29 Jul 2019
Serena Bassolino looks at common complications in anaesthetising patients, assessment of the situation and best course of action.

Image © Chalabala / Adobe Stock
Anaesthetic complications occur frequently, but are rarely fatal. The majority of those can be anticipated, if not avoided, with an accurate assessment of the patient and adequate preoperative stabilisation. Some anaesthetic complications are secondary to the drugs used in the perioperative period, while others are a direct consequence of the patient’s underlying condition. Hypoventilation, hypothermia and hypotension are the most common complications that occur during anaesthetic and, if not treated appropriately, can became emergencies and significantly affect the outcome.
“Anaesthesia is 99% boredom and 1% panic”. This adage tries to capture the idea that, most of the time, anaesthesia is routine and predictable, but when an emergency happens, the progression to a critical state can be rapid and difficult to control.
This article discusses some of the more common anaesthetic complications and how to deal with them. However, two other factors should be considered by all of the clinical team members about to embark on anaesthetising a patient: preanaesthetic assessment of the patient to identify any pathological or physiological abnormalities that may affect the procedure; and preanaesthetic assessment of the environment.
This second aspect, often described as a “pre-flight checklist”, is analogous to a pilot checking the aeroplane (and him or herself) prior to take-off, and should consider elements such as the anaesthetic machine, team members, the planned procedure, predicted adverse events (such as aspiration or haemorrhage) and steps taken to prevent or deal with them1.
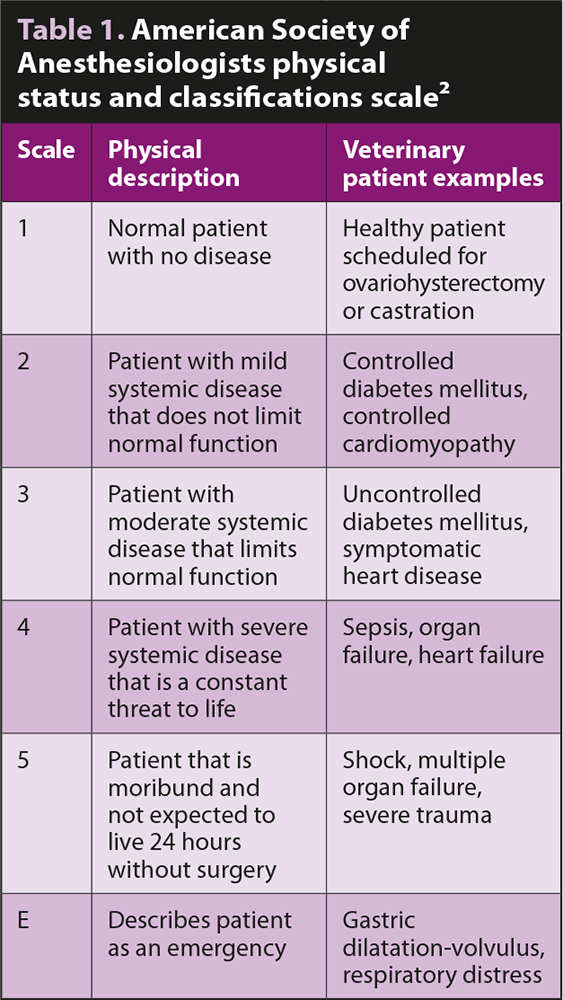
In-depth assessment of patients before anaesthetic is a cornerstone in prevention of any anaesthetic complication. Using the scale developed by the American Society of Anesthesiologists (ASA) is helpful to identify patients at risk. Animals are graded from 1 to 5 – depending on the severity of their disease (Table 1). It has been shown that risk of death during anaesthesia in healthy patients (ASA 1 to 2) was 0.05% for dogs and 0.11% for cats, increasing up to 1.33% for dogs and 1.40% for cats in ill patients (ASA 3 to 5)3.
Even if the death rate is relatively low in our patients, anaesthetic complications occur frequently. In a group of 1,281 dogs, hypoventilation, hypothermia and hypotension occurred in 63%, 53% and 38% of patients respectively4.
The following is a list of the most common anaesthetic complications and emergencies, with some guidance on how to deal with them.
Hypoventilation is defined as an increase in end-tidal CO2 or partial pressure of CO2 (PCO2; above 45mmHg). It is commonly encountered in sedated or anaesthetised patients, as most anaesthetic drugs directly affect the brainstem respiratory centres, causing a degree of respiratory depression5. While mild hypercapnia can be tolerated (permissive hypercapnia), a sustained and significant increase in CO2 should prompt intervention as severe respiratory acidosis can directly depress cardiac and vascular muscle, and can cause arrhythmias and depression of the CNS.
