22 Jan 2018
Sarah Caney describes approaches to successfully managing two common conditions in older cats at the same time.

The assessment of renal function in cats with hyperthyroidism can be difficult – for example, polyuria/polydipsia and a reduction in urine specific gravity can be encountered with both conditions.
Hyperthyroidism and chronic kidney disease (CKD) are common conditions in older cats – hyperthyroidism is estimated to affect around 10%, whereas CKD is thought to affect more than 30%. Unsurprisingly, therefore, it is not unusual for older cats to suffer from both conditions concurrently. The presence of CKD can make diagnosis and management of hyperthyroidism more complicated. Optimum treatment of hyperthyroidism is desirable, where possible, since it is damaging to renal function and can contribute to progression of disease. With appropriate care it is generally possible to successfully manage cats with both CKD and hyperthyroidism.
Published studies have indicated around 10% to 20% of cats diagnosed with hyperthyroidism have evidence of pre-existing chronic kidney disease (CKD) on first assessment of their thyroid disease.
Whether a causal relationship exists between hyperthyroidism and CKD, or whether both conditions simply occur in concert, is not known because they are both common conditions in the older individual. Prevalence studies generally indicate around 10% and more than 30% of older cats suffer from hyperthyroidism or CKD, respectively.
Increasing evidence suggests hyperthyroidism causes damage to the kidneys, which may contribute towards long-term development of CKD through several mechanisms. These include tubulointerstitial damage, fibrosis, glomerular hypertension and chronic interstitial nephritis caused by an increase in angiotensin II. Evidence of renal damage is supported by the presence of proteinuria and increased levels of a number of urinary markers of tubular damage, such as retinol-binding protein in cats suffering from hyperthyroidism. The renal damage may be reversible, since levels of these markers are documented to reduce following achievement of euthyroidism.
Presence of hyperthyroidism can mask or hide reduced renal function, since the hyperthyroid state increases renal blood flow and glomerular filtration rate (GFR). This can make diagnosis of CKD difficult in cats suffering from hyperthyroidism.
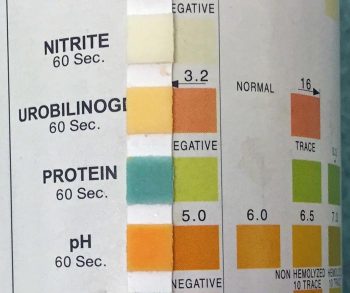
Evaluation of blood and urine samples is important in the assessment of both hyperthyroid and CKD patients. It is not only valuable in diagnosing these conditions, but also in assessing severity and looking for the presence of additional illnesses. Unfortunately, in the case of cats with concurrent hyperthyroidism and CKD, interpretation of laboratory tests becomes especially challenging. A true assessment of renal status is only possible following assessment of biochemistry and urinalysis once euthyroidism has been achieved.
The presence of CKD makes diagnosis of hyperthyroidism problematic because of the suppression of thyroid hormones — the so-called sick euthyroid syndrome. Therefore, in cats with clinical signs compatible with hyperthyroidism, a normal total thyroxine (T4) should not be taken as evidence the cat does not have this condition. Further tests, such as a free T4 assay, may be helpful in diagnosing hyperthyroidism in a cat with concurrent CKD.
The presence of CKD can affect serum biochemistry and haematology results. Laboratory consequences of hyperthyroidism, such as erythrocytosis, occasionally seen in hyperthyroid cats, may be masked by anaemia associated with CKD.
Identifying the presence and quantifying the severity of renal disease in a hyperthyroid cat is difficult. Traditionally, a diagnosis of CKD is made in patients with compatible history and clinical signs, in addition to persistent azotaemia (elevated urea and/or creatinine) and a reduced urine specific gravity (USG; <1.035). More recently, assessment of symmetric dimethylarginine (SDMA), a serum biomarker that is renally excreted, has been shown to be helpful in assessing renal function, as discussed later.
If azotaemia and reduced USG are documented in a cat with hyperthyroidism, then pre-existing CKD is confirmed. The extent of CKD is likely to be underestimated due to the impact hyperthyroidism has on GFR and, hence, serum creatinine levels.
Clinicians should bear in mind concentrations of urea and creatinine are affected by extra-renal factors, and by hyperthyroidism. For example, urea tends to be high in hyperthyroid cats as a consequence of polyphagia (hence increased protein intake), and this may falsely increase the concern a hyperthyroid cat has CKD. Conversely, creatinine concentrations tend to be misleadingly low, because hyperthyroid cats are thin and have very little muscle mass (creatinine being derived from muscle turnover). The increased GFR present in hyperthyroid cats tends to reduce blood levels of both urea and creatinine.
