17 Apr 2017
Isuru Gajanayake discusses the changes to nutritional requirements that should be considered in older canine and feline patients.

Nutrition has always played a key role in managing animals undergoing physiological stresses (such as growth and reproduction) and during disease states. Senescence should be considered a physiological state requiring specific attention.
With improving veterinary care, many dogs and cats are living longer and, as a direct consequence, the proportion of senior dogs and cats in the general pet population is increasing. In addition to this, many of these older animals are living with chronic medical conditions due to the earlier detection and improved management of such disorders.
The pet-owning public is often keen to use nutrition to optimise the health and longevity of their senior pets. To meet these client expectations, the vet must be able to:
Gain of excessive body fat is common with increasing age in dogs and cats. This may be due to the reduced metabolic energy demand after neutering that is not compensated by a reduced food intake. In addition, reduced physical activity and exercise with age (for example, due to the development of conditions such as OA) may also contribute to weight gain.
Increased body fat is particularly concerning because longitudinal studies have demonstrated excessive body condition to be associated with a shorter lifespan in dogs (Kealy et al, 2002).
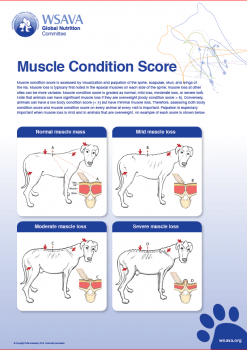
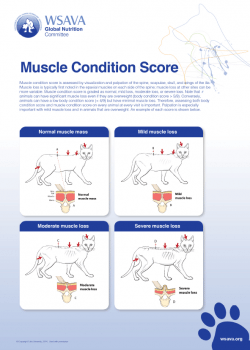
Loss of lean body mass (muscle) is common in elderly people. Termed sarcopenia, this phenomenon is thought to lead to decreased muscle strength with subsequent physical disability, poor quality of life and even death (Freeman, 2012). This form of muscle wasting occurs in the absence of illness, whereas cachexia is the form of muscle wasting associated with disease states (for example, cancer, heart failure and renal disease).
Evidence exists ageing dogs and cats are affected by sarcopenia. For example, healthy geriatric cats are reported to have one-third less muscle mass compared to young cats (Laflamme and Gunn-Moore, 2014).
Although age-related changes are seen on histopathology of certain digestive organs (such as salivary glands, liver, small intestine and pancreas) of elderly dogs, these changes are typically not severe, and nutrient digestion and absorption do not appear to be affected (Larsen and Farcas, 2014).
In contrast, cats appear to have reduced digestibility of protein, fat and carbohydrate with increasing age. In particular, one-third of geriatric cats appear to have reduced ability to digest fat and one-fifth of aged cats have reduced ability to digest protein (Perez-Camargo, 2004). This is likely to have implications on the amount and digestibility of dietary protein and fat provided to elderly cats.
Reduced renal function is often assumed in many elderly dogs and cats; however, because a large reserve of renal functional capacity exists, minor loss of renal function is usually well compensated. Other age-related changes that may affect appetite and food consumption in geriatric animals include reduced senses of taste and olfaction, decreased sensitivity to thirst, and cognitive dysfunction syndrome.
No single diet is suitable for all senior patients. For this reason, every individual elderly cat and dog must undergo a basic nutritional evaluation to formulate a nutrition plan.
This includes consideration of the animal’s previous diet history, its appetite and presence of clinical signs of illness (such as vomiting, diarrhoea, polydipsia, polyuria and weight loss). Laboratory testing, such as complete blood count, serum biochemistry, urinalysis and serum thyroxine in cats, may also be necessary to check for presence of diseases where clinical signs of such disorders exist.
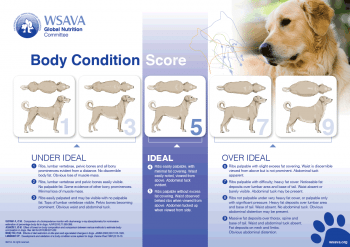
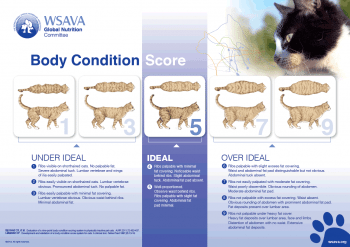
Physical examination of the senior dog and cat should include both body condition and muscle condition scoring to assess the patient for obesity and sarcopenia, respectively. A historical record of the animal’s bodyweight can also provide useful information about its health. In clinical practice, body energy stores are most reliably assessed and graded by using a body condition scoring system (Figure 1). Because different scoring systems have been described, senior pets should be scored using a single system for consistency.
