12 Sept 2022
Emi Barker BSc(Hons), BVSc(Hons), PhD, PGCertTLHE, DipECVIM-CA, MRCVS explains how coughing diseases are spread and which lessons from the pandemic can be applied to animal care.

Image: © otsphoto / Adobe Stock
Anyone who feared that Bill Gates was trying to monitor us through implants contained within a vaccine has clearly never had to microchip a cat or dog.
The past couple of years have been challenging to many colleagues in first opinion practice, but some positive outcomes have been observed.
Vets frequently use analogies to enhance owner understanding1, and being able to relate issues around pet vaccination to the various debates and issues surrounding COVID-19, and its treatment in humans, could help in enabling owners to appreciate the recommendations vets make.
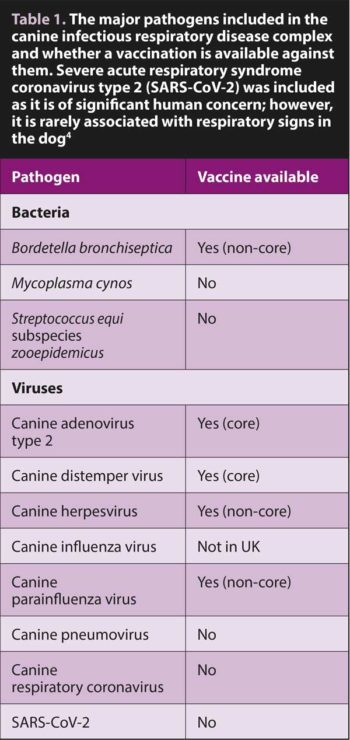
Canine infectious respiratory disease (CIRD) complex is a contagious cause of acute-onset cough in the dog2. Although approximately 75% to 80% of dogs will have Bordetella bronchiseptica as a contributory agent and a third canine parainfluenza virus3, the CIRD complex comprises a wide variety of bacteria and viruses (Table 1) that may occur in isolation or combination. Some members are more pathogenic than others, while the presence of co-infections typically results in a worsening of clinical signs.
In addition, CIRD is not the sole cause of acute cough – with inhalation of foreign material (for example, a tracheal foreign body; aspiration pneumonia), neoplasia, aeroirritants (for example, smoke inhalation), parasitism (for example, angiostrongylosis), and heart disease on the (incomplete) differential list. CIRD complex organisms – particularly B bronchiseptica – also have the potential to cause chronic cough.
Even before the COVID-19 pandemic struck, most cases of acute infectious cough in humans were viral in nature, with causative agents including the common cold viruses (including rhinovirus and human parainfluenza virus) and influenza virus5.
Some cases of cough are bacterial in nature, including infectious with Bordetella pertussis (the causative agent of whooping cough in children), Mycoplasma pneumoniae, Streptococcus pneumoniae and Haemophilus influenzae.
Where co-infections occur, morbidity increases and some of these agents, such as SARS-CoV-2 (the causative agent of COVID-19), also have the potential to cause chronic disease. So, already, many parallels can be seen between acute-onset infectious cough in people and dogs.
Respiratory tract infections are spread between individuals via inhalation of fluid droplets forcefully expelled from the respiratory tract via sneeze or cough, or direct contact. Risk of infection increases as increasing numbers of susceptible individuals come into direct contact with each other or share the same airspace – be that a kennel or dog show, holiday cruise or nightclub, veterinary hospital or care home.
So, while the colloquial name for CIRD is kennel cough, it is not seen exclusively in kennelled dogs, nor the rhinoviruses of freshers’ flu solely seen in first-year university students6.
In people, it is not practical or possible to vaccinate against all the hundreds of viruses and their strains that cause cough; therefore, the focus is on those infections with the potential to cause life-threatening respiratory disease with or without severe extra-respiratory signs (such as meningitis).
 These include vaccines against S pneumoniae, H influenzae type b, influenza and B pertussis. Use of these vaccines is also often restricted to those that are considered at increased risk of infection due to a combination of lack of previous exposure (such as young children), immunocompromise (such as the elderly and immunocompromised), and increased risk of co-infections.
These include vaccines against S pneumoniae, H influenzae type b, influenza and B pertussis. Use of these vaccines is also often restricted to those that are considered at increased risk of infection due to a combination of lack of previous exposure (such as young children), immunocompromise (such as the elderly and immunocompromised), and increased risk of co-infections.
In an equivalent manner, it is not practical or possible to vaccinate all dogs against all causes of CIRD (see Table 1 for vaccine availability). Some vaccines are considered core and are included in the primary vaccine course given to puppies, while others are considered non-core and their use situational7.
