28 Jan 2019
Darren Barnes discusses the investigation and management of these cases in companion animals – as well as indications for surgical intervention – and outlines post-treatment care.

Thoracic trauma is common in small animals. They vary dramatically in aetiology – from blunt trauma to impalement and bite wounds – and, subsequently, are associated with varied pathologies requiring tailored treatments.
Cases are challenging to manage, as many organs and body systems may be involved. They require a systematic approach to triage, coupled carefully alongside diagnostic evaluation. Many cases can be stabilised by appropriate medical therapy and thoracic drainage.
Surgical exploration of the thorax is generally not advocated in cases of blunt trauma, except in cases with profuse or continued haemorrhage or organ rupture. It is more commonly recommended in patients impaled on foreign objects that may leave residue within the thorax, and for bite wounds to allow thorough debridement of traumatised tissue.
Thoracic trauma is common in small animal patients.

The nature of the trauma varies – from blunt, contusive injuries associated with vehicle collisions or falls from a height; to sharp, penetrating injuries associated with impalement injuries and gunshot wounds; to bite wounds with crushing and tearing of the deeper tissues.
These very different aetiologies result in different patterns of injury that, subsequently, require differing approaches to their investigation and management. Likewise, the severity of injury determines the suitability and requirement of a patient for surgical exploration. Therefore, each case must be assessed and treated individually, rather than applying a standardised algorithmic approach.
Blunt trauma to the thoracic wall frequently results in diaphragmatic rupture and/or intrathoracic organ trauma1, including pulmonary contusions. However, injury to the thoracic wall is infrequent due to its compliance in small animal species2. Where rib fractures are observed, even when not causing a clinical dysfunction, vets should be aware of a strong association with more serious intrathoracic soft tissue injury.
Penetrating injuries to the thorax are also frequently associated with intrathoracic pathology. One study reported 69% of impalement injuries to the trunk resulted in thoracic penetration, with more than a third of those cases having residual foreign material removed from the wound at surgery3.
Bite wounds are commonly seen with large dogs attacking smaller dogs or cats. The characteristic of these injuries is that the externally visible puncture wound is the tip of the iceberg, with extensive deeper crushing, tearing and avulsion injury to the tissues of the thoracic wall, and possibly to intrathoracic structures. Bite wounds are the most common trauma resulting in dogs and cats requiring emergency thoracic surgery4,5.
Immediately on presentation, patients suffering thoracic trauma are often dyspnoeic and show signs of shock. Therefore, examination may be very limited to allow oxygen supplementation.
As possible thereafter, in order of priority for the specific patient:

Trauma scoring systems have been developed in humans to help better predict prognosis. The animal trauma triage score (ATT) was established for cats and dogs in 1994 to assign a score based on evaluation of cardiac function, perfusion, respiratory function, eye, muscle and integument disease, skeletal injury, and neurological abnormalities6.
Future study of these scoring systems may help identify patients in which specific therapeutic interventions may be beneficial; however, for now their use is limited to prognostication.
Thoracic-focused ultrasonographic assessment has been shown to be highly sensitive and specific in the acute setting for diagnosis of pneumothorax – and other intrathoracic injury – without the need for chemical restraint or anaesthesia7, although is highly operator-dependent.
The specifics of ultrasound assessment are beyond the scope of this article, but assessment may be performed at the bedside while performing other assessments and continuing oxygen therapy. Assessment also allows for guided thoracentesis for therapeutic drainage, as well as sampling for laboratory interpretation of pleural fluid.
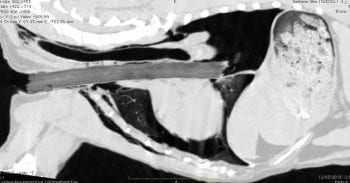
Once the patient has been stabilised, CT or radiography may be performed to make a more global evaluation of the thoracic cavity (Figure 1). It should be noted, for these modalities, sensitivity for identifying wood from impalement injuries is low due to its low radiopacity3,8. The author advocates the use of CT for global screening of the extent of the injury (Figures 2 and 3) and for planning surgical intervention, in combination with directed ultrasound, to aid assessment of soft tissue injuries and increase detection of retained foreign material in the case of impalement injuries.
Acute analgesia for thoracostomy tube placement, or at the time of surgical intervention, may be easily administered by means of paraspinal intervertebral nerve blocks using levobupivacaine.
Thereafter, further analgesia may be administered – in the form of NSAIDs – in cardiovascularly stable patients following volume resuscitation and renal parameter assessment.
Intrathoracic administration of levobupivacaine every six to eight hours may be beneficial following thoracic drainage, and the analgesic may provide best analgesia to the dependent surfaces in the thorax and, therefore, be of most benefit in patients with trauma involving the sternum, or following median sternotomy for thoracic exploration.