Assessment of GFR – considered to be the best assessment of renal function – is possible from clinical practice, although this remains an expensive test. Since 2015, inexpensive assays for SDMA have been available for the assessment of renal function. Studies indicate SDMA assessment may be more sensitive than serum creatinine in diagnosing early CKD (Hall et al, 2014). Unlike serum creatinine, SDMA levels are not affected by muscle mass and, therefore, may be more reliable in assessing renal function in a poorly muscled cat suffering from hyperthyroidism. At present, no published data exists regarding the usefulness of SDMA assessment in diagnosing occult renal disease in non-azotaemic patients with hyperthyroidism.
Assessment of USG is usually helpful to define renal function, but this too can be affected by hyperthyroidism. A healthy USG is generally considered to be greater than 1.035, with concentrations fewer than 1.035 taken as one of the indications of kidney disease. However, in hyperthyroid cats, the ability to produce concentrated urine is compromised, and a USG below this figure can be obtained from cats that have healthy kidneys. Additionally, this healthy value varies with the type of diet fed. Cats fed strictly dry food should concentrate urine to greater than 1.045.
Mild proteinuria is a common finding in hyperthyroid cats and is thought to occur as a consequence of glomerular hypertension and hyperfiltration associated with the hyperthyroid state. The prognostic significance of proteinuria in hyperthyroidism is unknown, but it does tend to resolve with treatment, even in cats that develop azotaemia.
Both hyperthyroidism and CKD are conditions associated with a higher incidence of urinary tract infection (UTI). For example, one study showed 12% of hyperthyroid cats suffered from UTIs. Unfortunately, most of these suffer from clinically silent urinary infections and may only show vague clinical signs, such as weight loss and lethargy.
Treatment of clinically asymptomatic bacterial UTI is controversial; treatment should be prioritised for those patients showing systemic or lower urinary tract signs, where there is an active urinary sediment or where concurrent pyelonephritis is suspected (Sparkes et al, 2016).
Treatment goals are to reverse clinical signs and, if possible, reduce total T4 levels to the lower half of the reference range. All treatments for hyperthyroidism have the potential to worsen kidney function. This is because the hyperthyroid condition increases renal blood flow and GFR. When the hyperthyroidism is treated, the increased cardiac output and renal blood flow to the kidneys decreases. This results in a decrease in GFR by up to 50% of the pretreatment level.
For many hyperthyroid cats, this return to normality is not associated with kidney problems. However, in a proportion of patients, this reduction in blood flow has the potential to unmask kidney disease not previously recognised, allowing the pre-existing kidney disease to manifest itself clinically. In those cats in which renal disease has been documented before treatment is started, treatment has the potential to worsen renal function and may precipitate a crisis. Significant decreases in renal function are generally evident by four weeks post-treatment, after which time GFR stabilises with very little deterioration, depending on the degree or stage of renal disease.
Azotaemia develops after achievement of euthyroidism in around 15% to 25% of patients. However, so far, a number of studies have shown it is not possible to predict accurately which patients will reveal CKD following treatment of hyperthyroidism. These studies have evaluated pretreatment laboratory variables, such as serum biochemistry, USG, proteinuria, and haematology.
In general, no significant differences have been seen when comparing the pretreatment parameters in cats that developed a post-treatment renal azotaemia with those that did not. Although USG is reduced in cats with CKD, it also can be reduced as a consequence of hyperthyroidism, so analysis of this parameter alone is not sufficient to be helpful. Equally, although a pretreatment USG of greater than 1.035 is often reassuring, it cannot be viewed as a guarantee the cat will not develop a post-treatment renal azotaemia. The fact some cats with primary renal azotaemia remain able to concentrate urine to 1.045 or greater complicates the interpretation further.
At the time of writing, no published data exists supporting the use of SDMA assessment in predicting which hyperthyroid cats will suffer a clinically significant deterioration in renal function following achievement of euthyroidism.
GFR is reported of some value in predicting post-treatment renal azotaemia. One study reported some value in using a combination of pretreatment GFR, USG and total T4 in predicting which patients developed a post-treatment renal azotaemia. In the same study, a significant difference was found in pretreatment GFR and USG in cats that eventually developed post-treatment renal azotaemia.