In this case:
Hypoxaemia occurs when arterial partial pressure of oxygen (PaO2) is less than 80mmHg or arterial blood haemoglobin saturation (SaO2) is less than 95%6. If hypoxia is identified, the first thing to do is supplement oxygen via flow by mask, nasal prongs and intubate if needed.
If the patient is already intubated and breathing 100% oxygen (fraction of inspired oxygen [FIO2] 1.0) then:
Hypothermia occurs due to a combination of cold hospital environment and altered patient thermoregulation. While hypothermia protects against ischaemia and hypoxia, a reduction of core body temperature is also associated with vasoconstriction, lactic acidosis, reduced drug metabolism, impaired coagulation and impaired immune system7. Forced air warming systems are an effective means of preserving and increasing body heat in the anaesthetised patient8, while humidification and warming of inhaled gas have been shown to be ineffective as a sole means of maintaining core temperature in companion animals9.
Many factors are associated with the development of hypotension, including most anaesthetic agents, hypovolaemia, haemorrhage, peripheral vasodilation and myocardial dysfunction5. If a patient is hypotensive consider:
Cardiac dysrhythmias can occur as a result of pre-existing medical conditions or as a response to surgery and anaesthesia. Most of them have little clinical significance and do not require treatment; however, if perfusion is compromised, immediate treatment is needed.
When a bradyarrhythmia is identified consider:
If a tachyarrhythmia is present consider:
Hypersensitivity reactions can occur in the peri-anaesthetic period and can be life-threatening. The two most common types are anaphylactic reactions (antigen-immune complex mediated or type 1), which require a previous exposure to the agent, and anaphylactoid reactions, which do not involve IgE and do not require previous sensitisation20. They cannot be clinically distinguished and can be equally dangerous. Hypotension, tachycardia, arrhythmias, pulmonary and portal hypertension, and cutaneous changes can occur.
If suspicion of a severe allergic reaction exists:
Cardiopulmonary arrest (CPA) occurs as a result of the cessation of ventilation and circulation. When CPA is suspected, administration of all anaesthetic drugs should be suspended and drugs previously administered should be reversed. Basic life support needs to be started immediately as any delay significantly reduces the chances of return to spontaneous circulation (ROSC).
Basic life support (BLS) consists of administrating chest compressions and ventilation. The optimal compression rate is 100 to 120 per minute.
Compressions can be performed:
In cases of tension pneumothorax, pleural or pericardial effusions, or significant chest wall/diaphragm injuries, open-chest CPR should be performed.
Airways should be secured with orotracheal intubation and oxygen should be delivered with a FIO2 of 1.0. Optimal ventilation rate is 10 breaths per minute with a tidal volume of 10ml/kg. Compressions should not be stopped during ventilation.
BLS should be administered in two-minute cycles. The operator delivering the compressions should be changed at every cycle to avoid fatigue and ineffective compressions. At the end of every BLS cycle, the team leader should look for signs of ROSC (ECG, pulse, apex beat, increase in end-tidal CO2). Both during ROSC checks and swapping of compressor, delays in administrating chest compressions should be minimised.
Advanced life support includes therapy with vasopressors, positive inotropes and anticholinergics, correction of electrolyte/acid-base disturbances, volume deficits and defibrillation. The two drugs routinely used during cardiopulmonary resuscitation are epinephrine and atropine. Epinephrine is a non-specific adrenergic agonist used for its vasopressor (α1) activity. The initial dose is 0.01mg/kg and it should be administered every three to five minutes (every other BLS cycle). Atropine is a parasympathetic antagonist. The literature has not shown beneficial or detrimental effect of its use at standard dosing (0.04mg/kg) during CPR. Its action lasts up to 20 minutes.
During CPR, minimum monitoring includes ECG and capnography. ECG is needed to recognise “shockable” rhythms (ventricular fibrillation and pulseless ventricular tachycardia), while capnography is useful to assess the quality of CPR: an end-tidal CO2 above 15mmHg in dogs and 20mmHg in cats is associated with effective CPR and an increased rate of ROSC.
Consensus guidelines, printable CPR algorithms and CPR drug charts can be found in the open access Reassessment Campaign on Veterinary Resuscitation guidelines21.