Following diagnostic imaging, further thoracic drainage may be performed by either blind or ultrasound-guided needle drainage using a butterfly needle, extension set, syringe and three-way tap, or – for larger-volume effusions – by placing thoracostomy drains.
The author prefers to use relatively narrow-bore, Seldinger-type thoracostomy drains with multiple fenestrations for drainage of haemorrhagic effusions and/or air, as is common with traumatic thoracic injury.
Care should be taken to place the drains through a skin incision over the 9th to 11th ribs – and the skin undermined to enter the thorax at least two to three intervertebral spaces more cranially – to allow a seal around the tube to prevent air leakage.
With thoracostomy tubes in place – unilaterally or bilaterally, as dictated by the specific case requirements – respiratory rate and effort should initially be monitored constantly then hourly once stable. The thorax is drained hourly, also initially, and more often as dictated by changes in respiratory rate and effort. In cases where pneumothorax reforms rapidly, it may be necessary to seal open thoracic wounds with occlusive dressings, and/or use one-way Heimlich valves or a continuous digital closed drainage system that may also allow quantitative assessment of ongoing drainage.
Indications for surgical intervention can be controversial. Thoracic surgical exploration in the acute setting is associated with extremely high incidence of mortality in humans9, so needs careful consideration. Human patients stabilised to undergo thoracotomy in an operating theatre have a much better prognosis than those undergoing emergency thoracotomy in accident and emergency, although this finding is likely biased by more stable patients with less severe injuries being taken to theatre9.

Penetrating trauma to the thorax is generally accepted as an indication for thoracic exploration; however, surgery is not frequently indicated following blunt thoracic trauma9. Publications have investigated the mortality rate and risk factors for emergency thoracic surgery in dogs and cats, and showed much more promising results4,5 – likely, in part at least, influenced by the difference in pathogenesis and pattern of injury between human and small animal patients.
Indications for thoracic cavity exploration include persistent or life-threatening haemorrhage, pneumothorax that does not resolve with conservative management, and clinical suspicion of retained foreign material that may be apparent on diagnostic evaluation. Thoracic wall exploration is recommended for dogs suffering thoracic bite wounds, for debridement of devitalised tissue. Surgeons should be prepared and equipped for subsequent exploration of the thoracic cavity in patients with extension of wounds full-thickness through the thoracic wall, or in cases with more than three thoracic radiographic lesions – for example, rib fracture, pneumothorax, pleural effusion and pulmonary contusion)10-12. Surgeons should also be prepared to perform lung lobectomy and pericardiectomy among other intrathoracic procedures, if necessary, following full surgical exploration.
The thoracic wall requires airtight closure in cases where the pleural space meets air from the outside world. This may be achieved by forming a seal with primary repair of the traumatised tissues, but, with extensive debridement, may also require additional wound closure techniques, such as the use of muscle flaps – for example, latissimus dorsi or rectus abdominis muscles – or with meshes:
Negative pressure wound therapy has been reported in a small number of humans and one dog, using polyurethane foam covered with an occlusive dressing and negative pressures of -100mmHg to -125mmHg applied until the wound is covered by a healthy bed of granulation tissue prior to delayed primary wound closure13-15. Adequate surgical debridement is essential prior to dressing placement13.
The advantages of this technique are the lower intensity of dressing management, with dressings only required every two to three days, and a closed system allowing restoration of negative pleural pressure. The acceleration of wound healing is thought to be multifactorial, but includes removal of third-space fluid and debris from the wound, improved microvascular tissue perfusion, decreased bacterial colonisation, removal of inhibitory wound healing factors, and the mechanical response of surrounding tissues to controlled force15.