Unfortunately, while being commercially available to many clinicians, assessment of GFR via an iohexol clearance assay is very expensive, limiting its usefulness. Where used, it may help predict the likelihood of post-treatment renal azotaemia: patients with low or low/normal GFRs are likely to be most vulnerable to a clinically significant deterioration in their renal function. The usefulness of other markers of renal function, such as the urinary N-acetyl-beta-D-glucosaminidase to urinary creatinine ratio (NAG index) and urinary retinol binding protein, are still being evaluated.
Many clinicians prefer to treat hyperthyroid cats with a reversible treatment (antithyroid medication or iodine-restricted food) in the first instance. The main advantage of this approach is it is reversible. In other words, if renal function deteriorates, the treatment for hyperthyroidism can be reduced or discontinued to help stabilise the patient. Medical treatment of hyperthyroidism induces euthyroidism more gradually than surgical thyroidectomy or radioiodine therapy – both of which may result in an acute destabilisation of a patient.
In cats whose renal function remains stable on medical treatment, permanent treatment of their hyperthyroidism can be considered with a greater degree of confidence. Although no definite guidelines exist, it is probably advisable to monitor patients on medical treatment for at least one month, possibly longer, after euthyroidism has been achieved before a decision is made to elect for more permanent, curative treatments. This recommendation is based on the finding GFR stabilises by one month following achievement of euthyroidism. This approach is probably unduly cautious for cats suffering from hyperthyroidism and where serum creatinine is ≤250µmol/L pre-treatment, since optimal treatment of hyperthyroidism is highly desirable to minimise hyperthyroidism-associated renal damage.
If a cat is known to have CKD before medical treatment for hyperthyroidism is started, and especially if in IRIS stage 3 or 4 CKD (serum creatinine is >250µmol/L), it is advisable to start treatment with a lower dose of medication initially, while monitoring the renal values closely. For example, if using thiamazole, a starting dose of 1.25mg every 12 to 24 hours should be considered. If any problems are seen then the thiamazole dose can be lowered or the treatment may be discontinued. If, conversely, medication is not associated with renal or other adverse effects, the dose can be titrated to induce and maintain euthyroidism.
Frequent and regular re-evaluations are essential to facilitate optimal management of both CKD and hyperthyroidism. Assessment of renal parameters is recommended at two to three and four to six weeks following the start of treatment, or after changing the dose of antithyroid medication.
Ongoing management of patients with CKD and hyperthyroidism requires attention to both conditions. IRIS guidelines (2016) should be followed with respect to staging and management of CKD, and any complications present as a result of this. Where possible, attempts should be made to induce and maintain euthyroidism as discussed already.
In those patients where euthyroidism is associated with a clinical and biochemical worsening of renal disease, it may be necessary to titrate therapy to achieve the best balance possible. The individual priorities of each patient need to be considered to determine which therapy and approach is most appropriate. For example, in some patients, suboptimal control of the hyperthyroidism may be tolerated clinically, whereas euthyroidism may be associated with severe renal dysfunction and a clinical crisis.
Care should be taken to avoid iatrogenic hypothyroidism (IH), since this is known to increase the likelihood of renal complications and worsen patients’ survival times.
In patients receiving antithyroid medication, the dose can be titrated to prevent iatrogenic hypothyroidism. To the author’s knowledge, IH has not been confirmed in a patient receiving an iodine-restricted food as sole management for hyperthyroidism, although one cat was reported to have a transiently subnormal T4.
If seen, a change in diet would be indicated. Patients that have received curative treatment for their hyperthyroidism should have their T4 and renal parameters monitored following treatment to assess treatment success and look for evidence of IH. If a subnormal T4 is reported and azotaemia is present or worsened following treatment, consideration should be given to assess the patient for presence of IH through measurement of free T4 and endogenous thyroid-stimulating hormone (TSH), performing a thyrotropin stimulation test or scintigraphy.
TSH levels are typically >0.5ng/ml in patients with IH. Restoring euthyroidism may be of benefit in improving renal function in those cats suffering from transient or permanent IH.
Treatment success should be gauged on clinical response to treatment, as well as assessment of laboratory parameters. Accurate assessment of bodyweight and body condition score is vital, in addition to a thorough history, general clinical examination, and blood pressure measurement. Fortunately, in many cats, it is possible to achieve a balance between these two conditions and gain a good treatment outcome.
The prognosis for cats with azotaemic CKD evident at the time of their diagnosis of hyperthyroidism is of poor survival (median six months); however, the survival of euthyroid cats developing azotaemia post-treatment for their hyperthyroidism may not be any different to those remaining non-azotaemic (Williams et al, 2010).