24 Mar 2017
Karen Perry describes two new approaches to stabilising the luxated patella in dogs, as well as a new form of subsequent pain relief post-surgery.
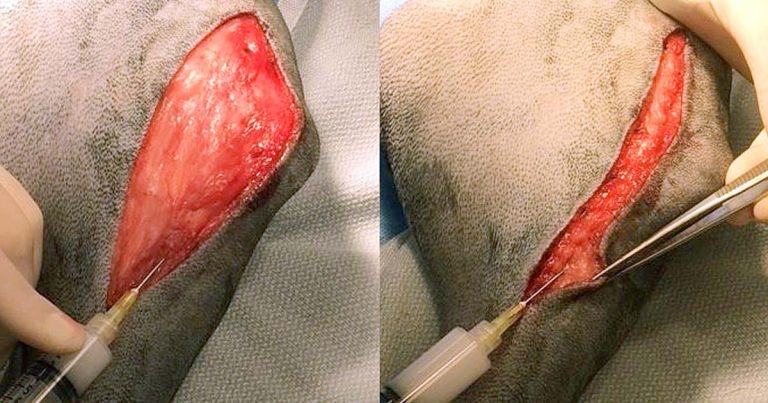
Figure 3. Intraoperative photograph demonstrating the injection technique for a bupivacaine liposome injectable suspension at multiple levels during closure (see also a short video of this technique available as supplementary online material).
Stifle surgery is commonly performed in small animal practice, with both medial patellar luxation and cranial cruciate ligament disease being frequently encountered. While the majority of cases can be treated successfully with traditional surgical techniques, for select cases, additional options can be useful to facilitate a complete return to function and comfort.
Two advances available to assist in stabilising the luxating patellae, trochlear groove replacement and the RidgeStop implant are discussed here. Another important consideration following stifle surgery is the provision of adequate perioperative analgesia. Clinical evidence in dogs indicates multimodal analgesia provides the most effective relief from postoperative pain and a new addition to the armoury, in the form of a bupivacaine liposome injectable suspension, is also reviewed.
Medial patellar luxation (MPL) is one of the most common orthopaedic conditions in dogs1,2. The associated anatomic abnormalities have been extensively reviewed, yet remain poorly understood3-10.
Conventional surgical treatment now focuses on improving alignment of the quadriceps apparatus and stability of the patella via trochleoplasty and TTT, in conjunction with soft tissue reconstructive procedures that balance tension within parapatellar soft tissues, including medial release and lateral imbrication techniques. Despite this, reluxation still occurs in 8% to 12% of cases12-14.
Failure to recognise femoral varus as a factor contributing to quadriceps mechanism malalignment has been suggested as a potential cause of suboptimal outcome or reluxation13,15,16. It has been suggested corrective distal femoral osteotomy (DFO) should be performed when femoral varus is excessive. However, most canine femora have some degree of varus, the degree of which appears to vary both in and between breeds15,17-21, and the degree to which femoral varus is excessive and subsequent indications for DFO are not well defined. Previous publications have advocated DFO when femoral varus angles exceed 10° or 12° 15,18-20,22.
Chronic instability and erosion of the femoropatellar joint surfaces result in lameness and progressive OA. While osteochondral trochleoplasties have been used to deepen the trochlear groove and enhance patellar stability, these are not feasible when osteophytes and cartilage erosion have severely damaged the trochlear groove (Figure 1).
In these situations, another option is needed. One available option is a trochlear groove replacement prosthesis. This is a two-component implant comprised of a base plate and a trochlear prosthesis:
The base plate is made of perforated titanium and coated with a glow discharge anodisation, with calcium phosphate incorporated to promote osseous integration. Three conical holes in the base plate match with three
conical feet on the trochlear prosthesis. Depending on the size of the base plate, it is secured to the bone using either two or four titanium alloy bone screws.
The trochlear prosthesis is made of grade five titanium; it is anatomically shaped (like a trochlear groove) on the upper face, highly polished and treated with amorphous diamond-like carbon coating to provide a very low coefficient of friction and a scratch-resistant surface. The trochlear prosthesis has three conical feet that match the conical holes in the base plate and it is attached by aligning the feet with the holes and then tapping lightly with a hammer to achieve press-fit locking.