Minimal displacement of a low number of rib fractures invariably does not require surgical stabilisation – and may be managed conservatively with analgesics and, in certain circumstances, bandages – although it is imperative these do not adversely impact respiratory function. Large flail segments can often appear dramatic, but even these need to only undergo surgical stabilisation if associated with hypoventilation.
A retrospective case series found no significant difference in outcome between cases managed conservatively and surgically; however, a bias may have existed to managing more clinically significant lesions surgically16.
Fractured ribs may be stabilised by suturing to adjacent ribs with encircling sutures, or interfragmentary or intramedullary wiring16. Multiple adjacent fractured ribs may be sutured in an alternating, overlapping “basket-weave” fashion12,17.Alternatively, ribs may be sutured with non-absorbable material to an external splint affixed, in turn, to at least one intact rib cranial and caudal to the flail segment. Such an external brace should be maintained for about two weeks to allow adequate stability to be achieved by scar tissue.
Sternal defects may also appear dramatic, but, once again, only require surgical intervention if accompanied by intractable hypoventilation. Sternebrae may, similarly, be stabilised by external bracing, as described for flail segment splinting or by intersegmental bone plating18; or anecdotally by the author, by intramedullary pinning between adjacent sternebrae, as shown in Figure 4.

The surgical approach to thoracic exploration will be dictated by the location of the surface wound and the intrathoracic region in need of evaluation. Intercostal thoracotomy allows rapid access in emergency settings using simple instrumentation, as well as simpler access to the hilus of the lung on the operated side with an appropriately positioned (fourth to sixth intercostal) thoracotomy.
Median sternotomy allows for more thorough evaluation of both hemithoraces, but is more challenging to perform and requires additional instrumentation.
Thoracoscopy allows for very limited intrathoracic evaluation, so may be most useful as an additional diagnostic tool for intrathoracic evaluation that may then require an open surgical approach, except for more minimal interventions.
Coeliotomy may be appropriate for selected cases – such as those where thoracic trauma is limited to the diaphragm – although the approach may be extended through a median sternotomy incision, if indicated, following an initial surgical evaluation.
Following treatment of thoracic trauma, patients should be monitored in the intensive care setting, as changes in clinical status can be rapid and require regular reassessment for immediate intervention. As time passes following intervention, gradually support with analgesia, IV fluid therapy and oxygen administration weaned based on continued reassessments.
Frequency of thoracic drainage can be reduced with decreasing drain production prior to drain removal, with resolution of pneumothorax and reduction of fluid drainage to serosanguinous fluid at a level anticipated by the presence of the drain (loosely in the region of 2ml/kg/day).
Increasing fluid production, or presence of fluid of a different nature, warrants cytological interpretation, and possibly culture and sensitivity testing. Hospital stays may be protracted in cases following severe thoracic trauma3.
Antibiotic therapy should be broad-spectrum in nature following initial sampling of thoracic effusions, or biopsy of devitalised tissue or foreign material at the time of surgical debridement, and thereafter based on culture and sensitivity findings. The duration of treatment will depend on the extent and type of trauma, and presence of retained foreign material or surgical implants.
Thoracic trauma cases are challenging to manage as many organs and body systems may be involved. Patients frequently have additional non-thoracic injuries due to the nature of the inciting causes of thoracic trauma. Therefore, cases often benefit from multidisciplinary management, but can have excellent outcomes with a targeted approach, including surgical management if appropriate.