Formulation of vaccines is also highly variable, with many distinct types available – each with its own advantages and disadvantages (Table 2).
The high-circulating prevalence of some infectious agents results in regular exposure and “boost” to the immune response of most adults; this can reduce the need to vaccinate against some infectious agents (such as canine parvovirus).
Furthermore, vaccination or infection with some infectious agents results in persistent sterile immunity (infection does not develop following subsequent exposure), while others merely reduce the likelihood of clinical disease and risk of spread to others (infection and transmission can still occur, albeit at a lower frequency).
It should be noted, though, that it is not possible to confirm this persistent immunity without performing serological testing.
Where this immunity is scaled up into a population of animals, a “herd immunity” can develop, which is where enough individuals within a group have protective immunity that limits spread to others.
The percentage of individuals within a population with immunity required to achieve herd immunity depends on the virulence of the infectious agent, and the type of immunity achieved following vaccination or exposure. For some infections, it may never be possible to achieve a level of herd immunity required to protect those most vulnerable from disease.
Examples of all the previous points have been widely discussed over the past 24 months in the context of human health care:
For many, COVID-19 has brought significant morbidity, severe financial hardship and even death. Vaccination against COVID-19 is a now an option that, in common with other vaccinations, is not without inconvenience (including transient pain, fever, and lethargy in most) or expense (including time allocation, travel and taxes). While the overall risk of life-changing consequences is extremely low, the potential for benefit is high – individually and as part of the “herd”.
However, the author appreciates this is easy to say when only relatively positive experiences are had. In the author’s household, the COVID-19 booster vaccination roll-out arrived slightly too late, with her husband developing clinical signs a few days after his booster and herself three weeks before her booster was originally booked.
Fate smiled on them and they only experienced mild clinical signs, and were able to work from home or use up annual leave – likely less fate and more due to having both received the primary vaccine course. The greatest inconvenience was deferment of a long-overdue holiday.
Many dogs with acute cough will have an underlying infectious cause – particularly if they are young – and will have recently mixed with large numbers of other dogs, have had contact with dogs suspected of having CIRD or live in an area of high prevalence of CIRD. However, CIRD is not a single aetiological agent, nor the only differential for acute cough, and careful review of the history (including vaccination status), clinical signs and physical examination is warranted in each case.

As most dogs with CIRD will have mild – if inconvenient – clinical signs, treatment should focus on management of cough rather than the most common underlying bacterial cause; that is, do not reach for the antimicrobials unless extenuating circumstances are present. Consider meloxicam instead – not forgetting the need to isolate the household from other dogs to reduce onwards transmission.
Vaccination is protective against some forms of CIRD and can reduce the morbidity associated with others; it can also mitigate against cost and inconvenience of managing a dog with an infectious disease, so it is recommended – particularly in dogs at increased risk due to their contact with others (such as those due to be kennelled, attend a show or sign up for “doggy day care”).
But, like the author and her husband, vaccines and their boosters need to be given sufficiently in advance of exposure to allow immunity to develop, and selection of vaccine will depend on individual circumstances.
Historically, only live intranasal or intraoral vaccines against B bronchiseptica were available with a rapid onset of action (from 72 hours) and required only a single annual dose. These vaccines were frequently multivalent, including a live-attenuated strain of canine parainfluenza virus in addition. Their use is restricted to immunocompetent dogs and they carry the potential of revision to virulence – especially in immunocompromised in-contact pets and people (that is, their owner or the administering vet).
A subunit vaccine for B bronchiseptica that is administered by SC injection is now commercially available; however, two doses are required in the primary course, the onset of immunity is after two weeks and the first booster is recommended at seven months. Advantages include an absent risk of revision to virulence or potential of transmission to in-contacts; they are also considered safe for use during pregnancy.
The risks and benefits of “off-label” vaccination of dogs with non-pregnancy-associated immunocompromise with inactivated or subunit vaccines requires careful discussion with their owners and, ideally, the manufacturer. Efficacy (the duration of immunity and immune response-generated) would likely be lower than would be anticipated with an immunocompetent dog; however, where vaccination was deemed necessary, their selection would be preferable to a live-attenuated vaccine.
The following points can be taken from what we know:
It has been a while since the author vaccinated any pet other than her own. But for those readers on the front line, the author hopes that increased owner awareness of immune function, vaccination, scientific uncertainty and test accuracy helps you in the daily struggle to relate complex concepts to the benefit of the pets you care for.