The prosthesis is available in 10 sizes and selecting the appropriate one is important to achieve optimal results. Oversizing of the prosthesis can lead to soft tissue impingement with capsule tension and associated thickening23. If the patella groove is too wide for the patella, the patella may tilt within the groove, although the clinical relevance of this is uncertain as lameness and stifle pain have not been associated with this finding in the small number of cases reported23.
Initial selection is based on a mediolateral radiograph of the stifle using a transparent template over the radiograph. The correctly sized implant will sit such that the base of the patellar groove replacement implant is aligned with a line drawn from the point of origin of the long digital extensor to the most proximal aspect of the trochlea23. However, the final decision regarding appropriate size will be made intraoperatively, so having a selection of sizes available and sterile is recommended.
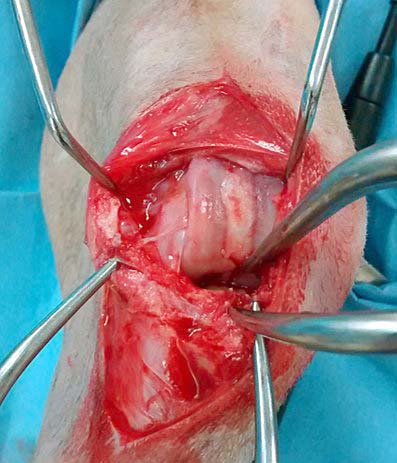
Surgery to place the prosthesis is performed via a parapatellar arthrotomy. Following reflection of the patella, an osteotomy of the femoral trochlea is performed parallel to the frontal plane using an oscillating saw. The osteotomy starts distally at the level of the origin of the long digital extensor tendon and ends proximally at the proximal end of the trochlea. Following the osteotomy, the bone surface is rasped to make it as flat and uniform as possible prior to fixation of the base plate.
A trial prosthesis (available in all 10 sizes) is positioned on the osteotomy surface; an appropriately sized prosthesis results in the proximal and distal borders of the prosthesis matching with the corresponding edges of the osteotomy. With the trial prosthesis in place, the patella is reduced and the stability of the patella and tightness/laxity of the parapatellar soft tissues is assessed. Additionally, the patella must be verified to fit inside the groove of the trial implant.
If alterations need to be made, these may include using a larger or smaller trial prosthesis or removing an additional slice of bone from the osteotomy site. The prosthesis can also be moved further proximally or distally to enhance patellar stability. Once the correct position for the prosthesis is determined, the bone can be gently marked with an osteotome to ensure placement of the base plate in the correct position.
The base plate is then secured to the bone using two or four screws depending on the size of prosthesis selected and the trochlear prosthesis is press-fit to the base plate by aligning the conical pegs with the corresponding holes in the base plate and tapping firmly using a Teflon hammer. It is important to ensure a complete press fit at the time of implantation, as dislodgement of the trochlear prosthesis from the base plate has been reported, which necessitates revision surgery23. The patella is then reduced and stability and range of motion of the stifle assessed.
Occasionally, the patella may be too wide or flat to seat appropriately within the trochlear of the prosthesis. In these cases, partial parasagittal patellectomy may be required. To achieve this, the width of the trochlear is measured and compared to the width of the patella at the widest point. With the patella reflected and rotated to expose the underside, small slivers of bone can then be removed from the medial and lateral aspects of the patella as required to allow seating within the trochlear. Lateral imbrication or medial release can be performed routinely as for standard MPL stabilisation.
In addition to having the capacity to restore function to dogs with severe femoropatellar OA, trochlear groove replacement offers some potential advantages that may facilitate treatment of MPL. Due to the tall ridges and smooth contours of the prosthesis when compared to a traditional recession trochleoplasty, it has been postulated balanced tracking of the patella is more likely to occur with trochlear groove replacement23. The smooth surface of the prosthesis also provides low friction to glide the patella, reducing tissue damage and inflammation23.
When placing the prosthesis, it is possible to realign the patella somewhat by moving the prosthesis medially or laterally within the frontal plane. It can also be placed more proximally to prevent patellar luxation, which occurs at the most proximal extent of the trochlear groove, or more distally to prevent luxation occurring at the most distal extent.