Similar to the body condition scoring systems used for assessing adipose stores, a qualitative assessment of the senior dog or cat’s muscle mass should also be performed by using a muscle condition scoring system (Figure 2).
Because obese animals can display – and mask – muscle wasting, both fat and muscle condition scores should be performed in all elderly animals. The WSAVA nutrition tool kit provides useful information and guidelines for nutritional assessment of dogs and cats (www.wsava.org/nutrition-toolkit).
The energy requirements of an individual cat or dog will depend on many factors, including – arguably most importantly – its energy (adipose) stores. The energy requirements of most healthy dogs and cats decrease after neutering as they mature (Harper, 1998). If this reduced energy requirement is not compensated by a decreased calorie provision, excessive gain of body fat ensues.
Following the reduced energy needs noted with maturity, somewhat surprisingly, the energy needs of geriatric cats increases after 13 years of age (Perez-Camargo, 2004). This higher energy requirement in senior cats may be due to reduced digestive efficiency – especially as elderly cats have a reduced ability to digest fat (the most energy dense of the three macronutrients). Thus, an individual senior animal’s energy provision will be dependent on its species, age, activity levels and energy (body fat) stores.
Otherwise healthy senior cats and dogs require a high dietary protein provision to counteract an age-related decrease in protein synthesis and increase in nitrogen excretion (Laflamme, 2005). As aforementioned, sarcopenia is likely to affect senior cats and dogs, and a protein replete diet may prevent or help address this age-related metabolic complication.
In addition to this, some diseases associated with ageing, such as feline hyperthyroidism, can lead to significant muscle wasting, which does not necessarily normalise with treatment of the disorder (Peterson et al, 2016).
Protein intolerance, due to hepatic or renal functional impairment, may be present in senior dogs and cats due to diseases such as chronic hepatitis and chronic kidney disease. However, genuine indications for protein restriction should be confirmed via laboratory testing rather than merely assumed, because unnecessary protein restriction is likely to be detrimental in the long term.
Senior cats and dogs may require increased dietary fat provisions to maximise their energy intakes, because fat is more energy dense compared to carbohydrate and protein. An energy-dense diet may be especially useful in situations where food consumption is reduced for reasons such as cognitive dysfunction. In addition, senior cats may require a higher dietary fat provision compared to younger cats, to counteract age-related fat maldigestion.
The vitamin and mineral requirements of senior dogs and cats are likely to be similar to adult maintenance requirements, unless the presence of specific diseases mandates nutrient modulations (for example, phosphorus restriction for chronic kidney disease or sodium restriction for congestive heart failure).
Antioxidants – including lipoic acid, vitamin E and glutathione – may help minimise age-related decline in brain function (Rhodebush et al, 2005). Similarly, dietary supplementation with long-chain omega-3 fatty acids may also help with canine cognitive dysfunction and OA (Moreau et al, 2013).
Based on the aforementioned information, the specific requirements of an individual cat or dog can be evaluated, taking into consideration its:
A plethora of diets marketed for senior dogs and cats are available. Some of these diets are marketed for specific sub-categories within senior pets, such as diets based on:
Selecting an appropriate diet should primarily take into account specific nutrient needs of a patient, based on its nutritional assessment. Where a therapeutic diet is indicated to manage a confirmed medical condition, this would generally take precedence over age-related nutrient modulations. In some cases, a balanced, home-cooked diet may be useful to feed an elderly dog or cat – especially if no suitable commercial diet meets a patient’s specific nutrient needs, or poor consumption of commercial diets occurs due to habit or inappetence.
It is essential any home-cooked diet is formulated to be balanced – that is, to provide all essential nutrients in the correct amounts. Dietary supplements, such as omega-3 fatty acids, can be helpful to manage age-related cognitive dysfunction and OA. These can be provided in food or as a separate supplement.
As with the implementation of any feeding plan, monitoring of its effectiveness and appropriate adjustment of the plan is necessary. This must include regular physical examinations to check bodyweight, body condition score and muscle condition scores. Monitoring of clinical or subclinical organ dysfunction with laboratory or other tests may also be necessary.
Senior dogs and cats are at risk of body conformational changes, including excessive body fat and muscle wasting (sarcopenia). Energy requirements generally decline with age; however, geriatric cats have increased energy needs. Dietary protein may help minimise sarcopenia, so should only be restricted if genuinely indicated (such as for chronic kidney disease).
Supplements can help modulate age-related organ dysfunction (of the brain, for example) or age-associated disease such as joints. Nutritional assessment of each senior cat and dog allows formulation of an appropriate diet and feeding plan, and presence of disease in elderly cats and dogs should be confirmed by laboratory testing, rather than assumed.