with the help of diagnostic imaging6,7,8,11,13. In most cases, the microchip could be easily visualised after dissection of surrounding structures and removed with minimal traction6,8,11,13. In more complex cases, a dorsal laminectomy13 or hemilaminectomy16 was implemented. Perioperative antibiotics are used in all reported cases, but their use is inconsistent postsurgery.
In at least two cases, it was determined that attempted removal of the microchip would result in further injury to the spinal cord, thus worsening the clinical signs4,15. In one case report, surgeons attempted removal of the microchip, but were unable to dislodge it. However, because adequate decompression of the spinal cord was achieved, the microchip was left in place15.
Neurological signs continue to be present immediately postsurgery, but improve with time, as reported in their follow up exams6,7,8,11,13,16. In the medically managed cases, progressive improvement of clinical signs was noted4,15.
Regardless of surgical or medical management, none of the cases made a complete recovery and a degree of neurological deficits was still present4,6,8,11,13,15,16. One case report that followed up with the patient 11 months postsurgery stated that the patient still had residual paresis of the left thoracic limb13. Furthermore, one case that opted for medical management reported that 16 months after presentation, the patient was neurologically stable and continued to have a good quality of life15. Unfortunately, due to a lack of long-term follow-up reports, the current literature does not highlight the long-term implications of either surgical or medical management.
In some of the reported cases, including this case, the microchip was placed by people that had not been trained to do so4,13. Although it is best for licensed veterinarians, and people under supervision of licensed veterinarians, to implant microchips3, it should be noted that anyone may implant a microchip inappropriately.
If it is suspected that a microchip has been placed near or within the vertebral canal, a thorough history, physical examination and neurological examination should be undertaken. An emphasis should be put on how quickly the clinical signs manifest and if clinical signs have progressed. It should be noted that in most cases, neck pain may not be discerned.
Radiographs and computed tomography should be used to precisely localise the microchip as well as assess neighbouring structures. Despite surgical or medical management, appropriate pain relief should be used, as well as have periodic follow ups to monitor recovery and improvement of clinical signs.
It is important to understand and for the owners to be made aware that, despite removal, it is unlikely that clinical signs will completely resolve. Furthermore, if surgical management is chosen, owners should be warned that clinical signs may worsen after microchip removal. However, it is important to note that, regardless of management choice, some improvement in clinical signs can be expected and patients can continue having a good quality of life.