Femoral valgus or varus can also be partially compensated for by rotating the prosthesis in the frontal plane. These characteristics of the prosthesis and the variable placement options available may lead to improved patellar coverage and alignment of the quadriceps mechanism when compared to traditional recession trochleoplasty, which may negate the requirement for additional procedures, such as TTT or DFO in some patients with only mild limb deformity23.
However, trochlear groove replacement cannot be expected to compensate for marked bone deformities and additional procedures may well be required to facilitate a return to normal function. This procedure may be performed concurrently with TTT, DFO or treatment of cranial cruciate ligament (CrCL) disease where this occurs concomitantly.
Little data is available regarding follow-up for this procedure, but Dokic et al23 reported on the use of this prosthesis in 35 cases of canine patellar luxation ranging from grade two to four. A total of 11 of the cases in this study had undergone previous surgical procedures, which had failed to yield satisfactory patellar stability. Complications occurred in 6 patients, 3 of which required surgical revision, but complete resolution of lameness was reported in 24 cases at the time of repeat evaluation at 12 weeks postoperatively and in another 7 cases following longer-term evaluation.
Based on these results, it appears use of the trochlear groove replacement has the potential to decrease lameness associated with severe femoropatellar OA and to improve patellar stability. This may represent a valuable addition to the armoury of the small animal orthopaedic surgeon when it comes to treating this sometimes challenging condition. Further studies are required comparing use of the prosthesis to more conventional techniques, such as abrasion trochleoplasty, before these advantages can be stated more definitively.

Another novel option available to assist in treating MPL cases is a patella luxation repair system implant. This implant is used to augment the medial trochlear ridge – hence eliminating the requirement for a traditional trochleoplasty. Similar to the aforementioned trochlear groove replacement implant, in cases with only mild limb deformity, it is suggested the use of the repair system may also eliminate the requirement for TTT. In cases with more severe deformities, the implant can be placed following realignment procedures including TTT and DFO, and has also been used concurrently with CrCL stabilisation.
The repair system is a novel high molecular weight polyethylene implant secured in place using three 2.7mm standard cortical screws. The implant is available in sizes ranging from 1.5cm to 3.5cm, with the 1.5cm implant available as high and low profile. The size required is determined from the “ridgespan” measurement taken from a standard mediolateral radiograph. The implants are appropriate for most sizes of dogs and some cats. The “ridgespan” is measured from the proximal extent of the trochlear ridge to the condylar notch (Figure 2). If the measurement falls between two sizes, the smaller size implant is generally selected.
The surgical approach to place this implant for a case of MPL is via medial parapatellar arthrotomy with the patella reflected laterally. Based on the templating performed, the appropriate size drill guide is used. Different guides are available for the left and right limbs, so care must be taken in selecting the correct one. The guide is placed along the trochlear ridge and the patella temporarily returned to the trochlear groove to assist in assessing placement of the guide.
The most distal hole is drilled first using a 2mm drill bit. This screw is monocortical. Once the hole is drilled the drill bit is replaced with a temporary fixation peg. The length of screw used here is dictated by the size of RidgeStop implant used and ranges from 14mm to 24mm. The most proximal hole is then drilled, again using a 2mm drill bit – this screw is bicortical. Again, a temporary fixation peg is used to maintain drill guide positioning once the drill bit is removed. The remaining hole is then drilled, 2mm and bicortical, and the position maintained using a fixation peg.
At this stage, the distal fixation peg is taken out and the drill guide carefully removed over the two proximal pegs. The implant is then slid over the two proximal pegs and pressed into position on the trochlear ridge. The distal monocortical 2.7mm screw of appropriate length is placed. The most proximal fixation peg is then removed, a depth gauge used to ascertain appropriate screw length and a bicortical 2.7mm screw placed. The final screw is then placed similarly. Care must be taken not to overtighten the screws as the implant is relatively soft and can be deformed by over-tightening. The patella is then replaced into the trochlear groove and stability and stifle range of motion assessed.
Closure is routine, except in some cases it is not possible to close the joint capsule over the implant. In these cases, closure is achieved by suturing the overlying fascia and this has not been associated with complications in the small numbers of cases reported.
In contrast to trochlear groove replacement, the patella luxation repair system may not be applicable for cases with severe femoropatellar OA. It also does not provide the low friction surface for smooth gliding of the patella and hence will not have the postulated advantage of reducing tissue damage and inflammation. Advantages of the system, however, include the simple and rapid nature of the surgery and the fact this procedure is reversible – allowing a return to more traditional techniques should this fail24.
Although a moderate number of cases have been performed using the implant, to the author’s knowledge, only one abstract has been published detailing its follow-up24. This details the use of the implant in 17 cases with follow-up ranging from 1 month to 18 months. Of the 17 dogs, 14 had complete resolution of all clinical signs and one had incomplete resolution.
Three cases had the implant removed subsequently, but details of decision-making for these cases are not included in the abstract. These cases underwent traditional treatment for the MPL following implant removal and went on to make a full recovery. Other complications experienced were minor including seroma formation and mild joint swelling.
Stifle surgery is commonly performed in small animal practice with both CrCL disease and MPL being frequently encountered. How different clinicians manage postoperative pain for these patients varies considerably. Data regarding how long post-surgical pain persists in animals is limited, and certainly varies depending on the surgical procedure performed. The recommended period for analgesic administration postoperatively varies from days to weeks, but expert opinion emphasises the first 72 hours following surgery as critical25.
When patients remain in hospital, analgesia can normally be readily achieved using multimodal analgesia, but options become more limited once patients are discharged. Given most patients are discharged from hospital on the same day, or within 24 hours of stifle surgery, this can result in difficulty maintaining adequate pain control during the first 72 hours.
A bupivacaine liposome injectable suspension represents an advancement in this area. It has long been recognised one of the most effective means of preventing the transduction and transmission of nociceptive signals is through the use of local anaesthetics. However, until recently, the relief that could be provided through their use remained of limited duration, unless some form of wound soak catheter remained in situ. In 2011, the Food and Drug Administration approved an extended-release formulation of bupivacaine for use as a single-dose infiltration into the surgical site to effect post-surgical analgesia in human surgical patients.

The technology used in this product consists of multivesicular liposomes encapsulating aqueous bupivacaine. The liposomes are microscopic structures made of nonconcentric lipid bilayers designed such that bupivacaine is gradually released from the vesicles over a period of 96 hours as the lipid bilayers break down26 providing local analgesia.
A study evaluated the use of a similar bupivacaine liposome injectable suspension, administered via surgical site infiltration, just prior to closure in dogs following lateral retinacular suture placement for treatment of CrCL disease. The treatment was compared to the use of a saline placebo infiltrated similarly.
A total of 46 dogs were followed and results indicated the bupivacaine suspension provided measurable local analgesia over a 72-hour period as assessed by pain scoring, surgical site manipulation scores and necessity for rescue analgesia26. No significant adverse effects were noted26. This product may prove invaluable in maintaining analgesia during the critical first 72 hours post-surgery when patients have been discharged and injectable medications are no longer feasible.
The bupivacaine liposome injectable suspension is administered via a moving-needle injection technique (Figure 3) at a dose of 5.3mg/kg (0.4ml/kg) allowing the suspension to be injected into all tissue layers of the surgical field. This is necessary because the liposomes themselves do not readily diffuse from where they are deposited. As bupivacaine is released from the liposomes, it will diffuse locally into the surrounding tissues, providing up to 72 hours of pain control.
It is only licensed for single-dose administration following CrCL surgery, but it is likely further applications will evolve as more data becomes available; in humans, for example, the use of similar products for peripheral nerve blocks is being investigated. The suspension is licensed for use in the US, but the company also plans to release it in the UK.
The three innovative products discussed in this article all have the potential to advance treatment of commonly encountered stifle conditions in dogs. While trochlear groove replacement and RidgeStop may not be applicable to all cases of MPL, they represent useful options for some more complex cases, potentially allowing superior outcomes to be achieved in these individuals. The bupivacaine liposome injectable suspension signifies a noteworthy development in the field of postoperative analgesia. While the indications for the use of this product are limited, these will likely expand dramatically as more data on its use become available.